Abstract
Recurrent cecocolic torsion may cause recurrent right lower abdominal pain and right-sided thrust dyspareunia. It is seldom considered in the differential diagnosis of pain in this region. The propensity of the cecocolon to torse is secondary to the double developmental defect of a mobile cecocolon compounded by an elongated and overrotated organ that can be eccentrically located in the abdomen. The torsion may result in recurrent obstructions with spontaneous resolutions, but it may proceed to an acute episode of obstruction and strangulation with a more profound morbidity and mortality rate. The diagnosis of recurrent cecocolic torsion is verified by a plain x-ray film of the abdomen, contrast enema, and computed tomography scan. The preferred treatment is outpatient laparoscopic cecocolopexy. Laparoscopic or classical open cecocolectomy and right hemicolectomy are reserved for more complex and morbid presentations.
Keywords: Cecocolon, Torsion, Introrsion, Intussusception, Mesocecocolon, Cecocolopexy
INTRODUCTION
Recurrent cecocolic torsion may present as an acute pain in the right lower abdominal quadrant or more frequently as chronic and recurring episodes of pain of varying intensity and morbidity. In females, it may be associated with thrust dyspareunia.1 As a diagnostic entity, it is unfamiliar to many practitioners. Generally, at the time of diagnosis, it has already proceeded to become a cecocolic obstruction.
The cecocolon is predisposed to torsion because of 2 developmental abnormalities; namely, an incomplete fixation to the right iliac fossa and an associated elongated, overrotated, or eccentrically located cecocolon. More than 1000 cases were documented between 1941 and 19842–5 and more since then, yet the average practitioner is not conversant with this diagnosis.
With the awareness to this entity during occurrences of pain in the right lower abdomen, the clinician can diagnose or rule out this condition with specific radiological tests and institute the recommended surgical treatment before it can proceed to obstruction-strangulation.
EMBRYOLOGY
The developmental rotation of the colon is expected to be completed at the eighth month of gestation after the cecum has migrated in the right iliac fossa and cecocolic fixation by the mesocecocolon has occurred in the right paracolic gutter, and the right iliac fossa is expected to be completed 4 months after birth.6–9
An agenesia of the mesocecocolon for a variable length will leave the cecocolon freely mobile. The cecocolon may become redundant by elongation and overrotation.4,7,9 It can lie freely mobile anywhere in the abdominal cavity. This double developmental defect will pre-dispose the cecocolon to kinking, torsion, and introrsion.
A funicular Jackson's membrane10 acting as a fulcrum is a potential for a cecal bascule.1,11–14 A funicular parietocolic band8,12,15 may also cause cecocolic torsion at the level of the ascending colon.8,11–14 Cecal folds,16 which anchor the lateral aspect of the cecocolon to the parietal wall, are beneficial.
TERMINOLOGY
The terminology “recurrent cecocolic torsion” (RCT) is recommended because the torsion commonly includes the cecum, ascending colon, and the ileum. The ileum is omitted in this expression because it is too cumbersome to enunciate.12,13 “Cecal volvulus” is a familiar term, but it is a misnomer and is misleading because it is an anatomical impossibility,12–14 and it also signifies a late diagnosis after a permanent obstruction has occurred. It is called “cecal bascule”5 when the cecum folds upon itself, usually secondary to a funicular Jackson's membrane, which facilitates this “seesaw” effect. The old term “phantom tumor” was invoked to describe the recurring and spontaneously resolving cystic configuration of the RCT.17 “Floppy” or “mobile cecum syndrome” is a familiar term,18 but is better avoided because it does not confer a pathological innuendo.
INCIDENCE
The incidence of the unfixed cecocolon is documented to be between 20%21 and 33%.12–14,19 After 200 consecutive open and laparoscopic abdominal operations, the author documented 54 patients with mobile cecocolon. Some mobile cecocolon were normal in length, and some were elongated, overrotated, and redundant. Cecal folds, parieto-colic bands, and Jackson's membranes of various configurations were common. Seven of these 54 patients complained of infrequent recurrent abdominal pain (RAP) of varying intensity, and 2 of these patients needed surgical intervention.
The incidence of RCT that proceeds to complete obstruction, the so-called “cecal volvulus,” is estimated to be 30% of all colon obstructions.2,3,20–22 The incidence of symptomatic RCT is estimated to be 0.24% for the general population. The number requiring surgical attention is estimated to be 0.008% for the general population.12,13 RCT, fortunately, is an infrequent problem; however, it needs recognition because many undiagnosed cases occur with substantial morbidity and disability.4,12,13
COMMENT
The lack of insight regarding RCT leaves the clinician without a didactic point of reference on which to base a diagnosis. This is understandable because of the paucity of authoritative and trenchant articles on this topic. RCT is also confusing because its symptomatology has no pattern. Quite possibly, it is also confused with some familiar diagnostic entities and terminologies, eg, kinked appendix and Ogilvie's syndrome. Aggravating this confusion is the advocacy for laparoscopic exploration of the abdomen for RAP and the recommendation for an incidental appendectomy when no pathology is encountered.24 If RCT is not recognized and treated, RAP will recur unless adhesions ensue and produce an iatrogenic cecocolic fixation. It probably bears mentioning that some texts that discuss a differential diagnosis for appendicitis fail to mention RCT.25
Colonoscopy per se can not diagnose RCT because it will straighten and correct a torsed cecocolon and indeed it has been recommended to relieve RCT.3 When the contrast enema is imprudently performed, the mobility and the eccentric location of the cecocolon may be missed, but with proper use, including abdominal x-rays and CT scans, RCT can be proved or ruled out unequivocally.
SYMPTOMS
The history of RAP usually commences before the end of the first decade. The pain has no chronological regularity, and the attacks occur with irregular intervals of days, months, or years. The intensity varies from annoying to severe with some patients seeking repetitive emergency relief. The duration of the attacks varies from short twinges to hours with the attacks usually resolving spontaneously.
The pain is usually ushered in by the mesenteric symptoms of nausea and epigastric and periumbilical fullness. A sensation of distension, fullness, and sometimes a balloon-like tumescence in the RLQ may be present. As fast as the pain and tumescence appear, they may also disappear just as promptly; hence, the term phantom tumor.1,12,13,17
The basic character of the pain is colicky. In the absence of tenderness, the patient usually compresses the right lower abdominal quadrant (RLQ) and may relate that a gaseous rush and diarrhea results in relief of bloating. Many patients describe a personal specific maneuver to relieve or shorten the attacks of pain. They assume an attitude of comfort, and some of those described are straining, standing and walking, squatting and straining, compressing the abdomen and straining, and lying down doubled-up on the right side.12,13,17,19
An attack of pain that becomes persistent, disabling, and is associated with local signs of peritoneal irritation is an ominous sign that suggests an ongoing obstruction and strangulation of the bowel.12,13 The location of the pain is consistent so that an overrotated and redundant cecocolon even in a pelvic or left-sided abdominal location will still present with pain in the RLQ. A right-sided thrust dyspareunia may result in a redundant and elongated cecocolon in a pelvic location.1
Medication given for the pain may coincide with a spontaneous resolution that can lead to an erroneous conclusion that pain relief occurred, but the recurrent nature of the condition will compel the patient to return for more medications, which can lead to a patient being labeled a habitual user of pain medication.17 Usually, the patient has had a previous history of multiple medical and emergency room consultations, colonoscopies, misinterpreted x-ray examinations, and still has no viable diagnosis.12,13,17 Some patients have had negative appendectomies and pelvic explorations and continue to be plagued with RAP, and, in females, dyspareunia, months or years after the operation.
SIGNS
During the intervals between pain, no abdominal guarding occurs although deep tenderness, succussion splash, and gurgling on ballottement of the RLQ may be experienced. A distinct fullness may be palpated at this area.12,13,17 This palpable mass may spontaneously appear and disappear, sometimes with an audible rush on palpatory pressure. This should not make the clinician doubt his finding but alert him to the diagnosis of RCT.12,13,17
Currant jelly stools associated with colicky doubling-up and fretfulness with mild abdominal guarding but without any palpable mass were the presenting findings in a 16-month-old male child in the emergency room.
Tenderness is an ominous warning that obstruction with strangulation may be occurring.12,13 The white blood cell count may elevate moderately during an acute attack of the pain and can be persistently high with an ongoing obstruction-strangulation.
X-RAY DIAGNOSIS
This is the most definitive tool for diagnosing RCT. A plain x-ray film or contrast enema will define the location of a mobile cecocolon, whether it is of normal length, elongated, redundant and overrotated, or it is dilated and hypertrophic and showing signs of pseudo-obstruction. The CT scan may document the cystic configuration of RCT, but this is difficult to demonstrate even if the condition is suspected.11–13 The clinician should discuss the suspected diagnosis of RCT to help the radiologist in positioning the patient to afford various views to demonstrate the mobile cecocolon. The x-ray films showing an acute intestinal obstruction are well documented.21,26 The various diagnostic x-ray presentations of RCT are:
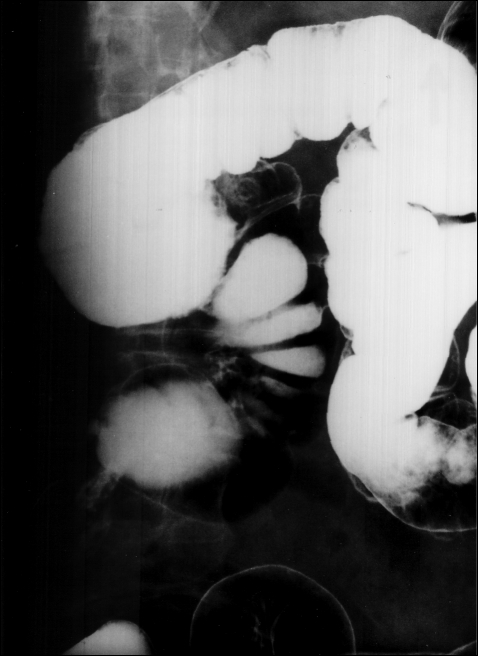
An abdominal film, without contrast, will show the cecocolon above the iliac crest (Figure 1) or elsewhere in the abdomen except the right iliac fossa.
-
With contrast (Barium or Gastrografin enema):
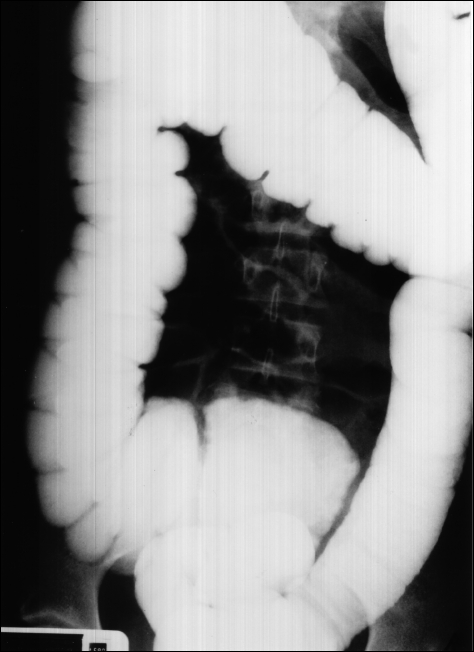
The mobile cecocolon may be redoubled or redundant and located above the iliac rest (Figure 2).
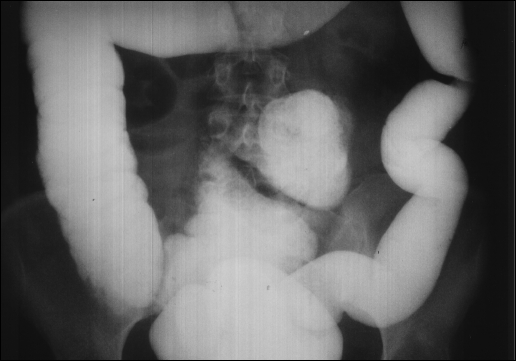
The mobile and redundant cecocolon is deviated toward the midline (Figure 3).
The mobile and elongated cecocolon is located in the pelvis (Figure 4).
The mobile, elongated, and overrotated cecocolon is located in the LLQ and lying transversely across the lower abdomen (Figure 5).
The mobile, elongated, and overrotated cecocolon is located crossing the midline to the left upper abdomen (Figure 6).
An abdominal film, with or without contrast, may disclose a markedly dilated and hypertrophic cecocolon with signs of pseudo-obstruction (Figure 7).
The CT scan may verify any of the above presentations (Figure 8) and may also depict the rare and elusive cystic configuration of RCT (Figure 9).
Figure 1.
The cecum is at the right upper quadrant. Note staples from appendectomy.
Figure 2.
Figure 2. A redundant cecocolon above the iliac crest.
Figure 3.
Cecocolon deviated medially.
Figure 4.
Cecocolon over-rotated into the pelvis.
Figure 5.
Cecocolon over-rotated transversely across the midline in the lower abdomen.
Figure 6.
Cecocolon over-rotated transversely across the midline in the upper abdomen.
Figure 7.
Massively dilated cecocolon with air-contrast located at the upper abdomen in communication with a normal-sized ascending colon.
Figure 8.
CT scan demonstrating the massively dilated cecocolon with air-contrast located at the upper abdomen in communication with a normal-sized ascending colon. A verification of Figure 7.
Figure 9.
A rare CT scan depiction of the cystic configuration of recurrent cecocolic torsion.
DISCUSSION
RCT must always be a consideration in any patient with a consistent history of recurrent right lower abdominal quadrant pain and particularly in the females with thrust dyspareunia. In patients who have had a previous exploration or appendectomy, especially in those who had negative findings, the operative and tissue reports must be reviewed for documentation regarding the presence or absence of RCT.
RCT should be within the purview of the proctologist. The patient usually is not referred to him or her because the patient has already been colonoscoped by a gastroenterologist who does not detect the problem, explored by the gynecologist for complaints of right-sided thrust dyspareunia and pelvic pain without a specific diagnosis, or explored by the general surgeon during an acute presentation in the RLQ who fails to identify RCT and performs an incidental appendectomy without permanently resolving the problem.
An abdominal radiograph with a contrast enema will verify or exclude the diagnosis decisively. An acute situation does not constrain the use of water-soluble contrast enema, which may detorse an RCT. However, being under fluoroscopic control, the torsion can be verified and documented by a radiologist who is aware of the clinical situation.12,13,27 Colonoscopy is not the procedure of choice for diagnosis because it may reduce and reposition a torsed or eccentrically located cecocolon and even reduce an intussusception or introrsion without recognition of RCT.
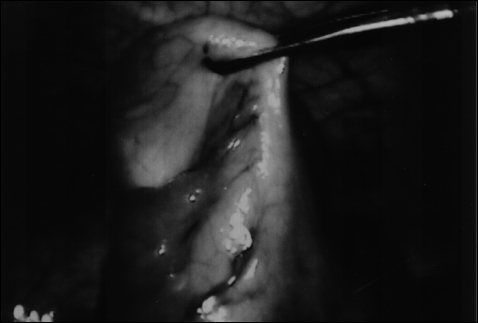
At laparoscopy or open laparotomy, regardless of whether appendicitis is present or not, the picture of a mobile cecocolon is unmistakable (Figures 10 and 11), and the surgeon should correct the cecocolic mobility. The presence of Jackson's membrane and parieto-colic bands in their various configurations must not be mistaken for adhesions.
Figure 10.
Laparoscopic picture of a freely mobile cecocolon.
Figure 11.
A mobile and redundant cecocolon at laparotomy, showing the site of the kink.
Figure 1 shows the cecum with staples from a previous appendectomy located in the right upper quadrant of the abdomen. The patient continued to have RAP 3 years after the previous appendectomy for a “mesenteric adenitis.” Figure 2 shows the redundant cecocolon above the iliac crest. The patient has had RAP since 13 years of age. Figure 3 shows a medially deviated cecocolon with an obvious area of kinking in a patient with dyspareunia. Figure 4 depicts the pelvic location of the cecocolon on a patient who has dyspareunia. Figure 5 presents a cecum incarcerated as a left inguinal hernia. The cecocolon is lying transversely across the lower abdomen. Figure 6 reveals the cecum across the midline and located at the left upper abdominal quadrant. Figure 7 is a patient who had RAP since her teens and shows an extremely distended and dilated cecocolon located transversely across the upper abdomen containing air and water-soluble contrast in direct communication with the ascending colon, which has a normal caliber. Figure 8 shows the CT scan of the foregoing patient in Figure 7, verifying the communication of the pseudo-obstruction of the cecocolon and the normal ascending colon. Figure 9 shows the elusive CT scan depiction of the torsed cystic configuration of a cecocolon. Possibly, this may be 1 of only 2 identified CT scans in existence demonstrating the cystic configuration of a cecocolic torsion.17
All the foregoing patients who underwent cecocolopexy experienced symptom relief. The patient in Figure 5 had a release of her incarcerated left inguinal hernia but declined cecocolectomy and continues to have mild RAP. The patients in Figure 7 and Figure 8 had a segmental cecocolectomy with resolution of their problems.
The lack of cecocolic fixation allows recurrent introrsions and intussusceptions with spontaneous resolutions, which may explain the mechanism of the colicky RAP. In the previously mentioned 16-month-old child, the proverbial abdominal mass of an intussusception was not palpated. His abdomen was relatively soft, with mild guarding. He may have had introrsions or intussusception that had already spontaneously resolved. The gastrografin enema verified the eccentrically located, mobile cecocolon. This case implies that the presence of currant jelly stools is not necessarily pathognomonic of intussusception but may be a result of an erosion of an ischemic mucosa during the process of introrsions or torsion.
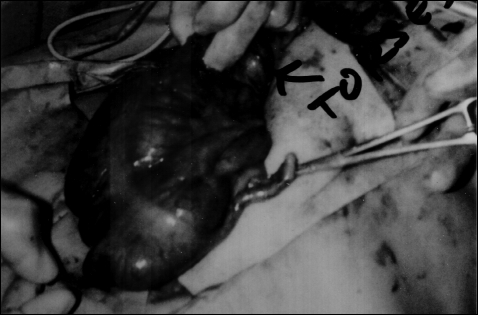
A 79-year-old female who had a lifetime history of RAP with a palpable fullness in the upper abdomen was initially diagnosed as having Ogilvie's syndrome of pseudo-obstruction. (Figures 7 and 8). This diagnosis was challenged and changed to RCT mainly because she had a prolonged history of RAP. Her tenderness was felt at the right hemi-abdomen, and only an unfixed and unanchored cecocolon could be located across the abdominal midline regardless of the size of a cecocolic distension and pseudo-obstruction. Because she was clinically deteriorating from her comorbidities, laparotomy was performed that verified the diagnosis of RCT. She recovered uneventfully after a cecocolectomy was performed for a hyperemic, thickened, and hypertrophic cecocolic segment (Figure 12). This case illustrates that chronic recurrent torsion with spontaneous resolution can result in cecocolic wall hypertrophy. It eventually overdilates and outpaces its end-arterial blood supply with its muscles becoming decompensated and flaccid thereby losing peristaltic capacity. Having become flaccid, it can develop the picture of pseudo-obstruction unlike Ogilvie's pseudo-obstruction, which is believed to result from “parasympathetic deficiency” to that segment of the intestine.23
Figure 12.
A dilated, hypertrophic, thick-walled, hyperemic, and tumescent cecocolic segment at laparotomy.
TREATMENT
The treatment of choice for RCT is outpatient laparoscopic cecocolopexy with interrupted nonabsorbable sutures to anchor the tinea libera to the parietal peritoneal wall of the right iliac fossa at about the level of the anterior superior iliac spine.1,8,12,13,18 Right hemicolectomy or cecocolectomy is recommended for a cecocolon when: 3,12,13,28
It is flimsy and dilated.
It is strangulated.
Viability is suspect.
It is overrotated and redundant and will foreshorten, accordion, and obstruct after cecocolopexy.
It is tumescent, hypertrophic, thickened, hyperemic, dilated, decompensated, and nonperistaltic.
Laparoscopic, laparoscopically assisted, or classical open resections are options at the operator's disposal with an already congenitally mobile cecocolon. Jackson's membrane and parieto-colic bands, which are generally mistaken for adhesions, should be resected especially if they are funicular because they may function as a fulcrum to facilitate the kinking and torsion of the mobile cecocolon specifically if cecopexy is not performed. During laparotomy for RAP, whether open or laparoscopic, it is incumbent upon the general surgeon to identify a mobile cecocolon and perform cecocolopexy, especially in the presence of a grossly normal appendix. Incidental appendectomy should be performed if no contraindications to the procedure exist.
Proponents of various procedures exist: simple detorsion by colonoscopic insufflation or contrast enema,3,4,29 cecostomy,3 cecopexy,8,12,13,18,26 a combination of cecopexy and cecostomy,3,28 cecopexy with peritoneal flap,5,9 and mesh.30
The appalling recurrence rate, morbidity, and mortality in studies by 3 authors in 3 countries, which included 700 patients, for 12 to 30 years, can only be explained by late diagnoses and treatment of RCT, which proceeded to obstruction and strangulation before the surgical treatment was instituted.2–4
CONCLUSION
RCT may result from 2 developmental defects: The mobility of the cecocolon with the absence of a mesocecocolon to anchor it to the parietal wall of the abdomen associated with an elongated, overrotated, and redundant cecocolon, which results in an inherent predisposition for it to torse and obstruct.
The knowledge that approximately 30% of the population have this developmental defect should always alert the clinician to consider RCT in the differential diagnosis of the patient who complains of recurrent RAP in the RLQ. This should be the primary consideration in the patient who has had multiple consultations, colonoscopies, and other procedures and still has no viable diagnosis to explain the RAP.
The alert diagnosis and treatment of RCT will forestall the morbidity and mortality attendant to an obstructing and strangulating event of the cecocolon. When the RCT becomes associated with progressive tenderness, a cecocolic obstruction and strangulation may be ongoing. It will need prompt surgical intervention.
The abdominal radiograph is the sine qua non for the diagnosis of RCT. The contrast enema will provide an unequivocal diagnosis of RCT. A plain x-ray film of the abdomen and a CT scan may document the eccentric location and unusual morphology of a mobile cecocolon. Acute presentations do not contraindicate the use of water-soluble contrast study for diagnosis.
The elective treatment of choice is outpatient laparoscopic cecocolopexy. Laparoscopic or open classical segmental cecocolectomy or right hemicolectomy is recommended when the cecocolic viability is suspect or for a more complex and morbid status of the cecocolon.
References:
- 1. Tirol FT. Dyspareunia: A symptom of cecocolic torsion. Abdm Surg. Fall 2001;11–15 [Google Scholar]
- 2. Anderson JR, Welch GH. Acute volvulus of the right colon; an analysis of 69 patients. World J Surg. 1986;10:336–342 [DOI] [PubMed] [Google Scholar]
- 3. Ballantyne GH, Brandner MD, Beart RW, Ilstrup DM. Volvulus of the colon. Incidence and mortality. Ann Surg. 1985;202:83–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rabinovici R, Simansky DA, Kaplan O, Mavor E, Manny J. Cecal Volvulus. Dis Colon Rectum. 1990;33:765–769. [DOI] [PubMed] [Google Scholar]
- 5. Wolf BG. Volvulus of the colon. In: Cameron JL. ed, Current Surgical Therapy. 3rd ed Toronto, Canada: BC Decker Inc; 1989:130–131 [Google Scholar]
- 6. Buchanan GD. Embryology. In: Didio LJA. ed, Synopsis of Anatomy. St. Louis: V. Mosby Co; 1970:93–98 [Google Scholar]
- 7. Bryne WJ, D'Harlingue AE. The gastrointestinal system. General considerations. In: Taeusch W, Ballard RA, Avery ME. eds. Schaffer and Avery's Diseases of the Newborn. 6th ed Philadelphia:WB Saunders Co; 1988:1054–1062 [Google Scholar]
- 8. Frantzides CT, Cziperle DJ, Soergel K, Stewart E. Laparoscopic Ladd procedure and cecopexy in the treatment of malrotation beyond the neonatal period. Surg Laparosc Endosc. 1996;6:73–75 [PubMed] [Google Scholar]
- 9. Smith WR, Goodwin JN. Cecal Volvulus. Am J Surg. 1973;126:215–222. [DOI] [PubMed] [Google Scholar]
- 10. Thorek P. Anatomy in Surgery. 2nd ed Toronto, Canada: JB Lippincott Co; 1962 [Google Scholar]
- 11. Tirol FT. Laparoscopic cecocolopexy with polypropylene mesh. Abdm Surg. Fall 1999;16–19 [Google Scholar]
- 12. Tirol FT. Recurrent cecocolic torsion. Phantom tumors. Abdm Surg. Fall 1999:20–24 [Google Scholar]
- 13. Tirol FT. Recurrent cecocolic torsion. Paper presented at: 40th National Congress of the American Society of Abdominal. Surgery May 1999 San Diego, Calif [Google Scholar]
- 14. Wolfer JA, Beaton LE, Anson BJ. Volvulus of the cecum. Anatomical factors in its etiology. Report of a case. Surg Gynec Obstet. 1942;74:882–892 [Google Scholar]
- 15. Seoudi HM, Curletti EL. Midgut nonrotation presenting in adults. Comp Surg. 1996;15(1):137–142 [Google Scholar]
- 16. Netter FH. Atlas of Human Anatomy. Summit, NJ: Ciba-Geigy Corp; 1989. Plate 264 [Google Scholar]
- 17. Tirol FT. Recurrent cecal volvulus. Phantom tumors. Abdm Surg. Fall 1998;12–13 [Google Scholar]
- 18. Shoop SA, Sackier JM. Laparoscopic cecopexy for cecal volvulus. Surg Endosc. 1993;7:450–454 [DOI] [PubMed] [Google Scholar]
- 19. Donhauser JL, Atwell S. Volvulus of the Cecum, A review of one hundred cases. In literature and a report of six new cases. Arch Surg. 1949;58:129–147 [PubMed] [Google Scholar]
- 20. Anson BJ, Maddock WG. eds. Callander's Surgical Anatomy. 4th ed Philadelphia: WB Saunders Co; 1989:516–522 [Google Scholar]
- 21. Corman ML. Volvulus. In: Colon and Rectal Surgery. 2nd ed Philadelphia, Pa: JB Lippincott Co; 1989:732–735 [Google Scholar]
- 22. Spitz L. Neonatal intestinal obstruction and intussusception in childhood. In: Maingot's Abdominal Operations. Stamford, Conn: Appleton-Century-Crofts; 1985;1054–1062 [Google Scholar]
- 23. Tenofsky PL, Beamer L, Smith RS. Ogilvie's Syndrome as a postoperative complication. Arch Surg. 2000;135:682–686 [DOI] [PubMed] [Google Scholar]
- 24. Stringel G, Berezin SH, Bostwick HE, Halata MS. Laparoscopy in the management of children with chronic recurrent abdominal pain. JSLS. 1999;215–219 [PMC free article] [PubMed] [Google Scholar]
- 25. Harrison EH. Appendectomy. In: Ballantyne GH, Leahy PF, Modlin IM. eds. Laparoscopic Surgery, Philadelphia, Pa: WB Saunders Co; 1994:499–507 [Google Scholar]
- 26. Ellis H. Special forms of intestinal obstruction. In: Maingot's Abdominal Operations. Stamford, Conn: Appleton-Century-Crofts; 1985:1186–1190 [Google Scholar]
- 27. Tirol FT. Letter to Editor. JSLS. 2000;4:183–184 [PMC free article] [PubMed] [Google Scholar]
- 28. Halvorsen JF, Semb BHK. Volvulus of the right colon. A review of 30 cases with special reference to late results of various surgical procedures. Acta Chir Scand. 1975;141:804–809 [PubMed] [Google Scholar]
- 29. Smith CD, Fink AS. Colonic Volvulus. In: Cameron JL. ed. Current Surgical Therapy. 6th ed Philadelphia: Mosby Inc.;1999:194–195 [Google Scholar]
- 30. El Katib Y. Volvulus of the cecum: Caecopexy by plovinyl alcohol sponge. Brit J Surg. 1973;60:475–478 [DOI] [PubMed] [Google Scholar]