Abstract
Background:
Gangrenous cholecystitis is a severe form of acute cholecystitis with high morbidity. This study investigate the outcomes for patients undergoing cholecystectomy for gangrenous cholecystitis in the decade before and after the introduction of laparoscopic technology at our institution.
Methods:
From 1982 to 2002, all patients undergoing cholecystectomy for gangrenous cholecystitis were prospectively entered into a database. Demographic data, method of surgery, and outcome variables were assessed and compared over time.
Results:
Cholecystectomy was performed to treat gangrenous cholecystitis in 238 patients (mean age, 54 years). From 1982 to 1992, 98 patients underwent cholecystectomy for gangrenous cholecystitis, and from 1992 to 2002, 140 patients underwent the procedure. Ninety-seven patients underwent laparoscopic cholecystectomy, and 33 patients (34%) required conversion. The open and laparoscopic cholecystectomy group differed in the number of intensive care unit admissions (13% vs. 5%, P<0.05), overall length of hospital stay (10 vs. 5.7 days, P<0.001) and rate of intraabdominal abscesses (8% vs. 0.7%).
Conclusion:
Gangrenous cholecystitis remains a disease with high morbidity. Laparoscopic cholecystectomy shortened hospital stay and can be offered without increasing morbidity. Methods to decrease intraabdominal abscess formation in patients undergoing laparoscopic cholecystectomy for gangrenous cholecystitis are needed.
Keywords: Laparoscopy, Cholecystectomy, Acute cholecystitis, Gangrenous cholecystitis
INTRODUCTION
Gangrenous cholecystitis is one of the most severe forms of acute cholecystitis and is encountered in 2% to 39% of patients with acute cholecystitis.1–12 The optimal surgical treatment of gangrenous cholecystitis is controversial. Earlier studies question the role of laparoscopic cholecystectomy,4,5 but more recent studies show improved outcomes when the procedure is feasible.6–8,10
This study was undertaken to determine the impact of laparoscopic cholecystectomy in the treatment of gangrenous cholecystitis, evaluating outcomes in the decade before and after its introduction in clinical practice.
METHODS
Between 1982 and 2002, data from all patients with gangrenous cholecystitis undergoing cholecystectomy at the Bexar County Hospital in San Antonio, Texas or at the South Texas Veteran Health Care System were prospectively collected in a database. Sex, age, race, American Society of Anesthesia (ASA) preoperative classification, year, type and duration of the procedure (primary open vs laparoscopic approach), morbidity, mortality, and length of hospital stay were recorded. These data were analyzed and compared over time. The diagnosis of gangrenous cholecystitis was based on operative findings. We excluded patients who underwent another operation at the same time, such as interventions for perforated peptic ulcer. Complications were classified according to Clavien:13 grade I complications are defined as requiring bedside interventions only, grade II requiring an invasive procedure, grade III complications leading to a permanent disability, and grade IV death.13 Patients who underwent conversion from the laparoscopic to the open procedure were included in the initial laparoscopic cholecystectomy group in an intention to treat analysis. Statistical calculations were performed using the unpaired Student t test, chi-square, and Fisher's exact tests where appropriate. The study was exempt from the Institutional Review Board.
RESULTS
Between 1982 and 2002, 11,360 patients underwent cholecystectomy at our institutions. During that time, 3752 patients were found to have acute cholecystitis and of those, 238 patients (6.3%) were diagnosed with gangrenous cholecystitis. Seventy-two women and 166 men underwent surgery for gangrenous cholecystitis, a ratio of 1:2.3. The mean age for all patients was 54 years (range, 16 to 87). The mean ASA score for all patients was 2.3 without differences due to sex.
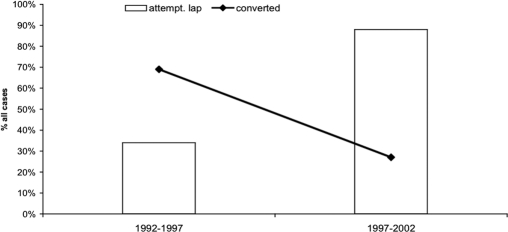
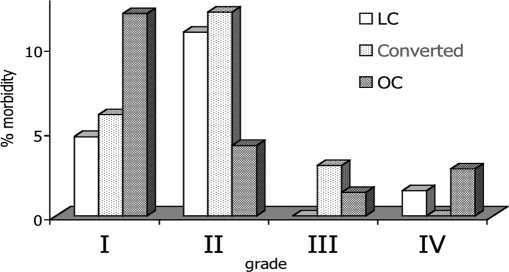
Eighty-four percent of the patients were Hispanic, 16% white, and 0.4% African American. Hispanic patients presented at a significantly younger age with gangrenous cholecystitis than white patients did, had lower ASA scores, and less morbidity and mortality (Table 1). Open cholecystectomy was performed in 141 patients, and in 97 patients, the cholecystectomy was attempted laparoscopically. Conversion to an open procedure was required in 33 (34%) patients. Intense inflammation obscured the anatomy, causing laparoscopic cholecystectomy to be unsafe in 73% of the patients requiring conversion. Nine percent of the patients were converted due to bleeding that could not be controlled adequately and 6% due to an abscess or perforation. One patient (3%) underwent conversion because a cholangiogram could not be performed, one (3%) due to colonic deserosalization, and in 6%, the reason was not documented. The number of patients undergoing laparoscopic cholecystectomy and the conversion rates for the first and second half of the last decade are shown in Figure 1. We identified 55 postoperative complications in 47 patients (Table 2). The morbidity rate was 20.5% for patients undergoing open cholecystectomy, 18.5% for all patients undergoing attempted laparoscopic cholecystectomy, 17% after successful laparoscopic cholecystectomy, and 21% in the converted group (P=NS). Figure 2 demonstrates the distribution of these complications according to their severity as described by Clavien et al.13 Patients who incurred complications were slightly older and exhibited slightly higher ASA scores, but this did not reach statistical significance (56.4 vs. 52.8 years, P=0.14; ASA 2.45 vs. 2.23, P=0.1 respectively). Patients with complications stayed a mean of 15 days in the hospital, while patients without complications stayed 7 days (P<0.01). Patients with bile leaks or intraabdominal abscesses were less likely to have had an IOC during surgery compared with the overall patient group (20% vs. 49.5% respectively; P<0.02).
Table 1.
Patient Demographics by Race
| Hispanic Patients | White Patients | P Value | |
|---|---|---|---|
| Patients (n) | 200 | 37 | |
| Mean Age (yrs) | 52 | 65 | <0.001 |
| Mean ASA | 2.2 | 2.9 | <0.001 |
| Morbidity Overall | 18% | 30% | 0.1 |
| Morbidity First Decade | 12% | 35% | <0.05 |
| Mortality | 1% | 8% | <0.01 |
Figure 1.
Percentage of attempted laparoscopic cholecystectomies in patients with gangrenous cholecystitis and conversion rate over time.
Table 2.
Complications in Patients With Gangrenous Cholecystitis by Operative Method
| Complication | Attempted LC n (%)* | Converted LC n (%)* | OC n (%) | P Value |
|---|---|---|---|---|
| Bile leaks | 6 (6.1%) | 4 (12%) | 4 (2.8%) | 0.2 |
| Cardiorespiratory | 3 (3%) | 1 (3%) | 6 (4.2%) | 0.6 |
| Intraabd. abscess | 7 (7.2%) | 3 (9%) | 1 (0.7%) | <0.01 |
| Ileus | 0 | 0 | 8 (5.7%) | <0.02 |
| Wound infection | 1 (1%) | 1 (3%) | 3 (2.1%) | 0.5 |
| Retained stones | 1 (1%) | 0 | 1 (0.7%) | 0.8 |
| Other | 2 (2%) | 1 (3%) | 7 (4.9%) | 0.1 |
LC=laparoscopic cholecystectomy, OC=open cholecystectomy.
Figure 2.
Morbidity rate by Clavien classification and operative methods in patients presenting with gangrenous cholecystitis from 1982 to 2002.
Five patients died (2%): 4 after open and 1 after laparoscopic cholecystectomy. Four patients died due to sepsis and multiple organ failure. The cause of the fifth patient's death was not available. The ASA score and age in this group of patients was significantly higher than the mean ASA score and age (4.2 vs. 2.23; P<0.001; 74.1 vs. 52.8 years; P<0.001, respectively).
The first and second decade of the study period were examined regarding the presence of preexisting disease, morbidity, mortality, and length of hospital stay (Table 3).
Table 3.
Comparison of Preexisting Disease, Morbidity, Mortality, and Length of Hospital Stay Between the First and Second Decade of the Study Period
| 1982 to 1992 | 1992 to 2002 | P Value | |
|---|---|---|---|
| N (patients) | 90 | 148 | |
| Mean Age (years) | 55 | 53 | NS |
| ASA* | 2.1 | 2.4 | <0.05 |
| Mortality (%) | 1.1 | 2.7 | NS |
| Morbidity (%) | 18 | 21 | NS |
| Intensive Care Unit | 10 | 10 | NS |
| Admissions (%) | |||
| Length of Stay (days) | 11 | 7 | <0.001 |
ASA=American Society of Anesthesia preoperative classification.
Table 4 compares characteristics and outcome data according to the surgical approach used. The P-values for operating room time, intensive care unit admissions, and length of stay refer to the differences between the laparoscopic cholecystectomy (LC) or attempted-LC group and the open cholecystectomy (OC) or converted groups. Significant differences existed between both completed and attempted LC in comparison with the open cholecystectomy. No statistically significant difference existed between the OC and converted groups in any of these categories. Subgroup analysis for patients undergoing cholecystectomy after 1992 revealed that patients undergoing laparoscopic cholecystectomy had a lower mean ASA score than did patients undergoing open cholecystectomy (2.28 vs. 2.73; P<0.01).
Table 4.
Comparison of Patient Demographics and Outcome Data by Operative Method Used
| Attempted LC* | Completed LC* | Converted LC* | OC* | P Value | |
|---|---|---|---|---|---|
| Patients (n) | 97 | 64 | 33 | 141 | |
| Age (years) | 52 | 52 | 52 | 55 | NS |
| ASA* | 2.3 | 2.3 | 2.2 | 2.3 | NS |
| Morbidity Rate (%) | 18.5 | 17 | 21 | 20.5 | NS |
| Mortality Rate (%) | 1 | 1.5 | 0 | 2.8 | NS |
| Operating Room Time (min) | 110 | 106 | 126 | 136 | <0.01 |
| Intensive Care Unit Admissions (%) | 5 | 3 | 9 | 13 | <0.05 |
| Length of Stay (days) | 5.7 | 4.7 | 7.3 | 10 | <0.01 |
LC=laparoscopic cholecystectomy, OC=open cholecystectomy, ASA=American Society of Anesthesia preoperative classification.
Table 5.
Comparison of Demographics and Outcome Data for Patients With Perforated and Nonperforated Gangrenous Gallbladder
| Demographics and Outcome | Patients With Perforated Gallbladder | Patients With Nonperforated Gangrenous Gallbladder | P Value |
|---|---|---|---|
| N | 30 | 208 | |
| Mean Age (years) | 60 | 53 | <0.05 |
| ASA | 2.6 | 2.3 | 0.07 |
| Morbidity (%) | 37 | 17 | <0.05 |
| Mortality (%) | 7 | 1.4 | <0.05 |
| Length of Stay (days) | 13 | 8 | <0.001 |
ASA=American Society of Anesthesia preoperative classification.
DISCUSSION
The use of laparoscopic cholecystectomy in the management of gangrenous cholecystitis has been challenged by some authors. Most studies report conversion rates for patients with gangrenous cholecystitis that are substantially higher than for patients undergoing elective laparoscopic cholecystectomy (Table 6).4–8,10–12 However, Bender et al11 found no change in the conversion rates over a 7-year study period. Similarly, Singer and McKeen5 found no significant difference in the length of hospital stay and a longer operative time in laparoscopically treated patients. Habib et al8 reported worse patient outcomes after conversion.
Table 6.
Gangrenous Cholecystitis
| Study | Year | n | Conversion Rate (%) | Morbidity (%) | Mortality (%) |
|---|---|---|---|---|---|
| Morfin1 | 1968 | 45 | N/A | 31 | 9 |
| Ahmad2 | 1983 | 43 | N/A | 16 | 0 |
| Cox4 | 1993 | 10 | 50 | 12 | 0 |
| Singer5 | 1994 | 24 | 75 | 8.3 | 0 |
| Eldar12 | 1997 | 51 | 49 | 20 | |
| Kiviluoto6 | 1998 | 21 | 16 | 0 | |
| Merriam7 | 1999 | 27 | 35 | 0 | 0 |
| Hunt10 | 2000 | 25 | 8.7 | 12 | 0 |
| Habib8 | 2001 | 53 | 32 | 50 | 0 |
| Bender11 | 2002 | 101 | 40 | 18 | 3 |
| Present Study | 2003 | 238 | 33 | 19 | 2 |
We reviewed our experience with the minimally invasive treatment of gangrenous cholecystitis and compared it with that of the previous decade of open cholecystectomy at the same institution. Morbidity and mortality rates were not significantly different between the 2 decades or in relation to the surgical approach used. Conversion did not appear to add significant morbidity. Despite increased ASA scores, the morbidity rate did not increase in the second decade, which likely reflects improved perioperative care. Grade III complications (including heart attack, heart failure, stroke) were more frequent in patients who had undergone the open procedure (primarily or after conversion). Postoperative intraabdominal infections were more frequent when the laparoscopic approach was used. Bile leaks appeared more frequently with the laparoscopic approach, but this did not reach statistical significance (Table 2). Although no easily identifiable cause exists for the increased incidence of postoperative bile leaks and abscesses in our data, the observation that significantly fewer intraoperative cholangiograms were performed in these patients might indicate the severity of the disease that made cholangiogram unfeasible.
In our study, the operative time and length of hospital stay favor the laparoscopic approach. Until 1997, few patients with gangrenous cholecystitis underwent laparoscopic cholecystectomy. Only after the experience with the laparoscopic procedure at our institution increased was it offered to most patients with severe gallstone disease. This is reflected in the significantly lower mean ASA scores for the laparoscopic group compared with ASA scores in patients undergoing the primary open procedure during the same period. Lacking precise predictors for conversion to the open procedure, we feel that laparoscopic cholecystectomy should be offered to most patients.
CONCLUSION
Gangrenous cholecystitis remains a disease that carries high morbidity and mortality. Men are more commonly affected, and Hispanic patients present at a younger age than Caucasians do but have lower morbidity from the disease. Laparoscopic cholecystectomy can be safely performed in most patients and leads to shorter hospital stays and fewer intensive care unit admissions and possibly less severe morbidity. Laparoscopy should be the initial approach in the treatment of most patients with gangrenous cholecystitis even in the face of higher conversion rates. The increased incidence of intraabdominal abscesses with the minimally invasive approach calls for new methods to decrease this complication.
Footnotes
Presented at the 12th International Congress and Endo Expo 2003, SLS Annual Meeting, Las Vegas, Nevada, USA, September 22–25, 2003.
References:
- 1. Morfin E, Ponka JL, Bush BE. Gangrenous cholecystitis. Arch Surg. 1968;96:567–573 [DOI] [PubMed] [Google Scholar]
- 2. Ahmad MM, Macon WL. Gangrene of the gallbladder. Am Surg. 1983;49:155–158 [PubMed] [Google Scholar]
- 3. Fry DE, Cox RA. Gangrene of the gallbladder. South Med J. 1981;74:666–668 [DOI] [PubMed] [Google Scholar]
- 4. Cox MR, Wilson TG, Luck AJ, et al. Laparoscopic cholecystectomy for acute inflammation of the gallbladder. Ann Surg. 1993;218:630–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Singer JA, McKeen RV. Laparoscopic cholecystectomy for acute or gangrenous cholecystitis. Am Surg. 1994;60:326–328 [PubMed] [Google Scholar]
- 6. Kiviluoto T, Sirén J, Luukkonen P, Kivilaakso E. Randomized trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351:321–325 [DOI] [PubMed] [Google Scholar]
- 7. Merriam LT, Kanaan SA, Dawes LC, et al. Gangrenous cholecystitis: analysis of risk factors and experience with laparoscopic cholecystectomy. Surgery. 1999;126:680–686 [PubMed] [Google Scholar]
- 8. Habib FA, Kolachalam RB, Khilnani R, Preventza O, Mittal VK. Role of laparoscopic cholecystectomy in the management of gangrenous cholecystitis. Am J Surg. 2001;181:71–75 [DOI] [PubMed] [Google Scholar]
- 9. Wilson AK, Koszol RA, Salwen WA, et al. Gangrenous cholecystitis in an urban VA hospital. J Surg Res. 1994;56:402–404 [DOI] [PubMed] [Google Scholar]
- 10. Hunt DRH, Chu FCK. Gangrenous cholecystitis in the laparoscopic era. Aust NZ J Surg. 2000;70:428–430 [DOI] [PubMed] [Google Scholar]
- 11. Bender JS, Duncan MD, Freeswick PD, Harmon JW, Magnuson TH. Increased laparoscopic experience does not lead to improved results with acute cholecystitis. Am J Surg. 2002;184:591–595 [DOI] [PubMed] [Google Scholar]
- 12. Eldar S, Sabo E, Nash E, et al. Laparoscopic cholecystectomy for acute cholecystitis: prospective trial. World J Surg. 1997;21:540–545 [DOI] [PubMed] [Google Scholar]
- 13. Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111(5):518–526 [PubMed] [Google Scholar]