Abstract
Blood glucose, glucose tolerance, serum insulin, free fatty acids in serum, plasma noradrenaline, and plasma adrenaline were measured in 10 patients with acute myocardial infarction (AMI) as well as in healthy subjects. Both noradrenaline and adrenaline in plasma were elevated in patients with AMI, the level being fairly constant in the individual patients and dependent on their degree of illness.
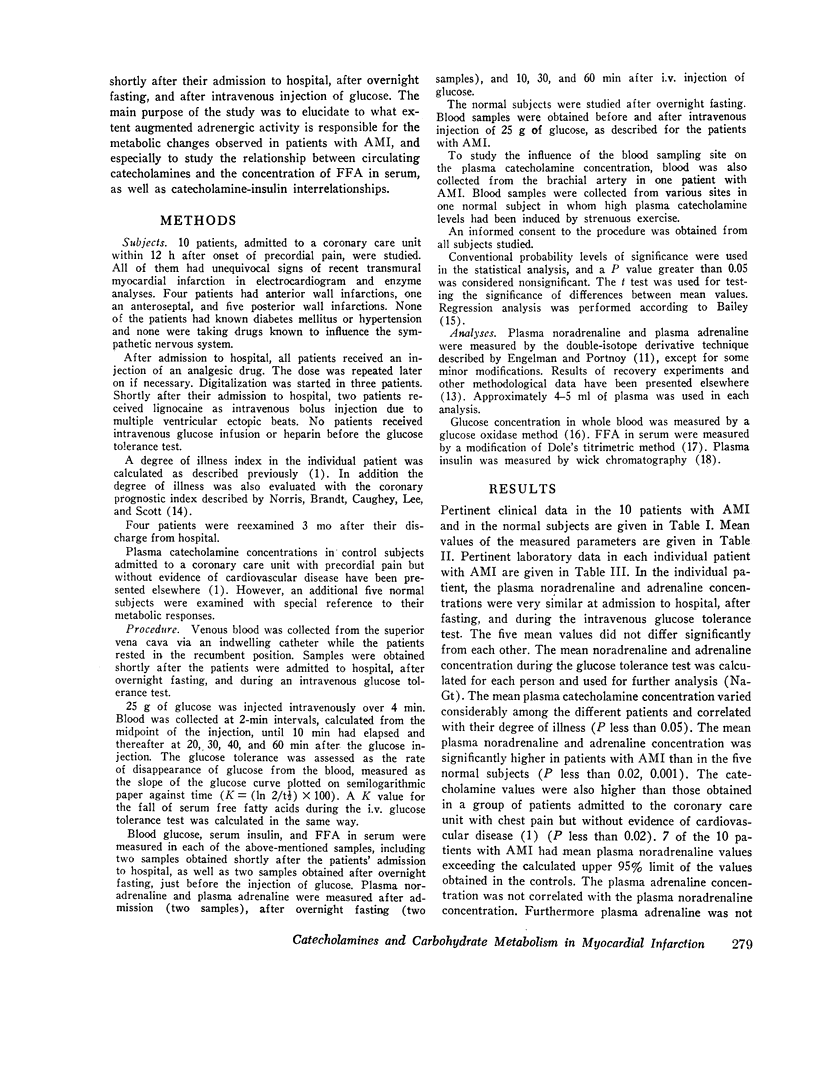
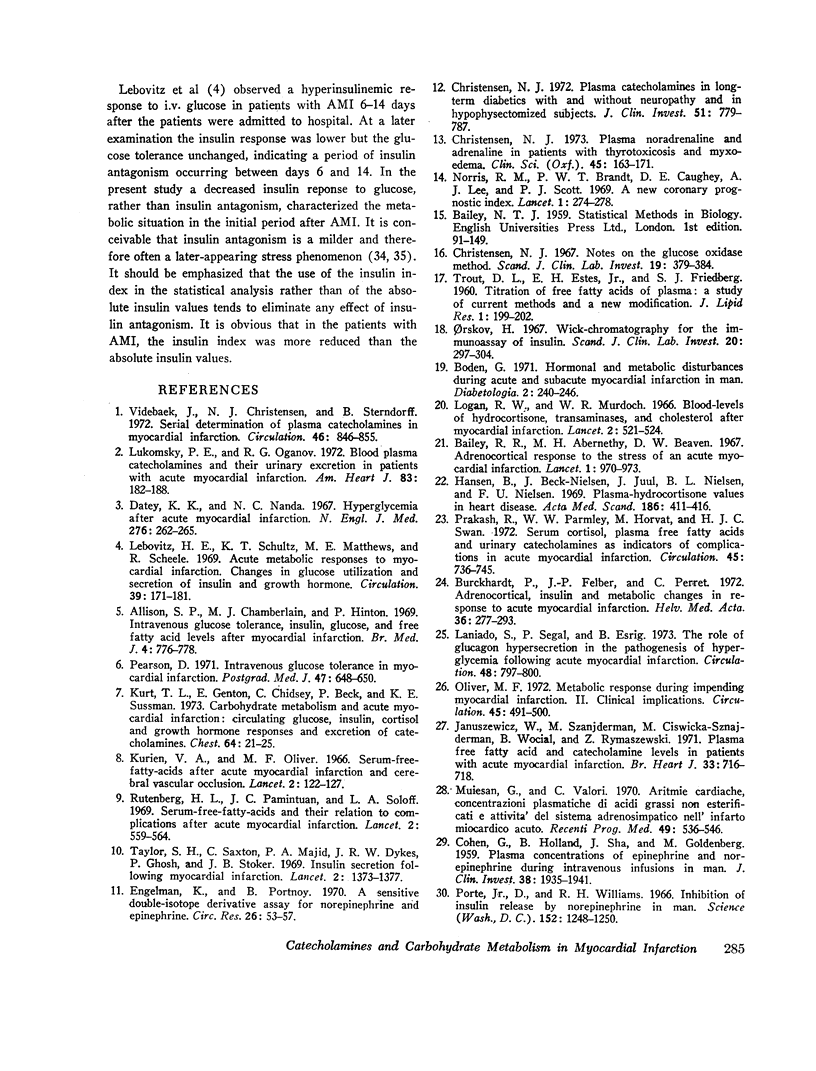
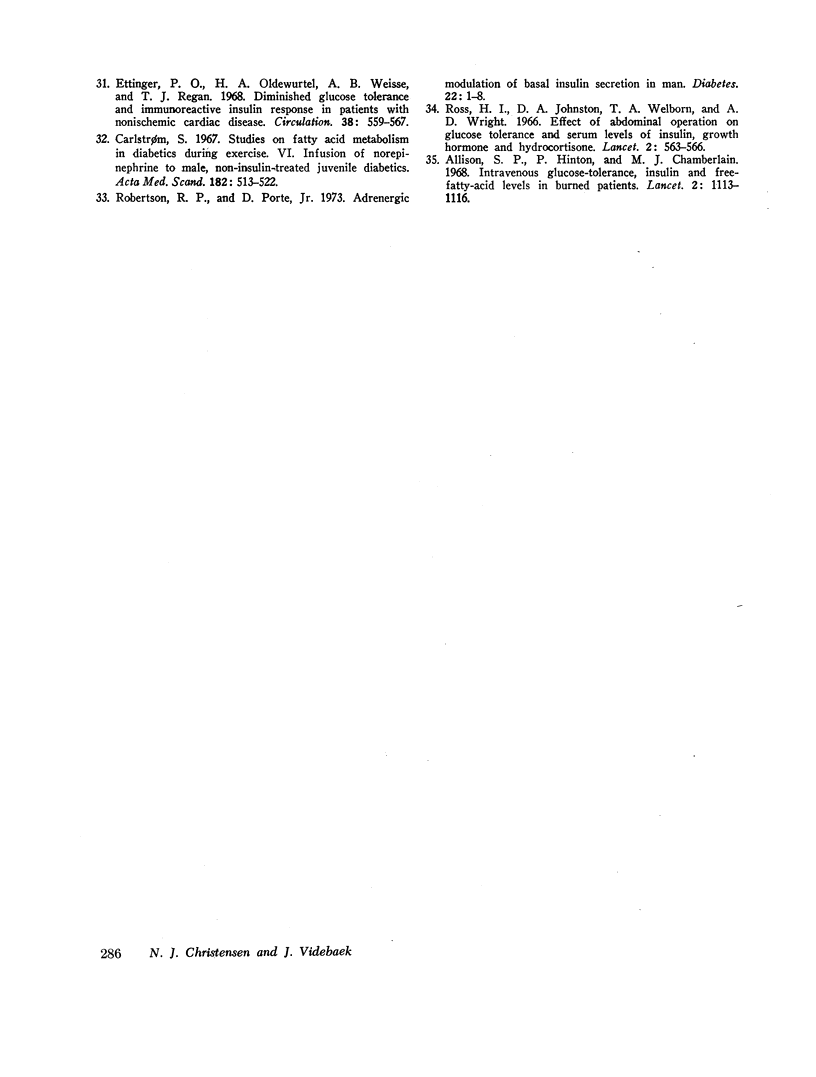
In the fasting state, blood glucose, serum insulin, and free fatty acids were elevated in patients with AMI. Plasma noradrenaline showed a highly significant correlation with the fasting blood glucose concentration, but not with serum insulin or free fatty acids. The concentration of free fatty acids in serum could be predicted only if both plasma noradrenaline and the basal insulin concentration were known.
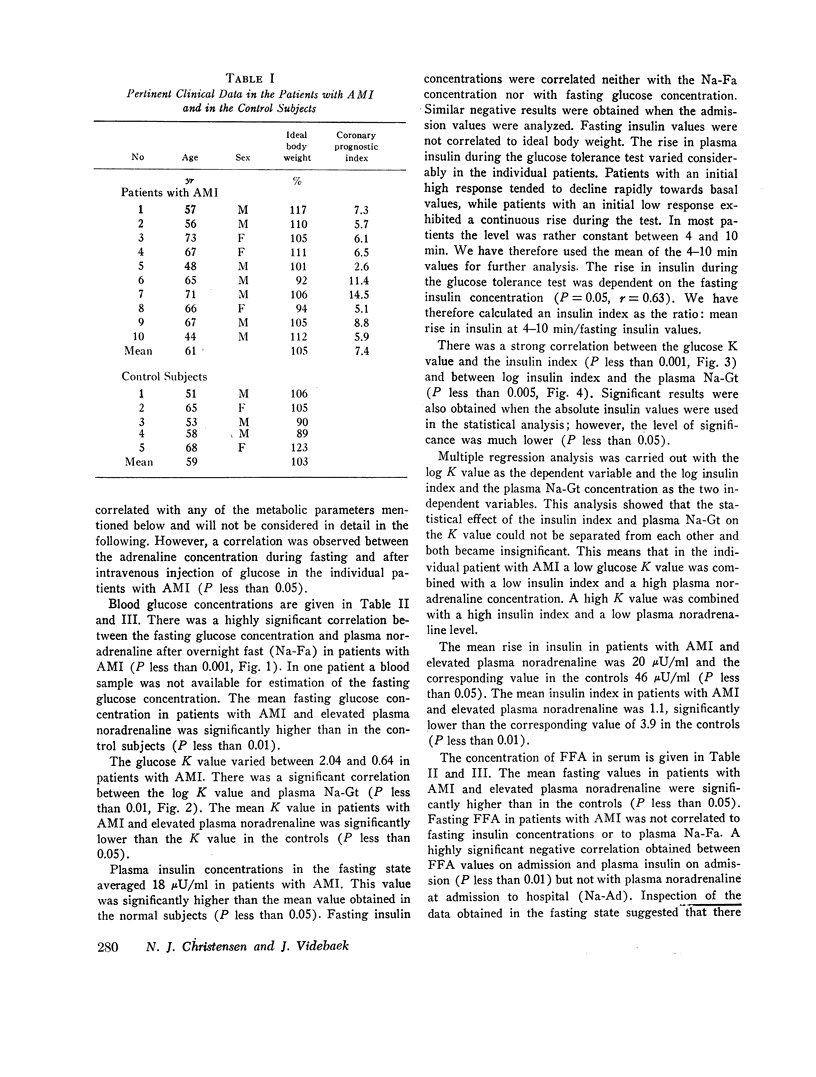
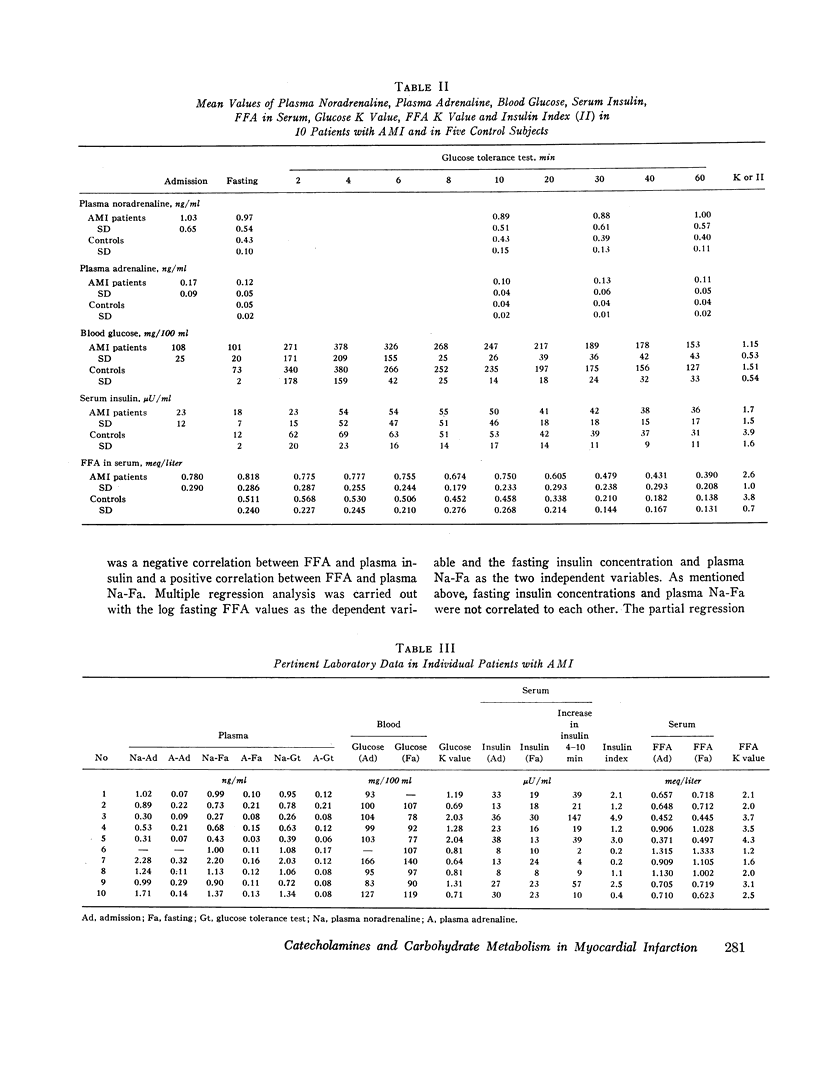
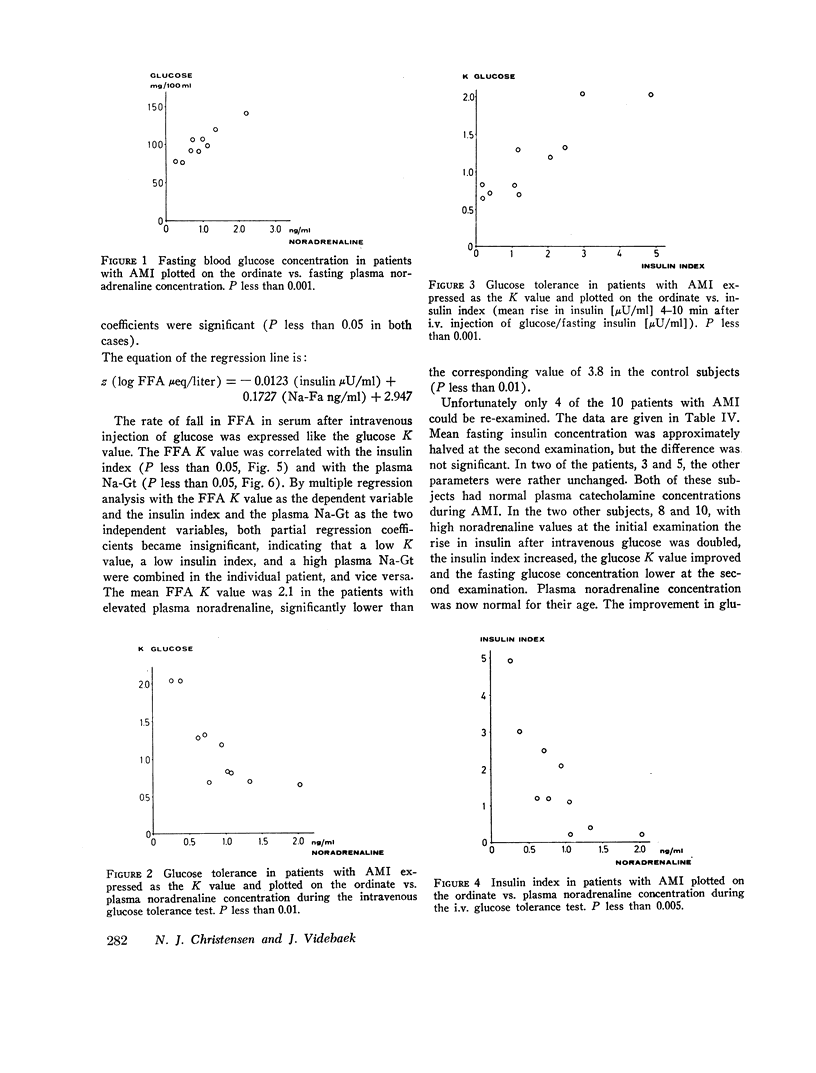
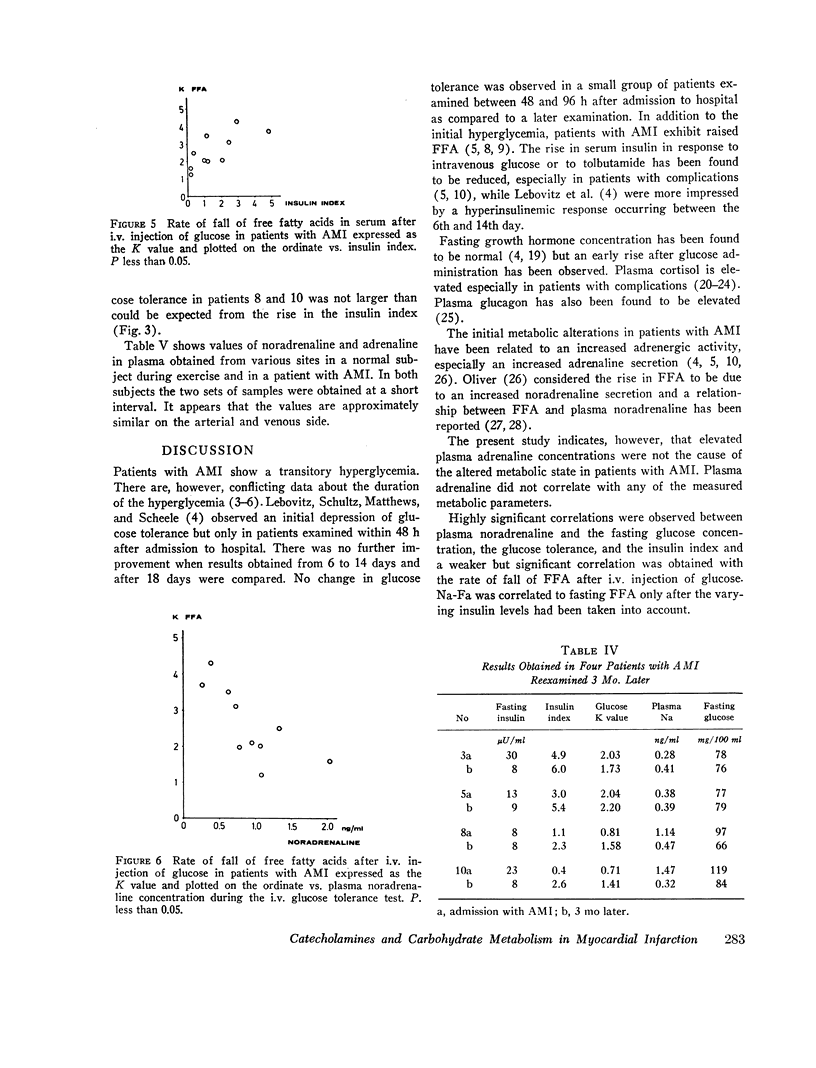
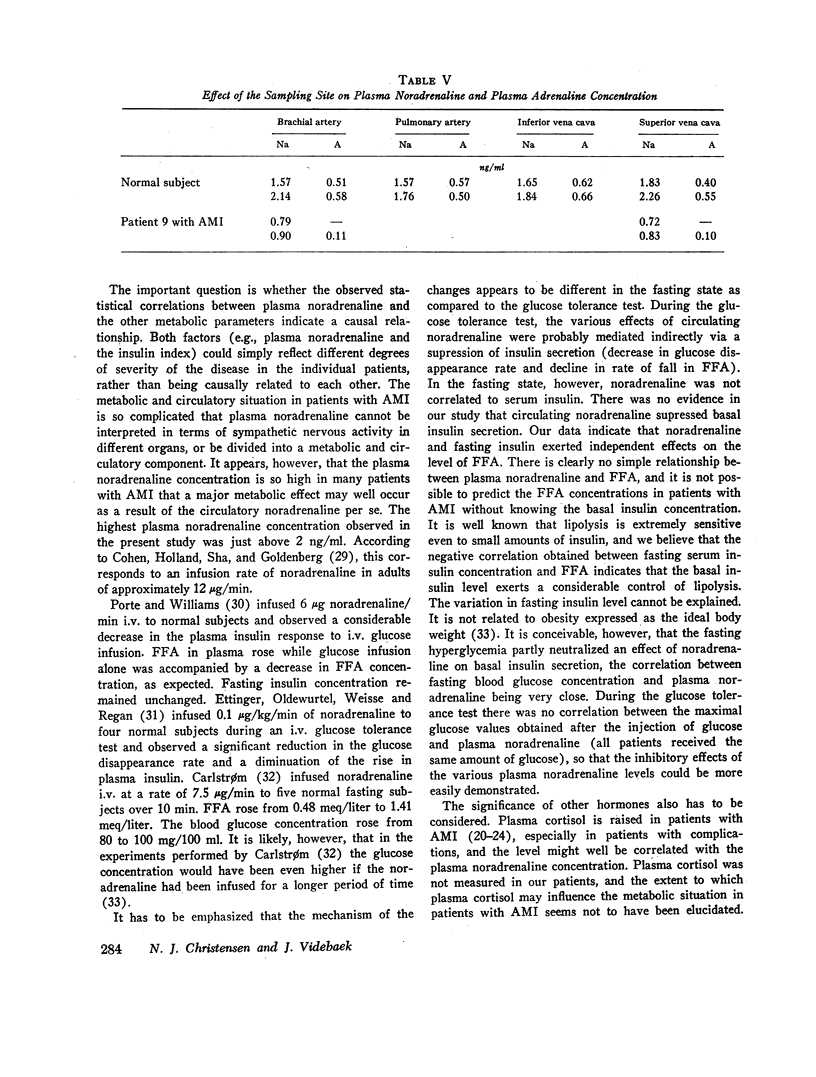
Intravenous glucose tolerance was reduced in patients with AMI, especially in patients with high plasma noradrenaline and a low initial rise in insulin. There was a significant negative correlation between the initial rise in insulin expressed in percentage of the basal insulin concentration and the plasma noradrenaline level. The statistical effects of serum insulin and plasma noradrenaline on the glucose tolerance could not be separated from each other. The decline in free fatty acids after intravenous injection of glucose showed a negative correlation with plasma noradrenaline and a positive correlation with the initial rise in insulin.
Plasma adrenaline did not correlate with any of the metabolic parameters mentioned above.
The plasma noradrenaline concentration was elevated to such a degree in patients with AMI that the observed changes in metabolism might have been caused directly by the circulating noradrenaline.
During the glucose tolerance tests, the effects of noradrenaline was probably carried out indirectly via a suppression of insulin secretion. It is conceivable that any effect of plasma noradrenaline on the basal insulin secretion was neutralized by the fasting hyperglycemia.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allison S. P., Chamberlain M. J., Hinton P. Intravenous glucose tolerance, insulin, glucose, and free fatty acid levels after myocardial infarction. Br Med J. 1969 Dec 27;4(5686):776–778. doi: 10.1136/bmj.4.5686.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison S. P., Hinton P., Chamberlain M. J. Intravenous glucose-tolerance, insulin, and free-fatty-acid levels in burned patients. Lancet. 1968 Nov 23;2(7578):1113–1116. doi: 10.1016/s0140-6736(68)91581-x. [DOI] [PubMed] [Google Scholar]
- Bailey R. R., Abernethy M. H., Beaven D. W. Adrenocartical response to the stress of an acute myocardial infarction. Lancet. 1967 May 6;1(7497):970–973. doi: 10.1016/s0140-6736(67)92356-2. [DOI] [PubMed] [Google Scholar]
- Boden G. Hormonal and metabolic disturbances during acute and subacute myocardial infarction in man. Diabetologia. 1971 Aug;7(4):240–246. doi: 10.1007/BF01211875. [DOI] [PubMed] [Google Scholar]
- Burckhardt P., Felber J. P., Perret C. Adrenocortical, insulin and metabolic changes in response to acute myocardial infarction. Helv Med Acta. 1972;36(4):277–293. [PubMed] [Google Scholar]
- COHEN G., HOLLAND B., SHA J., GOLDENBERG M. Plasma concentrations of epinephrine and norepinephrine during intravenous infusions in man. J Clin Invest. 1959 Nov;38:1935–1941. doi: 10.1172/JCI103972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlström S. Studies on fatty acid metabolism in diabetics during exercise. VI. Infusions of norepinephrine to male, non-insulin-treated, juvenile diabetics. Acta Med Scand. 1967 Oct;182(4):513–522. [PubMed] [Google Scholar]
- Christensen N. J. Notes on the glucose oxidase method. Scand J Clin Lab Invest. 1967;19(4):379–384. doi: 10.3109/00365516709090653. [DOI] [PubMed] [Google Scholar]
- Christensen N. J. Plasma catecholamines in long-term diabetics with and without neuropathy and in hypophysectomized subjects. J Clin Invest. 1972 Apr;51(4):779–787. doi: 10.1172/JCI106872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen N. J. Plasma noradrenaline and adrenaline in patients with thyrotoxicosis and myxoedema. Clin Sci Mol Med. 1973 Aug;45(2):163–171. doi: 10.1042/cs0450163. [DOI] [PubMed] [Google Scholar]
- Datey K. K., Nanda N. C. Hyperglycemia after acute myocardial infarction. Its relation to diabetes mellitus. N Engl J Med. 1967 Feb 2;276(5):262–265. doi: 10.1056/NEJM196702022760504. [DOI] [PubMed] [Google Scholar]
- Engelman K., Portnoy B. A sensitive double-isotope derivative assay for norepinephrine and epinephrine. Normal resting human plasma levels. Circ Res. 1970 Jan;26(1):53–57. doi: 10.1161/01.res.26.1.53. [DOI] [PubMed] [Google Scholar]
- Ettinger P. O., Oldewurtel H. A., Weisse A. B., Regan T. J. Diminished glucose tolerance and immunoreactive insulin response in patients with nonischemic cardiac disease. Circulation. 1968 Sep;38(3):559–567. doi: 10.1161/01.cir.38.3.559. [DOI] [PubMed] [Google Scholar]
- Hansen B., Beck-Nielsen J., Juul J., Nielsen B. L., Nielsen F. U. Plasma-hydrocortisone values in heart disease. Results after acute myocardial infarction (with and without cardiogenic shock) and in patients with congestive heart failure. Acta Med Scand. 1969 Nov;186(5):411–416. [PubMed] [Google Scholar]
- Januszewicz W., Sznajderman M., Ciswicka-Sznajderman M., Wocial B., Rymaszewski Z. Plasma free fatty acid and catecholamine levels in patients with acute myocardial infarction. Br Heart J. 1971 Sep;33(5):716–718. doi: 10.1136/hrt.33.5.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurien V. A., Oliver M. F. Serum-free-fatty-acids after acute myocardial infarction and cerebral vascular occlusion. Lancet. 1966 Jul 16;2(7455):122–127. doi: 10.1016/s0140-6736(66)92420-2. [DOI] [PubMed] [Google Scholar]
- Kurt T. L., Genton E., Chidsey C., 3rd, Beck P., Sussman K. E. Carbohydrate metabolism and acute myocardial infarction: circulating glucose, insulin, cortisol and growth hormone responses and excretion of catecholamines. Chest. 1973 Jul;64(1):21–25. doi: 10.1378/chest.64.1.21. [DOI] [PubMed] [Google Scholar]
- Lebovitz H. E., Shultz K. T., Matthews M. E., Scheele R. Acute metabolic responses to myocardial infarction. Changes in glucose utilization and secretion of insulin and growth hormone. Circulation. 1969 Feb;39(2):171–181. doi: 10.1161/01.cir.39.2.171. [DOI] [PubMed] [Google Scholar]
- Logan R. W., Murdoch W. R. Blood-levels of hydrocortisone, transaminases, and cholesterol after myocardial infarction. Lancet. 1966 Sep 3;2(7462):521–524. doi: 10.1016/s0140-6736(66)92880-7. [DOI] [PubMed] [Google Scholar]
- Lukomsky P. E., Oganov R. G. Blood plasma catecholamines and their urinary excretion in patients with acute myocardial infarction. Am Heart J. 1972 Feb;83(2):182–188. doi: 10.1016/0002-8703(72)90137-8. [DOI] [PubMed] [Google Scholar]
- Muiesan G., Valori C. Aritmie cardiache, concentrazioni plasmatiche di acidi grassi non esterificati e attivita' del sistema adrenosimpatico nell'infarto miocardico acuto. Recenti Prog Med. 1970 Dec;49(6):536–545. [PubMed] [Google Scholar]
- Norris R. M., Brandt P. W., Caughey D. E., Lee A. J., Scott P. J. A new coronary prognostic index. Lancet. 1969 Feb 8;1(7589):274–278. doi: 10.1016/s0140-6736(69)91035-6. [DOI] [PubMed] [Google Scholar]
- Oliver M. F. Metabolic response during impending myocardial infarction. II. Clinical implications. Circulation. 1972 Feb;45(2):491–500. doi: 10.1161/01.cir.45.2.491. [DOI] [PubMed] [Google Scholar]
- Pearson D. Intravenous glucose tolerance in myocardial infarction. Postgrad Med J. 1971 Oct;47(552):648–650. doi: 10.1136/pgmj.47.552.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porte D., Jr, Williams R. H. Inhibition of insulin release by norepinephrine in man. Science. 1966 May 27;152(3726):1248–1250. doi: 10.1126/science.152.3726.1248. [DOI] [PubMed] [Google Scholar]
- Prakash R., Parmley W. W., Horvat M., Swan H. J. Serum cortisol, plasma free fatty acids, and urinary cathecholamines as indicators of complications in acute myocardial infarction. Circulation. 1972 Apr;45(4):736–745. doi: 10.1161/01.cir.45.4.736. [DOI] [PubMed] [Google Scholar]
- Robertson R. P., Porte D., Jr Adrenergic modulation of basal insulin secretion in man. Diabetes. 1973 Jan;22(1):1–8. doi: 10.2337/diab.22.1.1. [DOI] [PubMed] [Google Scholar]
- Ross H., Johnston I. D., Welborn T. A., Wright A. D. Effect of abdominal operation on glucose tolerance and serum levels of insulin, growth hormone, and hydrocortisone. Lancet. 1966 Sep 10;2(7463):563–566. doi: 10.1016/s0140-6736(66)93036-4. [DOI] [PubMed] [Google Scholar]
- Rutenberg H. L., Pamintuan J. C., Soloff L. A. Serum-free-fatty-acids and their relation to complications after acute myocardial infarction. Lancet. 1969 Sep 13;2(7620):559–564. doi: 10.1016/s0140-6736(69)90261-x. [DOI] [PubMed] [Google Scholar]
- TROUT D. L., ESTES E. H., Jr, FRIEDBERG S. J. Titration of free fatty acids of plasma: a study of current methods and a new modification. J Lipid Res. 1960 Apr;1:199–202. [PubMed] [Google Scholar]
- Taylor S. H., Saxton C., Majid P. A., Dykes J. R., Ghosh P., Stoker J. B. Insulin secretion following myocardial infarction with particular respect to the pathogenesis of cardiogenic shock. Lancet. 1969 Dec 27;2(7635):1373–1378. doi: 10.1016/s0140-6736(69)90928-3. [DOI] [PubMed] [Google Scholar]
- Videbaek J., Christensen N. J., Sterndorff B. Serial determination of plasma catecholamines in myocardial infarction. Circulation. 1972 Nov;46(5):846–855. doi: 10.1161/01.cir.46.5.846. [DOI] [PubMed] [Google Scholar]



