Abstract
Introduction:
Laparoscopic splenectomy has become the procedure of choice for those patients who need to have a splenectomy. The skills required to perform a laparoscopic splenectomy are not easy to learn and therefore may limit the availability of this procedure to patients.
Methods:
We present a hand-assisted technique that allows the performance of a laparoscopic splenectomy safely and rapidly by surgeons without a great deal of experience with this procedure.
Results:
A laparoscopic hand-assisted splenectomy was performed by a chief resident who had not performed this procedure before. The operative time was comparable to that of a laparoscopic splenectomy performed by an experienced laparoscopic surgeon at our institution (65 vs 62 min).
Conclusions:
The hand-assisted technique is useful in a number of laparoscopic situations. We suggest that hand-assisted laparoscopic surgery might be used as an adjunct for surgeons with limited laparoscopic experience and for residents who are learning advanced laparoscopic skills.
Keywords: HALS, Laparoscopy, Splenectomy
INTRODUCTION
A splenectomy is indicated in a variety of disease states: malignancy, staging, diagnosis, trauma, and infection. In the past, open splenectomy was the procedure of choice. In 1991, Delaitre et al1 reported the first successful laparoscopic splenectomy. Benefits of the laparoscopic approach include decreased postoperative pain, better cosmesis, faster return of bowel function, earlier return to normal activities, and shorter hospital stays.2 Laparoscopic splenectomy is now the standard of care and is associated with a conversion rate to open splenectomy of less than 7%.3
Despite its popularity, some limitations exist. Splenomegaly and traumatic rupture of the spleen were considered relative contraindications to laparoscopic splenectomy due to the difficulties with manipulation and visualization. In addition, certain splenic malignancies require removal of an intact spleen for pathologic diagnosis. By necessity, one of the ports must be dilated to fit the spleen, which negates many of the benefits of a laparoscopic procedure. Finally, a laparoscopic splenectomy requires the surgeon to have advanced laparoscopic skills and therefore it may be underutilized.
In the 1995, Kusminsky et al4 introduced the hand-assisted laparoscopic technique as an adjunct to laparoscopic splenectomy. Hand-assisted laparoscopic surgery (HALS) uses a port large enough to accommodate the surgeon's hand. Several different ports are now on the market (the Dexterity Pneumo Sleeve, the Lap Disc, the Hand Port, the Intromit), which allow the maintenance of pneumoperitoneum while the surgeon's hand is within the abdomen. This technique allows hand-assisted manipulation and dissection of the spleen, manual control of large vessels, and removal of an intact spleen through the hand port.
Since the application of hand-assisted techniques, the application of laparoscopic splenectomy has expanded.3–8 Several reports have now been published in the literature about laparoscopic splenectomies for massive splenomegaly (>1000 g),5 traumatic rupture of the spleen, splenectomy during pregnancy,7 and excision of a splenic hydatid cyst.1,4 We report the use of a hand port to assist a resident who is learning the technique of laparoscopic splenectomy.
METHODS
A 43-year-old male initially presented with left lower quadrant pain. He was evaluated for diverticulitis with a computed tomography (CT) scan. In addition to demonstrating mild inflammation around the sigmoid colon, he was noted to have 15 to 20 lesions <1 cm within the spleen. Once he recovered from his diverticulitis, he underwent a follow-up CT scan that revealed that the lesions in his spleen had grown. He underwent an extensive workup that included magnetic resonance imaging (MRI) of the abdomen, positron emission tomography (PET) scan, bone marrow biopsy, multiple blood cultures, laboratory tests, and peripheral blood smears. The differential diagnosis included malignancy, sarcoidosis, and infections. Because the workup failed to reveal a cause for the lesions in his spleen, he was referred for a splenectomy.
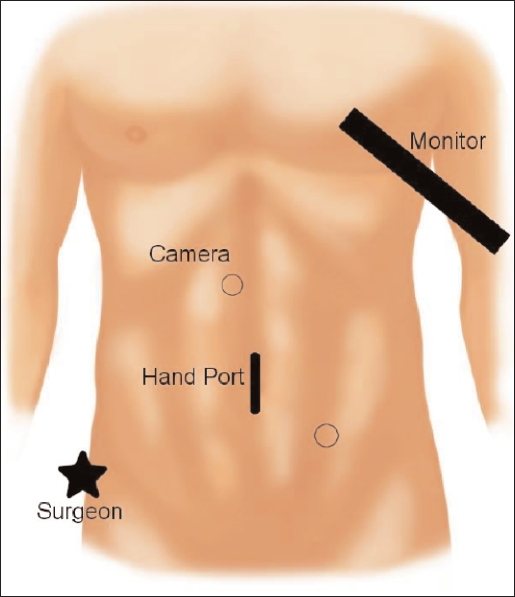
The patient underwent a hand-assisted laparoscopic splenectomy. The surgery was conducted by a chief resident with the assistance of an experienced laparoscopic surgeon. A hand port was inserted in the periumbilical position. Two additional ports were placed under direct vision (Figure 1).
Figure 1.
Port sites for hand-assisted laparoscopic splenectomy.
The splenectomy was then carried out in a standard fashion: ligation of the short gastric vessels, dissection of the hilum, use of the endo-GIA for the splenic vessels, dissection of the peritoneal attachments, removal of the intact spleen through the hand port, and closure of ports.
The patient recovered uneventfully from his splenectomy. The pathology revealed noncaseating granulomas. He was subsequently diagnosed with Bartonella (Cat Scratch Disease) and treated with doxycycline.
RESULTS
A hand-assisted laparoscopic splenectomy was performed by a chief resident who had not performed this procedure before. He accomplished the surgery in 65 minutes. This is comparable to an experienced laparoscopic surgeon's time performing a laparoscopic splenectomy without a hand port (average time, 62 min).
CONCLUSION
The hand-assisted technique is useful in a number of different situations. Specifically, it can be used as an aid in the removal of a massive spleen as well as in the setting of traumatic rupture of the spleen. It can also be used instead of converting to an open procedure when the anatomy is difficult or bleeding is encountered. In addition, we suggest that since a chief resident was able to perform the procedure efficiently using HALS splenectomy, it should also be considered as a possible bridge to performing a strictly laparoscopic splenectomy. Future studies are needed and should attempt to investigate whether the hand-assisted technique offers the same benefits as laparoscopy in terms of postoperative pain, better cosmesis, faster return of bowel function, early return to normal activities, and shorter hospital stays.
References:
- 1. Delaitre B, Maignien B. Splenectomy by the laparoscopic approach. Report of a case [in French]. Presse Med. 1991; 20: 2263. [PubMed] [Google Scholar]
- 2. Heniford TB, Matthews BD, Answini GA, Walsh RM. Laparoscopic splenectomy for malignant diseases. Semin Laparosc Surg. 2000; 7 ( 2): 93– 100 [PubMed] [Google Scholar]
- 3. Targarona EM, Balague C, Trias M. Hand-assisted laparoscopic splenectomy. Semin Laparosc Surg. 2001; 8 ( 2): 126– 134 [PubMed] [Google Scholar]
- 4. Kusminsky RE, Boland JP, Tiley EH, Deluca JA. Hand-assisted laparoscopic splenectomy. Surg Laparosc Endosc. 1995; 5 ( 6): 463– 467 [PubMed] [Google Scholar]
- 5. Ballaux KEW, Himpens JM, Leman MRP. Hand assisted laparoscopic splenectomy for hydatid cyst. Surg Endosc. 1997; 11: 942– 943 [DOI] [PubMed] [Google Scholar]
- 6. Bemelman WA, de Wit LT, Busch OR, Gouma DJ. Hand-assisted laparoscopic splenectomy. Surg Endosc. 2000; 14: 997– 998 [DOI] [PubMed] [Google Scholar]
- 7. Iwase K, et al. Hand-assisted laparoscopic splenectomy for idiopathic thrombocytopenia purpura during pregnancy. Surg Laparosc Endosc Percutan Tech. 2001; 11 ( 1): 53– 56 [PubMed] [Google Scholar]
- 8. Klinger PJ, Smith SL, Abendstein BJ, Hinder RA. Hand-assisted laparoscopic splenectomy for isolated splenic metastasis from an ovarian carcinoma. Surg Laparosc Endosc. 1998; 8 ( 1): 49– 54 [PubMed] [Google Scholar]
- 9. Gharaibeh KIA. Laparoscopic excision of splenic hydatid cyst. Postgrad Med J. 2001; 77: 195– 196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Greene AK, Hodin RA. Laparoscopic splenectomy for massive splenomegaly using a Lahey bag. Amer J Surg. 2001; 181: 543– 546 [DOI] [PubMed] [Google Scholar]
- 11. O'Reilly MJ, Saye WB, Mullins SG, Pinto SE, Falkner PT. Technique of hand-assisted laparoscopic surgery, J Laparosc Surg. 1996; 6 ( 4): 239– 244 [DOI] [PubMed] [Google Scholar]
- 12. Romanelli JR, Kelly JJ, Litwin DEM. Hand-assisted laparoscopic surgery in the United States: An overview. Semin Laparosc Surg. 2001; 8 ( 2): 96– 103 [PubMed] [Google Scholar]
- 13. Southern Surgeons Club Study Group Handoscopic surgery. Arch Surg. 1999; 134: 477– 486 [PubMed] [Google Scholar]