Abstract
Objective:
Pediatric gastric access for long-term enteral feeding may be performed via a laparotomy, laparoscopy, or a percutaneous approach. In children and adolescents, laparoscopic-assisted gastrostomy may be difficult due to a thick abdominal wall. Therefore, if the abdominal wall is estimated to be >2 cm on physical examination, or in children in whom a percutaneous endoscopic gastrostomy was unsuccessfully attempted by a gastroenterologist, we routinely perform a laparoscopic-assisted percutaneous endoscopic gastrostomy.
Methods:
From January 1998 through February 2003, we retrospectively reviewed 15 cases of a laparoscopic-assisted percutaneous endoscopic gastrostomy. Instruments used to perform this technique are a percutaneous endoscopic gastrostomy kit, an Olympus flexible endoscope, and one 5-mm STEP port placed through an infraumbilical incision for a 5-mm, 30-degree scope.
Results:
Age range was 2 years to 20 years (mean, 10). Operative time ranged from 20 minutes to 45 minutes. When a concurrent laparoscopic Nissen fundoplication was performed (n = 6), the percutaneous endoscopic gastrostomy was placed after completion of the Nissen fundoplication. No intraoperative complications occurred, and all tubes were successfully placed. Feeds were instituted the following day and advanced to goal. To date, no postoperative complications have occurred, and revision has not been necessary.
Conclusions:
Laparoscopic-assisted percutaneous endoscopic gastrostomy in children and adolescents is safe and effective. Utilizing laparoscopy permits evaluation of the peritoneum and lysis of adhesions, if necessary. Moreover, laparoscopy provides excellent exposure for accurate placement of the PEG, while avoiding injury to other organs.
Keywords: Laparoscopy, Percutaneous endoscopic gastrostomy
INTRODUCTION
Pediatric gastric access for long-term enteral feeding may be performed via laparotomy, laparoscopy, or a percutaneous approach. Gauderer et al1 initially described the percutaneous endoscopic gastrostomy (PEG) in 1980. It has since become widely accepted in both the adult and pediatric populations with over 216,000 performed annually in the United States.1 However, this technique is not without complications, with major complication rates reported as high as 17.5%.2
One of the more specific complications to the percutaneous technique is the formation of a gastroenteric or a gastrocolocutaneous fistula with a reported rate of 2% to 3.5%.3,4 These usually result from an inadvertent enterotomy made during the blind placement of the introducer needle for gastric access. Patients with prior abdominal surgery are often precluded from a PEG because of such concerns. Additionally, the location within the stomach of the PEG may cause gastroesophageal reflux.5
In children in whom a PEG was unsuccessfully attempted by a gastroenterologist, we routinely perform a laparoscopic-assisted PEG. In 1995, Stringel et al6 reported this approach in 2 children where attempts at simple PEG had failed. In addition, we routinely perform a laparoscopic-assisted PEG in children not referred to a gastroenterolo-gist who require enteral access and have an abdominal wall >2 cm in size on physical examination. If the abdominal wall is >2cm, then it becomes technically difficult to perform a laparoscopic gastrostomy through the 5-mm port, and therefore we have adopted the laparoscopic-assisted PEG in these situations. If the abdominal wall is <2 cm, we routinely perform a laparoscopic gastrostomy with an MIC-KEY button (Ballard Medical Products, Draper, Utah) on the greater curvature of the stomach. In 1993, Stringel et al7 reported on a laparoscopic gastrostomy positioned on the lesser curvature of the stomach to help prevent reflux. We report our initial 15 cases utilizing laparoscopic-assisted PEG.
METHODS
From January 1998 to February 2003, we retrospectively reviewed all cases of laparoscopic-assisted PEG. The placement of the PEG utilizes a standard PEG kit, flexible Olympus endoscope; 5-mm, 30-degree laparoscope; and a 5-mm STEP (Tyco Healthcare, Norwalk, Connecticut) port. The 5-mm port is placed through an infraumbilical incision using an open technique. Once pneumoperitoneum is achieved, the 5-mm, 30-degree laparoscope is then introduced for diagnostic evaluation of the peritoneum. Once the stomach is identified and amenable for safe advancement to the anterior abdominal wall, the assistant advances the endoscope into the stomach. The stomach is insufflated, and by using laparoscopy, an optimal placement of the PEG on the greater curvature of the stomach is achieved. The needle and sheath are inserted through the anterior abdominal wall in the left upper quadrant by the surgeon and into the greater curvature of the stomach under direct visualization. The PEG is then performed in the standard fashion. Once the PEG is in satisfactory position, we confirm gastric apposition to the abdominal wall by using the laparoscope and document the distance of the PEG tube in relation to the skin edge for postoperative management.
This study was reviewed and approved by the Colorado Multiple Institutional Review Board (COMIRB#04 – 0729).
RESULTS
During the study period, 15 children underwent laparoscopic-assisted PEG. The age range was 2 years to 20 years with a mean age of 10 years. Operative times for PEG placement ranged from 20 minutes to 45 minutes. In 6 of these patients, the PEG was placed at the completion of a laparoscopic Nissen fundoplication. No intraoperative complications occurred, and all PEG tubes were successfully placed by using this technique. Feeds were instituted the following day and advanced to goal. To date, no postoperative complications have occurred, and revision has not been necessary.
DISCUSSION
Percutaneous endoscopic gastrostomy has become a routine procedure for feeding access in both the adult and pediatric population. For children who have had a failed attempt at PEG, we have been able to safely and effectively perform a laparoscopic-assisted PEG as described by Stringel et al in 1995.6 No intraoperative or postoperative complications have occurred to date, and no conversion to an open gastrostomy has been necessary.
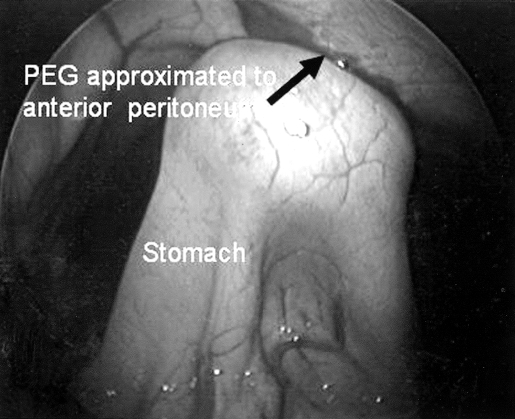
A majority of the laparoscopic-assisted PEGs were performed as the primary procedure. Placement of the laparoscope through a small infraumbilical incision is easily performed without much additional operative time. By performing the percutaneous gastric access under direct vision, we can guide the placement of the PEG tube to an ideal location on the stomach and prevent injury to the bowel (Figure 1). The location of the PEG is often a result of where the endoscope best transilluminates through the abdominal wall, which is not always an ideal location.
Figure 1.
Placement of the PEG within the body of the stomach with good apposition to the anterior abdominal wall.
Razeghi et al5 found that PEG placement in the antrum led to increased reflux in children. Using the laparoscope permits accuracy in the placement of the PEG. In one patient with a prior surgery, the placement of the laparoscope allowed for identification and subsequent lysis of adhesions, which then permitted safe completion of the PEG.
If the abdominal wall is <2 cm, we routinely perform a laparoscopic gastrostomy with an MIC-KEY button. Although Stringel et al7 reported this approach in 1993, they placed the gastrostomy on the lesser curvature of the stomach to help prevent reflux. We routinely position the gastrostomy on the greater curvature in the body of the stomach.
If the abdominal wall is >2 cm, then it becomes technically difficult to perform a laparoscopic gastrostomy, and therefore we have adopted the laparoscopic-assisted PEG in these situations. It is difficult to perform an MIC-KEY button gastrostomy through a 5-mm port, and therefore we will perform a laparoscopic PEG instead. This obviates the need to enlarge a port site or make a separate incision, maintaining the minimally invasive nature of the procedure. Furthermore, we have successfully performed this technique at the completion of other laparoscopic procedures, such as a Nissen fundoplication.
CONCLUSION
Based on our initial experience, laparoscopic-assisted PEG is a safe and effective technique to allow for feeding access as an alternative to an open gastrostomy, when a simple PEG has been unsuccessful or in children where a laparoscopic gastrostomy is difficult due to a thick abdominal wall. In these 2 situations, the addition of laparoscopy to the PEG placement is a safe, effective, and cosmetically superior approach over a standard gastrostomy incision.
Footnotes
Presented at the 12th International Congress and Endo Expo 2003, SLS Annual Meeting, Las Vegas, Nevada, USA, September 22–25, 2003.
References:
- 1. Gauderer MW, Ponsky JL, Izant RJ., Jr Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872–875 [DOI] [PubMed] [Google Scholar]
- 2. Gauderer MW. Percutaneous endoscopic gastrostomy-20 years later: a historical perspective. J Pediatr Surg. 2001;36:217–219 [DOI] [PubMed] [Google Scholar]
- 3. Khatak IU, Kimber C, Kiely EM, et al. Percutaneous endoscopic gastrostomy in paediatric practice: Complications and outcome. J Pediatr Surg. 1998;33:67–72 [DOI] [PubMed] [Google Scholar]
- 4. Patwardhan N, McHugh K, Drake D, Spitz L. Gastroenteric fistula complicating percutaneous endoscopic gastrostomy. J Pediatr Surg. 2004;39:561–564 [DOI] [PubMed] [Google Scholar]
- 5. Razeghi S, Lang T, Behrens R. Influence of percutaneous endoscopic gastrostomy on gastroesophageal reflux: a prospective study on 68 children. J Pediatr Gastroenterol Nutr. 2002;35:27–33 [DOI] [PubMed] [Google Scholar]
- 6. Stringel G, Geller ER, Lowenheim MS. Laparoscopic-assisted percutaneous endoscopic gastrostomy. J Pediatr Surg. 1995; 30(8):1209–1210 [DOI] [PubMed] [Google Scholar]
- 7. Stringel G, Robinson E, Maisel S. Laparoscopic gastrostomy. Pediatr Surg Int. 1993;382–384 [Google Scholar]