Abstract
Background:
Congenital midgut malrotation is rarely encountered outside the pediatric population. The Ladd's procedure is the standard corrective measure for intestinal malrotation in children and consists of division of peritoneal bands (Ladd's bands) traversing the posterior abdomen, reduction of volvulus, appendectomy, and functional postioning of the intestine with or without fixation. Clinical manifestations of malrotation and results of Ladd's procedure have been described in adults, but laparoscopic treatment remains to be established as adequate treatment.
Methods:
Records were reviewed of 7 patients, ages 17 to 45, all with a history of abdominal discomfort dating from childhood or early adolescence. The diagnosis of malrotation was made by barium small bowel examination in all cases. Symptoms consisted of recurrent bouts of abdominal pain that were most often postprandial, with bloating and, less frequently, constipation. Surgical treatment consisted of laparoscopic exploration via 4 ports. Peritoneal bands were completely divided, and an appendectomy performed in all patients. Three patients required reduction of nonstrangulated chronic midgut volvulus.
Results:
No early complications occurred, and all patients were discharged on postoperative days 1 through 3. At 2 months to 48 months after surgery, 1 patient had been lost to follow-up. Five patients (71%) reported substantial improvement in abdominal discomfort, with only occasional mild symptoms. Constipation continued in 1 patient, but required less aggressive treatment. One patient reported only slight improvement in postprandial abdominal pain.
Conclusions:
Although rarely encountered, intestinal malrotation after childhood can produce significant clinical symptoms that respond to surgical treatment. The results of the present series indicate that laparoscopic Ladd's procedure is an acceptable alternative to the open technique in treating symptoms of intestinal malrotation in adults.
Keywords: Intestinal malrotation, Ladd's procedure, Laparoscopy
INTRODUCTION
Congenital abnormalities of intestinal rotation are the cause of major clinical problems in infants, ranging from bowel obstruction to catastrophic loss of small intestine due to strangulated midgut volvulus. Over the past 30 years, a growing recognition of intestinal malrotation in adults has occurred, but the significance of this condition when identified after childhood is uncertain. Adult patients recognized as having abnormalities of intestinal rotation associated with symptoms undergo the same operative treatment performed in infants and children with this condition. Reports of the use of the Ladd's procedure in adults suggest that its benefits are similar to those achieved in pediatric surgical practice. However, experience is not extensive, and it is not clear that the clinical presentation in adults exactly parallels that observed in infants and children. The technical feasibility of laparoscopic Ladd's procedures, and limited early results of such treatment have been reported.1–3 In the present series, experience with laparoscopic treatment of a consecutive group of adult patients referred for chronic abdominal complaints after the radiologic diagnosis of intestinal malrotation is presented.
METHODS
Patients
Between June 1997 and February 2003, 7 patients were treated by the authors for intestinal malrotation at Yale New Haven Hospital, New Haven, Connecticut (NES, DKA) and Baystate Medical Center, Springfield, Massachusetts (NES) (Table 1). Patients included 5 women and 2 men, and ages ranged from 17 years to 45 years (mean, 31). One patient had chronic Hepatitis C, but other patients were in generally good health. One had undergone prior pelvic laparoscopy, and a second had undergone prior laparoscopic cholecystectomy. The diagnosis of intestinal malrotation had been made in all patients by barium upper gastrointestinal/small bowel contrast studies that had been ordered for the workup of abdominal pain. Additional tests consisted of abdominal ultrasound, abdominal computed tomographic scan, esophagogastroduodenoscopy, and radionuclide gastric emptying study. Abdominal pain was predominantly early postprandial (onset 30 to 60 minutes after eating) in nature, although 1 patient had a more constant pattern of pain exacerbated by eating. Other symptoms included bloating (4 patients), nausea (3 patients), and constipation (1 patient). Vomiting was not a prominent complaint. In 6 of the patients, symptoms had been present since childhood or adolescence and either ignored or treated with over-the-counter remedies. No presentation was related to new acute symptoms. Demographic data were recorded prospectively, and records were reviewed for length of hospital stay and information regarding symptoms. Patients not seen in office evaluation in the prior 6 months were contacted by telephone for specific information regarding the course of symptoms. Patients were specifically queried for presence, severity, and distribution of pain, as well as information on bowel function, nausea, vomiting, and additional surgical procedures after laparoscopic Ladd's procedure.
Table 1.
Radiologic Findings of Barium Upper Gastrointestinal/Small Bowel Contrast Studies
| Duodenum completely right-sided structure (does not cross midline) |
| Small intestine sequestered in right-side of abdomen |
| Colon to left of small intestine |
| Cecum midline or left-sided in 71% |
Operative Procedures
All patients underwent a Ladd's procedure, which consisted of complete division of all right-sided peritoneal bands, reduction of any noted volvulus, and appendectomy. A 4-port technique was used, with ports placed in the midline or left side of the abdomen. Peritoneal bands were divided with low-current electrocautery or ultrasonic dissecting shears (Harmonic Scalpel, Ethicon Endosurgery, or Autosonix, United States Surgical Corporation). Appendectomy was performed using a stapled technique. Sutured cecal fixation in the right abdomen was performed on the first case but in no others.
RESULTS
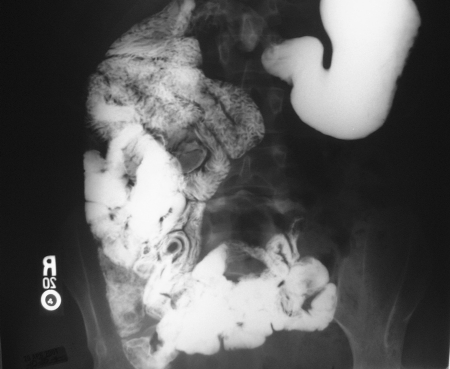
A fairly consistent pattern of radiologic findings was observed on barium upper gastrointestinal, small bowel series studies (Table 2). No radiologic evidence was found of obstruction in any study (Figure 1).
Table 2.
Characteristics and Symptoms of Patients Undergoing Laparoscopic Treatment of Intestinal Malrotation Diagnosed in Adulthood
| Patient # | Age/sex* | Prior Surgery* | Preop Symptoms* | Postop Symptoms |
|---|---|---|---|---|
| 1 | 38/m | none | postprand pain, constipation | constipation |
| 2 | 45/f | pelvic laparoscopy | postprand+constant pain | significant pain |
| 3 | 27/m | none | postprand pain | occasional pain |
| 4 | 40/f | lap cholecystectomy | postprand pain, bloating | none |
| 5 | 20/f | none | postprand pain | lost to follow-up |
| 6 | 29/f | none | postprand pain | none |
| 7 | 17/f | none | postprand pain, bloating | occasional pain |
m=male, f=female, lap=laparoscopic, postprand=postprandial.
Figure 1.
Barium small bowel examination in adult patient with intestinal malrotation.
Operative Findings
The absence of the ligament of Treitz was confirmed in all cases. The presence of a right-sided cecum on contrast study tended to be associated with a nonstrangulated, nonobstructing twist or volvulus of a portion of the small bowel mesentery (3 patients). Lysis of bands resulted in free progression of the small intestine from the pylorus to the ileocecal valve without intervening peritoneal structures or mesenteric twisting.
Postoperative Results
No early postoperative complications occurred, and patients were discharged home after 1 to 3 postoperative days (mean, 1.7 days). Patients were followed up for 2 months to 48 months. One patient was lost to follow-up after 2 months. Five of 7 patients (71%) had significant improvement in all preoperative symptoms, although only 2 patients (29%) reported being completely free of preoperative pain. Of nonpain complaints, constipation in 1 patient, which had been previously attributed to irritable bowel syndrome, persisted but was generally more manageable. One female patient with a more generalized and constant pattern of pain reported only slight relief in abdominal pain postoperatively. No further operative procedures were performed in any patient after laparoscopic Ladd's procedure during the period of follow-up.
DISCUSSION
The embryologic events leading to disorders of intestinal rotation were well-characterized as early as 1923 by Dott,4 and their patterns of occurrence in infants well-described by Kiesewetter in 1958.5 The occurrence of symptomatic intestinal malrotation beyond childhood has been reported intermittently over the last 4 decades, but it is quite clear that this is an uncommon clinical problem. Estimating the incidence of malrotation in adults in hampered by the fact that it may present to a variable degree and may be completely asymptomatic. The best estimate of prevalence is approximately 0.2% based on barium enemas done in 2000 asymptomatic patients.6 However, malrotation is rarely diagnosed in the absence of symptoms, and incomplete rotation may be so subtle a finding as to go unnoticed even at the time of abdominal exploration for other indications. Symptoms may be chronic or acute in nature, and generally prompt a workup that includes a barium contrast study of the foregut and midgut that demonstrates the anatomic abnormality.7 Surgical treatment has been guided by the pediatric surgical experience, and the Ladd's procedure has also been the treatment of choice in adults with malrotation.8,9
The results of the present report confirm both the technical feasibility and effectiveness of the laparoscopic approach to intestinal malrotation in adults. Based on the presented experience, it remains difficult to comment specifically on the value of Ladd's procedure in the adult population beyond the reduction of pain symptoms, because the risk of occurrence of clinically significant acute midgut volvulus without surgery is unknown. In 3 of the cases presented, twisting of the mesenteric pedicle was noted and easily reversed after peritoneal band lysis. However, this finding was not radiologically evident preoperatively and may have represented a long-standing anatomic situation with an uncertain association with chronic symptoms. Reports exist in the medical literature of emergent presentation of midgut volvulus in adults, although these are small in number.8,10–13 The most compelling of these described 7 patients with acute obstruction.10 These patients were treated promptly, and it was presumed that strangulation was avoided. It is not clear from these reports to what extent that adults are at risk for acute strangulating volvulus as compared with experience in infants. Strangulated midgut volvulus in infancy and early childhood can be so catastrophic and potentially life threatening an event that, extrapolating this experience, it would seem prudent to treat even asymptomatic intestinal malrotation in adults. The actual health risk of asymptomatic malrotation remains unknown.
The pain reported by our patients did not correlate with obstructive foregut or midgut pathology by contrast study. This raises questions as to the pathophysiology of pain associated with the architecture encountered. Peritoneal bands may have a restrictive effect on normal duodenal motility, but beyond this no clear explanation exists for the intensity of symptoms seen. As yet undescribed but potentially complex neurohumoral or neuromuscular changes may occur as the result of peritoneal band division in the area of previously entrapped duodenum or proximal jejunum. The relief of early postprandial symptoms observed in the majority of patients in the present series strongly suggests that freeing the duodenum may be of benefit in addressing patients' most pressing complaints.
The Ladd's procedure may be performed safely, with a high degree of patient satisfaction, by a laparoscopic approach in adults. Long-term follow-up will be required to determine whether patients are at risk for either new symptoms or recurrent malrotation-related problems such as midgut volvulus.
References:
- 1. Gross E, Chen MK, Lobe TE. Laparoscopic evaluation and treatment of intestinal malrotation in infants. Surg Endosc. 1996; 10:936–937 [DOI] [PubMed] [Google Scholar]
- 2. Bax NM, van der Zee DC. Laparoscopic treatment of intestinal malrotation in children. Surg Endosc. 1998;12:1314–1316 [DOI] [PubMed] [Google Scholar]
- 3. Yamashita H, Kato H, Uyama S, et al. Laparoscopic repair of intestinal malrotation complicated by midgut volvulus. Surg Endosc. 1999;13:1160–1162 [DOI] [PubMed] [Google Scholar]
- 4. Kiesewetter WB, Smith JW. Malrotation of midgut in infancy and childhood. Arch Surg. 1958;77:483–491 [DOI] [PubMed] [Google Scholar]
- 5. Dott NM. Anomalies of intestinal rotation: their embryology and surgical aspects with reports of five cases. Br J Surg. 1923; 251–286 [Google Scholar]
- 6. Kantor JL. Anomalies of the colon. Radiology. 1934;23:651–662 [Google Scholar]
- 7. Balthasar EJ. Intestinal malrotation in adults. Am J Roentgenol. 1976;126:358–362 [DOI] [PubMed] [Google Scholar]
- 8. Von Fl, ue M, Herzog U, Ackermann C, Tondelli P, Harder F. Acute and chronic presentation of intestinal nonrotation in adults. Dis Colon Rectum. 1994;37:192–198 [DOI] [PubMed] [Google Scholar]
- 9. Kern IB, Currie BG. The presentation of malrotation of the intestines in adults. Ann R Coll Surg Engl. 1990;72:239–242 [PMC free article] [PubMed] [Google Scholar]
- 10. Devlin HB, Williams RS, Pierce JW. Presentation of midgut malrotation in adults. BMJ. 1986;1:803–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rowsom JT, Sullivan SN, Girvan DP. Midgut volvulus in the adult, a complication of intestinal malrotation. J Clin Gastroenterol. 1987;9:212–216 [DOI] [PubMed] [Google Scholar]
- 12. Garg RC, Sharma J, Kumar N, et al. Symptomatic volvulus due to midgut malrotation in an adult. Trop Gastroenterol. 2001; 22:93–94 [PubMed] [Google Scholar]
- 13. Fukuya T, Brown BP, Lu CC. Midgut volvulus as a complication of intestinal malrotation in adults. Dig Dis Sci. 1993;38:438–444 [DOI] [PubMed] [Google Scholar]