Abstract
Background:
Although the technical feasibility of laparoscopic management of Crohn's disease has been described, it remains of limited perceived usefulness in the management of surgically complex Crohn's. Successful management of such disease by using minimal access techniques is described.
Patients and Methods:
Seventeen patients underwent laparoscopically assisted procedures to address clinically complex disease. Goals of the laparoscopic phase included mobilization of pertinent structures, localization of disease, and precise selection of incision location. Clinical situations encountered included fistulas, multiple-or long-segment disease, abscesses, and reoperative management.
Results:
Conversion to completely open procedures was not necessary in any case. Operative time was longer in complex Crohn's disease than in concurrently managed patients who underwent laparoscopic ileal/cecal resection for limited disease (244±18 vs 127±5 minutes, P<0.05). Management of long-segment or multi-segment disease was associated with the longest operative times (292±36 minutes). Length of hospitalization was also longer than after management of limited ileal disease (7.1±1.4 vs 4.5±0.4 days). Major complications occurred in 18%.
Conclusions:
Laparoscopic techniques can be applied to complex Crohn's disease with effective disease management. In patients who may require multiple procedures, maintenance of abdominal wall integrity should be of significant value.
Keywords: Laparoscopy, Crohn's disease, Fistula, Reoperative
INTRODUCTION
The patterns of pathology associated with surgically treated Crohn's disease can present challenges to the most skilled surgeons. The most straightforward cases involve short segment structuring disease of the terminal ileum without other, more complex features. Recent work has shown that these cases lend themselves to laparoscopic management, with the presumed benefits of minimally invasive methods observed for other diseases.1 Although these benefits have not been clearly demonstrated for patterns of disease other than limited terminal ileal, enough evidence has accumulated to suggest that laparoscopic or laparoscopically assisted procedures for Crohn's disease are suitable alternatives to open surgery when performed by experts. More complicated Crohn's disease, such as disease complicated by fistula, abscess, more extensive lengths of involved intestine, or need for reoperative care, represents a more formidable undertaking than short-segment terminal ileal disease even when the conventional open surgical technique is used. The technical feasibility of such management using laparoscopic methods has been suggested2–4 but remains controversial and is certainly not in routine use. Given the risk of eventual need for reoperation in this group, minimally invasive methods may offer these patients the greatest potential benefits despite technical difficulties imposed by their disease. In the present series, all patients with surgically complex Crohn's disease managed by a single surgeon underwent laparoscopic exploration with laparoscopically assisted measures to address the disease to define the effectiveness of systematic management.
PATIENTS AND METHODS
Seventeen patients (11 male, 6 female; 18 to 80 years old, mean 44±4 years) were identified from the 91 patients entered in the Yale University Surgical Gastroenterology Inflammatory Bowel Disease Database as having had surgical management of complex Crohn's disease using laparoscopic methods between March 1998 and October 2001. Complex Crohn's disease was defined as those cases involving 1 of 4 predefined criteria that increase the complexity of operative tasks and intraoperative decision-making (Table 1). Patient characteristics and indications for surgery were variable (Table 2). Most cases were reoperative. In 2 cases, 4 or more prior procedures for Crohn's disease had been performed. Prior procedures consisted primarily of terminal ileal and cecal resection, although other prior operations included diverting transverse colostomy, sigmoid colectomy, and appendectomy performed at the time of the Crohn's diagnosis. The presence of Crohn's disease had been clearly established by these prior operative procedures in all patients. Distribution of current disease was ascertained by preoperative investigations. Barium small bowel series, barium enema, colonoscopy with terminal small bowel examination, and abdominal CT were used as needed in all patients. Broad surgical goals (Table 3) were modified as needed for individual patients based on anatomic features of the disease. Laparoscopic access was obtained in open fashion in all cases. Paraumbilical primary ports were placed in cases of an initial procedure, and left-sided ports remote from old incisions were made during reoperative cases. Resection when necessary was performed in a highly conservative fashion (mini-resection), except where stricturing disease was so extensive and concentrated within longer segments that more aggressive resectioning was unavoidable. Efforts were made to keep open incisions for specific disease management to 8 cm or less in length, with the precise location determined by anticipated reach of mobilized mesentery. Where possible, incisions were localized to the infraumbilical area or a single abdominal quadrant (primarily transverse right-sided), carefully avoiding incisions in possible stoma sites (Figure 1). Operative time (incision to completed closure), complications, and length of hospital stay (LOS) were recorded prospectively. Follow-up was by direct interview and examination or telephone interview if no examination had occurred in the prior 12 weeks. Statistical analysis was performed with the Mann-Whitney U test.
Table 1.
Complex Crohn's Disease
| 1. Prior abdominal surgery for Crohn's disease |
| 2. Fistula |
| 3. Extensive (>50 cm) or multiple discontiguous segments of disease |
| 4. Abscess |
Table 2.
Demographic Characteristics of Patients Undergoing Laparoscopic Treatment of Complex Crohn's Disease
| Patient | Age/Sex* | Prior Surgery | Pattern of Disease† | Operation | Incision‡ |
|---|---|---|---|---|---|
| 1 | 26/M | None | Multisegment SB | Resection | Long |
| 2 | 47/M | Appendectomy | Multisegment SB | Resection, Stricturoplasty | Long |
| 3 | 46/M | Ileocecectomy | Recurrent Ileal | Resection | TrRLat |
| 4 | 40/F | Ileocecectomy | Adhesive | Lysis of Adhesions | None |
| 5 | 49/M | Mult SB Resection | Multisegment SB | Resection, Stricturoplasty | TrLLat |
| 6 | 20/M | Colostomy | Transverse colon, Abscess | Resection | TrLLat |
| 7 | 80/M | Sigmoidectomy | Left colon | Resection | Long |
| 8 | 73/M | None | Ileocolic fistula | Resection | Long |
| 9 | 18/F | None | Ileal, Abscess | Drainage, Appendectomy | None |
| 10 | 52/M | None | Multisegment, EC Fistula | Resection, Stricturoplasty | Long |
| 11 | 41/M | None | Multisegment, Ileocolic fistula | Resection | Long |
| 12 | 34/M | Ileocecectomy | Recurrent ileal, Ileocolic fistula | Resection | TrRLat |
| 13 | 33/F | None | Ileal, Ileocolic fistula | Resection | TrRLat |
| 14 | 54/F | Mult SB Resection | Recurrent ileal | Resection | TrRLat |
| 15 | 48/F | Mult SB Resection | Long segment jejunal | Stricturoplasty | Long |
| 16 | 36/F | Ileocecectomy | Recurrent ileal | Resection | TrRLat |
| 17 | 51/M | Ileocecectomy | Recurrent ileal, Ileocolic fistula | Resection | TrRLat |
M=male, F=female.
SB=small bowel, EC=enterocutaneous.
L=left, R=right, Long=longitudinal, Tr=transverse, Lat=lateral.
Table 3.
Operative Goals in Laparoscopic Management of Complex Crohn's Disease
| 1. Safe laparoscopic access and exposure |
| a. Open primary port placement in reoperative cases |
| b. Lysis of adhesions related to prior procedures |
| 2. Inspection of GI tract and identification of diseased segments |
| 3. Mobilization of appropriate intestinal segments |
| 4. Appropriate selection of limited open incision site |
| 5. Laparoscopically-assisted mini-resection and stricturoplasty for stricturing disease |
| 6. Fistula resection/repair |
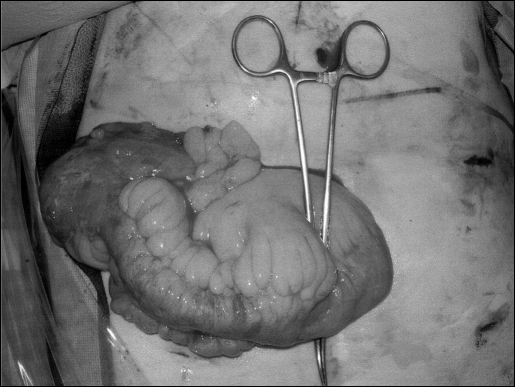
Figure 1.
Open phase of laparoscopically assisted procedure for recurrent terminal ileal Crohn's disease. Ileal-sigmoid colon fistula was managed by laparoscopically stapling across fistula site on the otherwise normal colon, facilitating mobilization of the ileocolic anastomosis through a transverse right-sided incision.
RESULTS
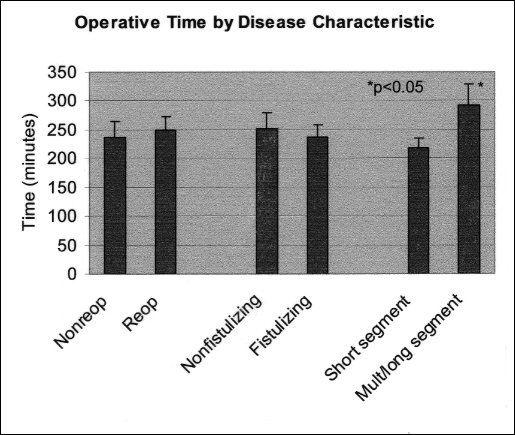
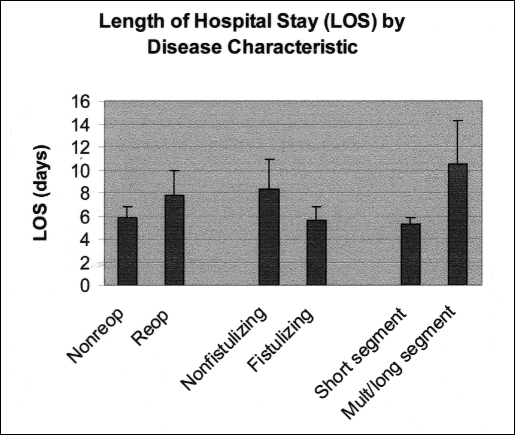
Conversion to fully open abdominal procedures was not required in any patient in the present series. Two patients required open incisions 10-cm long to manage fixed mesenteric mass and fistulizing disease. One patient thought to have chronic small bowel obstructive pathology due to Crohn's disease proved to have purely adhesive obstruction. Complications included intraabdominal abscess and fistula in 1 patient (7%) managed by nonoperative means (percutaneous drainage and TPN). This complication resulted in a prolonged hospitalization associated with further complications of central venous catheter sepsis and subclavian vein thrombosis. Postoperative wound infection occurred in 1 patient (7%). Overall length of operation was greatest in those patients with long- or multiple-segment disease (Figure 2), 83% of which were also reoperative cases with or without fistula. Overall hospital stay was also significantly greater in this patient category (Figure 3). Both operative time and hospital length of stay were significantly longer in patients with complex disease than in a concurrently managed group of 8 patients who underwent laparoscopic ileocecal resection for limited ileal Crohn's disease (244±18 minutes and 7.1±1.4 days versus 127±5 and 4.8±0.5 days, respectively). All patients received postoperative therapy consisting of either mesalamine or 6-mercaptopurine. At 2 to 58-month follow-up (median 16 months), 14 patients had relief of the Crohn's disease symptoms that precipitated operative care. Two patients had significant residual disease following surgery that was responsible for ongoing but attenuated symptoms, and 1 patient had recurrence of symptomatic ileal Crohn's disease 12 months following surgery that responded to medical therapy (total 18% symptomatic). No patients have required reoperation for Crohn's-related complications. To date, no incisional hernias have been diagnosed.
Figure 2.
Neither reoperation nor fistula corresponded to longer operative times. Extensive lengths and multiple segments of diseased intestine were associated with longer operations because of intense inflammatory changes along a greater length of bowel, with accompanying inflammatory mass(es).
Figure 3.
Findings suggest that multi-segment or long-segment disease is associated with longer hospitalization. This observation is best explained by longer delays in resumption of diet in this group, as well as the occurrence of complications in 2 patients, which delayed discharge.
DISCUSSION
Our present experience indicates that more complex patterns of Crohn's disease are amenable to a routine laparoscopic approach without imposing significant morbidity associated with lengthy procedures. Extracorporeal inspection of disease and selection of the most appropriate sites for stricturoplasty and resection are practical adjustments in minimally invasive techniques given the magnitude of pathology treated in these patients. Open incisions remained very small in most patients although in situations where the most marked inflammatory masses were encountered, relatively larger incisions were required for exposure and specimen removal. It was felt that the preoperative goals of mobilization of diseased bowel segments and minimization of incision size were complementary, in part because incision location could be carefully defined during the laparoscopic phase of the procedure. These goals were successfully attained in all patients.
Laparoscopic or laparoscopically assisted procedures have been undertaken for a variety of inflammatory and neoplastic conditions of the intestinal tract to achieve the same benefits thought possible when substantial incisions are avoided in other situations: diminished pain, more rapid resolution of ileus, improved pulmonary function, and possibly diminished postoperative adhesions compared with those in fully open procedures. However, in contrast to cholecystectomy, these approaches to enterocolic diseases have not at all been accepted as the “gold standard” of surgical treatment. In part, this may be due to limited surgeon acceptance of advanced laparoscopy. However, beliefs regarding Crohn's disease itself may also be contributory. Among the characteristics of the disease that are potentially imposing to the laparoscopic surgeon, are the changes related to intense local inflammation. Mesenteric shortening, masses related to matted bowel loops, thickened mesentery, abscesses, as well as adhesions from prior surgery are rightly viewed as technical obstacles to successful exposure and treatment of disease.
As expected, the technical difficulties encountered in the present series were more considerable than those encountered in the treatment of short-segment terminal ileal disease. However, they proved to be quite manageable when diseased segments were directly accessed during the open phase of each procedure. Abscesses were drained during laparoscopic dissection, or resected within an inflammatory mass, and did not impose problems specific to laparoscopy. This confirms an observation made previously by Wu et al5 that neither abscess nor phlegmon were specific contraindications to laparoscopically assisted treatment. Similarly, reoperative therapy proved manageable following access to the abdomen at a site remote from any abdominal wall incisions and lysis of adhesions to both parietal peritoneum and disease site. The lengthiest procedures were those involving cases of multiple disease segments, or long-segment disease (>50 cm of gross Crohn's involvement). These cases tended to be more complicated to manage laparoscopically in part due to the relative immobility of diseased segments, as well as the complexities of determining precise disease distribution, compounded in some cases by superimposed factors, such as adhesions of prior surgery, and the presence of intense inflammation associated with fistula. The presence of fistula alone, or reoperative management alone, had no apparent bearing on procedure length.
Laparoscopic procedures have been suggested to result in improved cosmesis compared with that in open operations for Crohn's disease,6 but questions have been raised as to whether this particular potential advantage justifies what has been described as an excessively long and difficult surgery.7 These questions might be thought to be especially relevant to the management of more complex clinical situations. Although cosmesis alone may be questioned as a primary consideration, it is the strong impression of the authors that body image issues, although difficult to quantify, are very important in patients with Crohn's disease. Furthermore, the issue of preservation of abdominal wall integrity begs the question of incisional hernia risk, particularly in patients with potential wound healing defects consequent to impaired nutrition and the use of potent immunosuppressive medications.
Estimates of the need for eventual reoperation for Crohn's disease are variable and dependant on length of follow-up, but many reports concur on a figure in the 40% to 50% range by 10 years postoperatively.8–10 A subgroup of these patients will require multiple procedures, as evidenced by the 2 patients in the present series who had undergone 4 or more operations. In our view, one of the more compelling reasons to undertake laparoscopic therapy is to avoid multiple episodes of abdominal wall injury with repeated abdominal explorations in the subset of patients at risk for such repeated surgery. Significant disability as the result of disturbance of abdominal wall blood supply, surgical treatment of incisional hernias, and behavioral alterations as a consequence of altered body image after multiple open procedures are very likely to prove much less problematic after laparoscopic operations.
Although follow-up is somewhat limited in this series, the 18% incidence of symptomatic Crohn's observed in these patients compares favorably with reports of symptomatic recurrence as high as 39% within 3 years following open operations for reoperatively managed Crohn's disease.9 To date, no patient has required reoperation following a laparoscopic procedure, and no comment can be made concerning postoperative adhesions. Some limited recent work has suggested that laparoscopy in Crohn's disease patients is associated with attenuation of selected aspects of systemic inflammatory response.11 Further work and longer periods of follow-up are required to determine whether minimal access procedures actually alter the natural history of disease in surgically treated Crohn's disease patients. However, the present results suggest strongly that for patients with complex Crohn's disease laparoscopic surgery in the hands of an experienced surgeon is very acceptable alternative to open surgery.
References:
- 1. Milsom JW, Hammerhofer KA, Bohm B, et al. Prospective, randomized trial comparing laparoscopic versus conventional surgery for refractory ileocolic Crohn's disease. Dis Colon Rectum. 2000; 44: 1–9 [DOI] [PubMed] [Google Scholar]
- 2. Canin-Endres J, Salky B, Gattorno, Edye M. Laparoscopically assisted intestinal resection in 88 patients with Crohn's disease. Surg Endosc. 1999; 13: 595–599 [DOI] [PubMed] [Google Scholar]
- 3. Joo JS, Agachan F, Wexner SD. Laparoscopic surgery for lower gastrointestinal fistulas. Surg Endosc. 1997; 11: 116–118 [DOI] [PubMed] [Google Scholar]
- 4. Poulin EC, Schlachta CM, Mamazza J, Seshadri PA. Should enteric fistulas from Crohn's disease or diverticulitis be treated laparoscopically or by open surgery? A matched cohort study. Dis Colon Rectum. 2000; 43: 621–626 [DOI] [PubMed] [Google Scholar]
- 5. Wu JS, Birnbaum EH, Kodner IJ, Fry RD, Read TE, Fleshman JW. Laparoscopic-assisted ileocolic resections in patients with Crohn's disease: are abscesses, phlegmons, or recurrent disease contraindications? Surgery. 1997; 122: 682–689 [DOI] [PubMed] [Google Scholar]
- 6. Dunker MS, Stiggelbout AM, van Hogezand RA, et al. Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn's disease. Surg Endosc. 1998; 12: 1334–1340 [DOI] [PubMed] [Google Scholar]
- 7. Breen EM, Ashley SW. Laparoscopic surgery for Crohn's disease?–A conditional yes. Inflamm Bowel Dis. 2000; 6: 43–45 [DOI] [PubMed] [Google Scholar]
- 8. Post S, Herfarth C, Bhm E, et al. The impact of disease pattern, surgical management, and individual surgeons on the risk for relaparotomy for recurrent Crohn's disease. Ann Surg. 1996; 223: 253–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Heimann TM, Greenstein AJ, Lewis B, Kaufman D, Heimann DM, Aufses AH., Jr Comparison of primary and reoperative surgery in patients with Crohn's disease. Ann Surg. 1998; 227: 492–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Krupnick AS. Morris JB. The long-term results of resection and multiple resections in Crohn's disease. Semin Gastrointest Dis. 2000; 11: 41–51 [PubMed] [Google Scholar]
- 11. Hildebrandt U, Kessler K, Pistorius G, et al. Granulocyte elastase and systemic cytokine response after laparoscopic-assisted and open resections in Crohn's disease. Dis Colon Rectum. 1999; 42: 1480–1486 [DOI] [PubMed] [Google Scholar]