Abstract
Objective:
Laparoscopic repair of ventral incisional hernias is feasible and safe. Polypropylene mesh is often preferred because of its ease of handling and lower cost. Complications like adhesion and fistula formation can occur. The goal of this study was to determine whether bowel adhesions and their attendant complications could be prevented by interposition of omentum.
Methods:
Thirty patients underwent laparoscopic ventral incisional hernias repair with polypropylene mesh. Omentum was always positioned over the loops of bowel for protection. At a mean follow-up of 14 months, 20 patients underwent ultrasonic examination using the previously described visceral slide technique to detect adhesions.
Results:
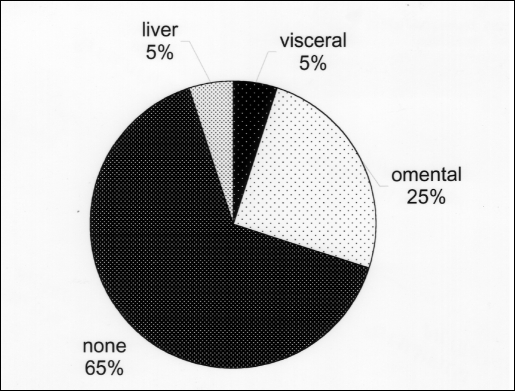
The mean size of the hernias in the study was 50.3 cm2, and the mean size of the mesh applied was 275 cm2. Thirteen patents (65%) had no sonographically detectable adhesions. Five patients demonstrated adhesions between the mesh and omentum, 1 patient developed adhesions between the left lobe of the liver and the mesh, and only 1 case of bowel adhesion to the edge of the mesh was found.
Conclusion:
Laparoscopic ventral incisional hernias repair with polypropylene mesh and omental interposition is not associated with visceral adhesions in the majority of patients. Polypropylene mesh can be used safely when adequate omental coverage is available.
Keywords: Laparoscopy, Incisional herniorrhaphy, Mesh, Ultrasound
INTRODUCTION
Laparoscopic ventral incisional hernia (VIH) repair has gained wide acceptance and increased popularity over the past decade. Multiple studies have documented the safety, technical feasibility, and efficacy of this technique.1–5 The extremely low rate of wound infection and recurrence are among the most important advantages of the laparoscopic approach. Because the prosthetic mesh is placed intraabdominally, many surgeons use expanded polytetrafluoroethylene (ePTFE) grafts because of the low adhesive potential.2–4,6,7 High cost, inferior handling characteristics, and poor incorporation into the tissues are among the drawbacks of ePTFE mesh. Another product, polypropylene (PP) mesh has been used by some authors without any immediate deleterious effect.8, 9 Nevertheless, long-term complications, such as severe adhesions, obstruction, and fistula formation, have been reported with PP.10,11 These complications seem to occur when the PP mesh is placed in direct contact with the serosal surface of the bowel. However, if omentum is interposed between the mesh and viscera, adhesions should not involve loops of bowel and should be restricted to omentum only. Using this technique, Franklin et al8 reported no adhesion-related complications in over 170 patients undergoing laparoscopic VIH repair during a 30-month follow-up.
METHODS
Between 1999 and 2001, patients undergoing laparoscopic VIH repair were prospectively enrolled in a surgical database. In 30 patients, PP mesh (Prolene, Ethicon Corporation, Somerville, NJ) was used for the hernia repair; omentum was interposed between the mesh and the underlying bowel. The mesh was secured in place with a hernia stapler along the edges and nonabsorbable transcutaneous sutures at the corners, taking care to ensure that the mesh overlapped the fascial defect by at least 3 cm in each direction. At a mean follow-up of 14 months, all treated patients were offered an abdominal ultrasound examination. Twenty patients agreed and were studied using an Acuson xp/10, 7 MHz linear transducer, supplemented by a curvilinear transducer when appropriate. A visceral slide technique was used specifically to detect adhesions. At the time of follow-up, all patients were also examined for hernia recurrence, wound infection, and seroma formation. Satisfaction with the procedure (completely/somewhat/not satisfied) and pain at the operative site (mild/moderate/severe) were assessed by using a standard questionnaire.
Visceral Slide
The visceral slide technique has been validated in previous studies.12, 13 This method is based on the demonstration of intestinal movement at the abdominal wall interface during real-time ultrasound imaging. Such movement may occur spontaneously as a result of respiratory excursions or may be induced by manual compression. During longitudinal surface scanning, a normal spontaneous visceral slide may range from 2 cm to more than 5 cm in distance. Detection of a visceral slide that measures less than 1cm is considered abnormal due to adhesions.
RESULTS
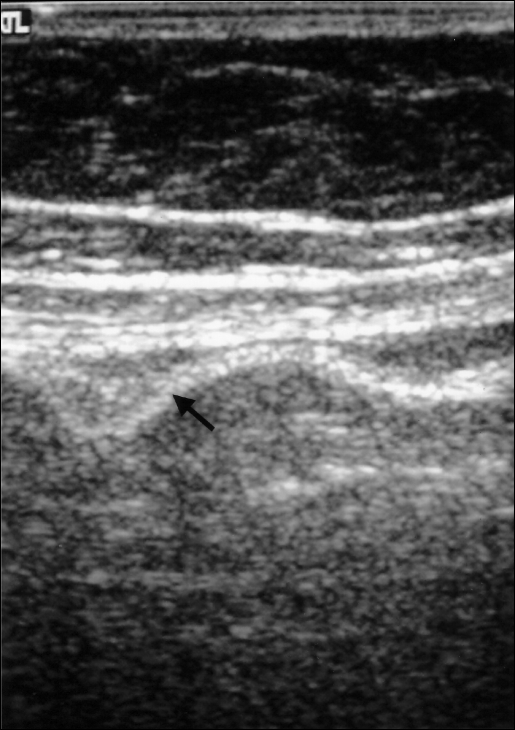
The demographics of all patients undergoing ultrasonic examination are specified in Table 1. No detectable omental or bowel adhesions were found in more than half of the patients (Figure 1). In some cases, mesh appeared to be somewhat corrugated, but normal visceral slide was detected in each instance (Figure 2). Five patients had omentum that appeared to be densely adherent to the PP mesh, as detected by the lack of a normal visceral slide. In one of these patients, the bowel was visibly tethered underneath the omentum but was not adherent to the mesh. One patient had tethered bowel at the edge of the hernia repair with thickened omentum underlying the mesh. In another patient, the left lobe of the liver appeared to be adherent to the mesh. The falci-form ligament had been divided to complete the hernia repair in that case. No infections were noted.
Table 1.
Patient Demographics
| Female/Male | 18/2 |
| Age (yrs) | 52 (28–74) |
| Mean BMI | 34.9 (23.9–47.8) |
| ASA II/III | 15/5 |
| Recurrent | 7 (35%) |
| Mean Size of Hernia (cm) | 50.3 (6–171) |
| Mean Size of Mesh (cm) | 275 (64–760) |
| Mean Length of Stay (days) | 1.9 (1–4) |
| Return of Bowel Function (days) | 1.6 (1–3) |
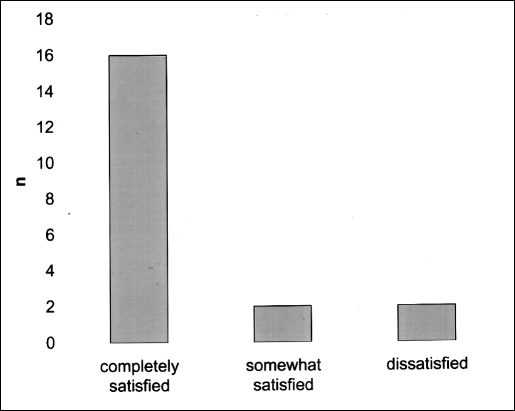
Figure 1.
The incidence of adhesions (%) detected by ultra-sonography in 20 patents after laparoscopic ventral incisional hernia repair with polypropylene mesh and omental interposition.
Figure 2.
Ultrasonogram of the patient after laparoscopic ventral incisional hernia repair: mesh (arrow) appears to be corrugated. No seroma or recurrence is detected.
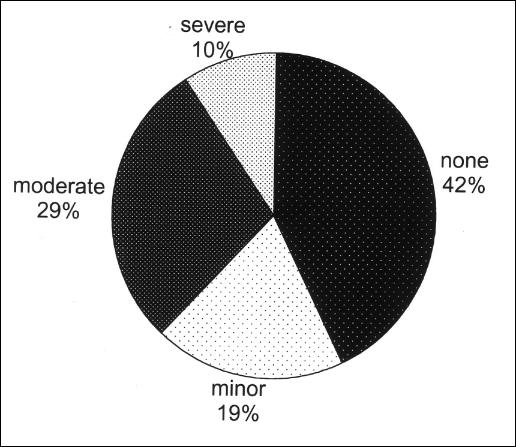
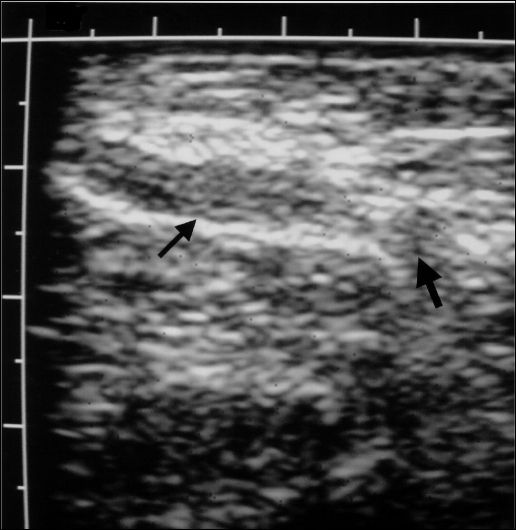
Nine patients had no pain at the surgery site, while 10 patients stated they experienced mild to moderate pain with activity, usually near the edges of the repair (Figure 3). Only 2 patients complained of severe pain at the site of repair. One of these patients described severe pain with activity even though she had been pain-free for 1 year after surgery. This patient was noted to have a small recurrence of the hernia just lateral to the edge of the mesh (Figure 4). Her initial repair 3 years earlier was accomplished using the separation of components technique, which led to a subsequent recurrence. The mesh used for this repair measured 760 cm. The patient refused further surgery.
Figure 3.
The incidence of persistent postoperative pain (%) at the repair site.
Figure 4.
Ultrasonogram of the patient with the recurrent hernia: omental herniation (thick arrow) is seen just lateral to the mesh (thin arrow).
The results of the satisfaction survey are shown in Figure 5. The reasons for less than complete satisfaction include unexpected postoperative pain in 1 patient and moderate crampy postoperative pain in a second patient. One patient had problems with a trocar site, and another patient felt that an area of attenuated fascia with underlying mesh constituted a recurrence.
Figure 5.
The results of the satisfaction survey following laparoscopic ventral incisional hernia repair.
DISCUSSION
The use of prosthetic materials for the repair of a ventral incisional hernia has significantly decreased the number of recurrences for this condition. Moreover, the laparoscopic approach has helped to reduce the number of infections, recurrences, and the length of hospital stay.1, 2, 7, 14
Polypropylene is easier to handle intraoperativly and less costly than ePTFE. It has good tensile strength and tissue integration. However, expedient tissue integration may produce clinically significant adhesion formation and enterocutaneous fistulization. The formation of adhesions has been studied in numerous experimental models. In 1 such study, increasing adhesion development was noted from day 1 to day 7 after placement of the prosthesis, but surfaces that were already covered with mesothelial cells did not show progression. Thereafter, the bowel had a diminished tendency to form adhesions even in the absence of omentum.15 Another animal model was used to compare adhesion formation after open and laparoscopic placement of mesh. The study demonstrated that the area of mesh covered with adhesions and the grade of the adhesions were significantly greater in both groups undergoing celiotomy compared with the adhesion formation in the laparoscopic group. On histologic examination, the vascularity of the animals that underwent incision through skin and fascia was increased and slower to regress than in the laparoscopically treated animals.16
In the clinical setting, PP mesh has been used previously for open VIH repair with a very low rate of enterocutaneous fistula formation,9 but fistulas have been reported as late as 15 years after the procedure.10 In laparoscopic VIH repair, PP has been combined with omental interposition as protection against bowel adhesions. No complications were reported during up to 84 months of follow-up.8 Colocutaneous fistula after laparoscopic VIH hernia repair with intraperitoneal PTFE has also been reported; in this case, the laparoscopic staples or external postoperative trauma may have played a role.7
The present study used the omental interposition technique as well. Ultrasound was used to detect adhesion formation at a time when this process was complete. Visceral slide detection by ultrasound was described by Kodama et al13 in 1992 and was again validated in a French study12 with intraoperative observation and was noted to have a sensitivity of 77%, specificity of 74%, and a negative predictive value of 84%.
The data in our study were prospectively collected, but the overall number of patients was modest. Nonetheless, a low recurrence and infection rate was confirmed as noted in other laparoscopic herniorrhaphy studies, and no mesh-related complications have been noted to date. Only 1 case of bowel adhesions to the edge of the mesh was found using ultrasound scanning at 24-month follow-up. This could be related to inadequate omental protection. Sixty-five percent of our patients did not have adhesions of bowel or omentum detectable on ultra-sound examination. This result is similar to that reported by Franklin et al8 where two thirds of the patients had few or no adhesions. Laparoscopic ventral incisional hernia repair appears to decrease adhesion formation. A decreased inflammatory response in the abdominal wall tissue might limit the inflammatory tissue reaction caused by the PP mesh in regards to adhesion with underlying viscera.
The results of this study are important but somewhat limited by the fact that the results of individual sonographic examinations could not be independently verified. The negative predictive value of the visceral slide method is approximately 80%; therefore, it is possible that some patients who were deemed free of adhesions might indeed have had mild or filmy adhesions not detectable by ultrasound. In any case, these adhesions, even if present are unlikely to have any clinical impact, because no visceral complications have been observed.
Late postoperative pain seemed to be mostly related to the suture points during strenuous activity. Although it was noted by half of the patients, it usually did not require medication and did not interfere with work or recreational activities. Still, postoperative pain management remains an important aspect of laparoscopic VIH repair. We have now gone to the use of absorbable monofilament material for the transfascial sutures.
CONCLUSION
Our early results indicate that laparoscopic ventral incisional hernia repair with PP mesh and omental coverage is not associated with sonographically detectable visceral adhesions in most patients. Moreover, visceral complications such as bowel obstruction or enterocutaneous fistula do not occur. Further accrual of patients and careful follow-up is needed to better understand the problem of ventral hernias and their repair with mesh.
Acknowledgments:
The study was supported by a grant from the San Antonio Area Foundation and an educational grant from the Ethicon Corporation.
Contributor Information
Juliane Bingener, Department of Surgery, University of Texas Health Science Center, San Antonio, Texas, USA..
George B. Kazantsev, Department of Surgery, University of Texas Health Science Center, San Antonio, Texas, USA..
Shailendra Chopra, Department of Radiology, University of Texas Health Science Center, San Antonio, Texas, USA..
Wayne H. Schwesinger, Department of Surgery, University of Texas Health Science Center, San Antonio, Texas, USA..
References:
- 1. Heniford BT, Park A, Ramshow BJ, Voeller G. Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg. 2000;190:645–650 [DOI] [PubMed] [Google Scholar]
- 2. Holzman MD, Purut CM, Reintgen K, Eubanks S, Papas TN. Laparoscopic ventral and incisional hernioplasty. Surg Endosc. 1997;11:32–35 [DOI] [PubMed] [Google Scholar]
- 3. Park A, Birch DW, Lovrics P. Laparoscopic and open incisional hernia repair: a comparison study. Surgery. 1998;124:816–822 [DOI] [PubMed] [Google Scholar]
- 4. Ramshaw BJ, Esartia P, Schwab J, et al. Comparison of laparoscopic and open ventral hernioraphy. Am Surg. 1999;65:827–832 [PubMed] [Google Scholar]
- 5. Toy FK, Bailey RW, Carey S, et al. Prospective, multicenter study of laparoscopic ventral hernioplasty. Surg Endosc. 1998;12:955–959 [DOI] [PubMed] [Google Scholar]
- 6. Condon RE, DeBord JR. Expanded polytetrafluoroethylene prosthetic patches in repair in large ventral hernia. In: Nyhus LM, Condon RE. eds. Hernia. 4th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1995:328–336 [Google Scholar]
- 7. DeMaria EJ, Moss JM, Sugerman HJ. Laparoscopic intraperitoneal polytetrafluoroethylene (PTFE) prosthetic patch repair of ventral hernia. Surg Endosc. 2000;14:326–329 [DOI] [PubMed] [Google Scholar]
- 8. Franklin ME, Dorman JP, Glass JL, Balli JE, Gonzales JJ. Laparoscopic ventral and incisional hernia repair. Surg Laparosc Endosc. 1998;8:294–299 [PubMed] [Google Scholar]
- 9. Vrijland WW, Jeekel J, Steyerberg EW, den Hoed PT, Bonjer HJ. Intraperitoneal polypropylene mesh repair of incisional hernia is not associated with enterocutaneous fistula. Br J Surg. 2000;87:348–352 [DOI] [PubMed] [Google Scholar]
- 10. DeGuzman LJ, Nyhus LM, Yared G, Schlesinger PK. Colocutaneous fistula formation following polypropylene mesh placement for repair of a ventral hernia: Diagnosis by colonoscopy. Endoscopy. 1995;27:459–461 [DOI] [PubMed] [Google Scholar]
- 11. Leber GE, Garb JL, Alexander AI, Reed WP. Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg. 1998;133:378–382 [DOI] [PubMed] [Google Scholar]
- 12. Balique JG, Alexandre JH, Arnaud JP, et al. Intraperitoneal treatment of incisional and umbilical hernias: intermediate results of a multicenter prospective clinical trial using an innovative composite mesh. Hernia. 2000;4(suppl):10–16 [DOI] [PubMed] [Google Scholar]
- 13. Kodama I, Loiacona LA, Sigel B, et al. Ultrasonic detection of visceral slide as an indicator of abdominal wall adhesions. J Clin Ultrasound. 1992;20:375–380 [DOI] [PubMed] [Google Scholar]
- 14. Hesselink VJ, Luijedndijk RW, de Wilt JHW, Heide R, Jeekel J. An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet. 1993;176:228–234 [PubMed] [Google Scholar]
- 15. Baptista ML, Bonsack ME, Felemovicius I, Delaney JP. Abdominal adhesions to prosthetic mesh evaluated by laparoscopy and electron microscopy. J Am Coll Surg. 2000;190:271–280 [DOI] [PubMed] [Google Scholar]
- 16. Garrard CL, Clements RH, Nanney L, Davidson JM, Richards WO. Adhesion formation is reduced after laparoscopic surgery. Surg Endosc. 1999;13:10–13 [DOI] [PubMed] [Google Scholar]