Abstract
Objectives:
Laparoscopic splenectomy has been increasingly used in patients with idiopathic thrombocytopenic purpura. Because it is associated with minimal abdominal trauma, platelet consumption could be reduced with the laparoscopic approach. The aim of this study was to analyze intraoperative bleeding and the need for apheresis platelets, comparing laparoscopic with open splenectomy.
Methods:
Records of 40 patients who underwent splenectomy (20 through laparoscopy and 20 through open surgery) for idiopathic thrombocytopenic purpura were retrospectively reviewed. Intraoperative bleeding and need of perioperative apheresis platelets were evaluated in both groups. Statistical evaluation was conducted using the Mann-Whitney rank test, and differences were considered significant at P<0.01.
Results:
The mean amount of intraoperative bleeding was less in the laparoscopic group (P<0.01). Apheresis platelets were necessary in all patients in the open group (2 units transfused in 55% and 1 unit in 45% of cases) and only in 30% of cases in the laparoscopic group (1 unit transfused in each case).
Conclusions:
Laparoscopic splenectomy is a safe procedure also in patients at high risk for bleeding diathesis. In idiopathic thrombocytopenic purpura, laparoscopic splenectomy should be the gold-standard surgical treatment. Need of platelet transfusion is probably reduced when laparoscopic splenectomy is compared with open surgery in these patients.
Keywords: Laparoscopic splenectomy, Idiopathic thrombocytopenic purpura, Apheresis platelets, Platelet transfusion
INTRODUCTION
Laparoscopic splenectomy has been increasingly used for removal of the spleen in patients with idiopathic thrombocytopenic purpura (ITP) refractory to medical treatment.1 Since its introduction in 1992,2 several studies have been published pointing out the safety of the procedure and the advantages, such as shorter hospital stay, less postoperative pain, and fewer complications.3,4 Other studies have compared the therapeutic response of laparoscopic versus open splenectomy, with contradictory results.5–7
Because laparoscopic splenectomy is associated with less abdominal trauma, operative platelet consumption and therefore need of platelet transfusion may be reduced during laparoscopy compared with open surgery. However, no data exist in this regard at this time. In this study, we evaluated in a retrospective analysis differences in intraoperative bleeding and the need for platelet transfusion comparing laparoscopic and open splenectomy.
METHODS
The records of 40 patients, who underwent splenectomy for ITP from 1994 to 2002, were reviewed. In 20 patients (study group), the spleen was removed laparoscopically, whereas in the other 20 patients (historical control group) splenectomy was performed by open surgery. In both groups, the same surgeon (RV) performed splenectomy, and enrollment in the laparoscopic or open group was determined according to the patient's choice.
Data assessed for each group are reported in Table 1. The median age of the patients was similar in both groups. The male-to-female ratio was also comparable. Preoperative median platelet counts were not statistically different. Alternative causes of thrombocytopenia were accurately ruled out before any medical or surgical treatment in these patients. All patients were previously treated with corticosteroids (prednisone 1 mg/Kg/die) for 4 months to 6 months before surgery. Splenectomy was indicated in cases refractory to medical treatment or relapsing at the interruption of corticosteroid therapy. All patients were symptomatic with various degrees of mucocutaneous bleeding when surgery was proposed. In these series, preoperative infusion of intravenous IgV was not performed in any patient.
Table 1.
Patient Data: Open Versus Laparoscopic Splenectomy
| Open | Laparoscopic | |
|---|---|---|
| Age (range) (yrs) | 19 to 30 | 18 to 27 |
| Sex ratio (M/F) | 1:3 | 1:3 |
| Mean preoperative platelet count (range) | 15 × 109/L (3 to 30) | 18 × 109/L (3 to 27) |
| Mean months of preoperative corticosteroid therapy (range) | 6 (2 to 8) | 4 (2 to 7) |
Open splenectomy was performed in the traditional fashion.1 Through a midline abdominal incision, short gastric vessels were accurately identified and divided. Splenic artery and vein were ligated and divided. Splenic hilum, tail of the pancreas, splenocolic and gastrosplenic ligaments, omentum, and paraduodenal area were always checked for accessory spleens, which were found in 2 patients (10%) in this series. Laparoscopic splenectomies were performed with patients lying in the right lateral position (left flank elevated about 45° above the operating table). A Hasson trocar was inserted in the upper umbilical region, and 3 other trocars were placed in the subxyphoid area (10 mm), lower left midclavicular line below the umbilical line (10 mm), and lower left axillary line (5 mm). With a 30° scope, after dissection of the spleno-colic ligament, division of the gastrosplenic ligament with the short gastric vessels was accomplished by using the ultrasonic dissector (Ultracision Harmonic Scalpel, Ethicon Endosurgery, Inc., Cincinnati, OH, USA). The convex surface of the spleen was then accurately dissected from the lateral abdominal wall and from the diaphragm; at this point, the splenic hilum was approached from the anterior aspect, and the splenic artery and veins were clipped and divided. The spleen was then inserted in a plastic bag that was pulled through the abdominal umbilical access. The spleen was then crushed and removed, care being taken to prevent bag lacerations and splenic fragment peritoneal implantation (splenosis). Like in the open approach, sites of accessory spleen were accurately scoped, and this allowed their identification and removal in 3 patients (15%) in this study group.
Results were evaluated comparing intraoperative bleeding and the need for perioperative platelet transfusion in the 2 groups. Platelets were transfused with apheresis platelets and were administered to the patients when the surgeon noted intraoperative bleeding from the cut surface without any evidence of damaged vessel. Statistical evaluation was conducted using the Wilcoxon rank sum test. Differences were considered statistically significant at P<0.01.
RESULTS
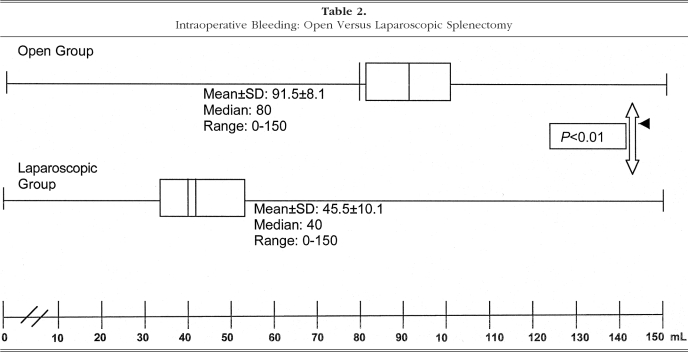
No intraoperative or postoperative complications occurred in either group. Data for each parameter evaluated in this study are reported in Tables 2 and 3. The mean amount of operative bleeding was 45.5±10.1 (median, 40; range, 0 to 150) in the laparoscopic group compared with 91.5±8.1 (median, 80; range, 0 to 150) in the open splenectomy group (P<0.01). Considering the number of patients who received platelet transfusion, in the open group 100% of the patients had apheresis platelets transfused, compared with only 30% in the laparoscopic group. In the open group, 55% of patients needed 1 unit and 45% 2 units. All patients who needed platelet transfusion in the laparoscopic group received only 1 unit of apheresis platelets. No postoperative bleeding was observed in any patient in either group.
Table 2.
Intraoperative Bleeding: Open Versus Laparoscopic Splenectomy
Table 3.
Platelet Transfusion: Open Versus Laparoscopic Splenectomy
| Open Group | Laparoscopic Group | |
|---|---|---|
| Percent of patients transfused | 100 | 30 |
| Units transfused (% pts) | 1 U (55) | 1 U (30) |
| 2 U (45) |
DISCUSSION
Steroid therapy and splenectomy are the most effective treatment options in patients with ITP. Steroid therapy is curative in about 50% of these patients,8 but definitive remission of the disease has been described in only 20% to 25% of the treated cases.1,9,10 Splenectomy is indicated in patients who do not respond to medical therapy, in patients relapsing at the withdrawal of steroid therapy, when steroid therapy is contraindicated, or in cases with low compliance to prolonged medical treatment.
Since its introduction in 1992,2 laparoscopic splenectomy has been gaining increasing attention in several centers for removal of the spleen, especially for benign hemato-logical disorders. ITP is the most common indication for laparoscopic splenectomy in several series reported in the literature,11–18 probably because of the less challenging operative technique due to the absence of splenomegaly in these patients. Laparoscopic splenectomy can be performed safely in ITP patients, despite thrombocytopenia, and is associated with decreased hospital stay, shorter time to recovery, and lower hospital charges compared with those in open approach.19,20
The laparoscopic approach also allows complete visualization of sites where accessory spleens are located, whose removal is essential for the curative effects of splenectomy in patients with ITP. With laparoscopic techniques, the splenic hilum, tail of the pancreas, splenocolic and gastrosplenic ligaments, omentum, and paraduodenal area can be easily checked for accessory spleens, which are present in 18% to 95% of ITP patients.12–14 Because it lacks tactile feedback, to improve the success of laparoscopy in detecting small accessory spleens, in recent reports some authors have recommended using an intraoperative gamma probe.21
In addition, laparoscopy could be responsible for hematological benefits. Only a few studies, however, have addressed this issue. In spite of a few contradictory reports, most clinical and experimental22 studies support the view that laparoscopic surgery is associated with better preservation of postoperative systemic immune function than is open surgery. Several other clinical studies have shown that laparoscopic surgery may induce fewer thrombogenic changes than traditional surgery does, although deep vein thrombosis can still occur after laparoscopy, and its prevention is mandatory in mini-invasive procedures.23 No study has been published with regard to platelet consumption in laparoscopic surgery. The lesser extent of tissue trauma with laparoscopy, which seems to be the key factor for the immunological and coagulative differences compared with those of open surgery, could induce a lower consumption of platelets. With laparoscopy, it can be supposed that use of platelets for hemostasis of small vessels in the cut surface, especially in the abdominal wall, is less pronounced and therefore their consumption is reduced. Our study seems to confirm this hypothesis. In our study, in patients whose spleen had been removed laparoscopically, surface bleeding during the dissection of the spleen from its attachments appeared less important than in open surgery and almost never required intraoperative transfusion of platelets. In our opinion, this could be explained by the fact that circulating platelets were preserved in the abdominal phase of the operation and used by the organism when they occurred for hemostasis in dissection of the spleen, resulting in less bleeding during the intraabdominal phase of the procedure. The use of the Harmonic scalpel might also play an additional role in the reduced intraoperative bleeding during laparoscopy. In the laparoscopic group of this study, intraoperative bleeding was less significant, with P<0.01, than in the open surgery group and the need for apheresis platelets was lower, as judged by the surgeons during the operation.
CONCLUSION
Laparoscopic splenectomy is a safe procedure in patients with a high risk of bleeding diathesis. In ITP patients, the laparoscopic approach for removal of the spleen should be the gold-standard surgical treatment. Need for platelet transfusion is probably reduced when laparoscopic splenectomy is compared with open surgery in these patients.
Contributor Information
Rosario Vecchio, University of Catania, Department of Surgery Vittorio Emanuele Hospital, Catania, Italy..
Emma Cacciola, Department of Biomedical Science, Section of Haematology, Vittorio Emanuele Hospital Catania, Italy..
Giuseppe Lipari, University of Catania, Department of Surgery Vittorio Emanuele Hospital, Catania, Italy..
Valeria Privitera, University of Catania, Department of Surgery Vittorio Emanuele Hospital, Catania, Italy..
Chiara Polino, University of Catania, Department of Surgery Vittorio Emanuele Hospital, Catania, Italy..
Rossella Cacciola, Department of Biomedical Science, Section of Haematology, Vittorio Emanuele Hospital Catania, Italy..
References:
- 1. Vecchio R, Cacciola E, Cacciola RR, Palazzo F, Rinzivillo C, Giustolisi R. Predictive factors of response to splenectomy in adult chronic idiopathic thrombocytopenic purpura. Int Surg. 2000;85(3):252–256 [PubMed] [Google Scholar]
- 2. Delaitre B, Maignien B, Icard P. Laparoscopic splenectomy. Br J Surg. 1992;79:1334. [DOI] [PubMed] [Google Scholar]
- 3. Katkhouda N, Waldrep DJ, Feinstein D, et al. Unresolved issues in laparoscopic splenectomy. Am J Surg. 1996;172:585–590 [DOI] [PubMed] [Google Scholar]
- 4. Lefor AT, Melvin S, Bailey RW, Flowers JL. Laparoscopic splenectomy in the management of immune thrombocytopenic purpura. Surgery. 1993;114:613–618 [PubMed] [Google Scholar]
- 5. Lozano-Salazar RR, Herrera MF, Vargas-Vorackova F, Lopez-Kar X. Laparoscopic versus open splenectomy for immune thrombocytopenic purpura. Am J Surg. 1998;176(4):366–369 [DOI] [PubMed] [Google Scholar]
- 6. Brunt LM, Langer JC, Quasebarth MA, Whitman DE. Comparative analysis of laparoscopic versus open splenectomy. Am J Surg. 1996;172:596–601 [DOI] [PubMed] [Google Scholar]
- 7. Watson DI, Coventry BJ, Chin T, et al. Laparoscopic versus open splenectomy for immune thrombocytopenic purpura. Surgery. 1997;121:18–22 [DOI] [PubMed] [Google Scholar]
- 8. Coon WN. Splenectomy for ITP. Surg Gynecol Obstet. 1987; 164(3):225–229 [PubMed] [Google Scholar]
- 9. Di Fi, no SM, Lachant NA, Kirshner JJ, Gottlieb AJ. Adult idiopathic thrombocytopenic purpura. Am J Med. 1980;69:430–442 [DOI] [PubMed] [Google Scholar]
- 10. Mc Millan R. Chronic ITP. N Eng J Med. 304(19):1135–1147, 1981 [Google Scholar]
- 11. Baccarani U, Terrosu G, Donini A, Zaja F, Bresadola F, Baccarini M. Splenectomy in hematology. Current practice and new perspectives. Haematologica. 1999;84:431–436 [PubMed] [Google Scholar]
- 12. Terrosu G, Donini A, Baccarani U, et al. Laparoscopic versus open splenectomy in the management of splenomegaly: our preliminary experience. Surgery. 1998;125:154. [PubMed] [Google Scholar]
- 13. Glasgow RE, Yee LF, Mulvihill SJ. Laparoscopic splenectomy. The emerging standard. Surg Endosc. 1997;11(2):108–112 [DOI] [PubMed] [Google Scholar]
- 14. Decker G, Millat B, Guillon F, Atger J, Linon M. Laparoscopic splenectomy for benign and malignant hematologic disease: 35 consecutive cases. World J Surg. 1998;22(1):62–68 [DOI] [PubMed] [Google Scholar]
- 15. Trias M, Taragona EM, Espert JJ, et al. Impact of hematological diagnosis on early and late outcome after laparoscopic splenectomy: an analysis of 111 cases. Surg Endosc. 2000;14(6): 556–560 [DOI] [PubMed] [Google Scholar]
- 16. Breslel R, Guerci A, Brunaud L, et al. Laparoscopic splenectomy for idiopathic thrombocytopenic purpura: outcome and long-term results. World J Surg. 2002;26:111–114 [DOI] [PubMed] [Google Scholar]
- 17. Friedman RL, Hiatt JR, Korman JL, Facklis K, Cymerman J, Phillips EH. Laparoscopic or open splenectomy for hematologic disease: which approach is superior? J Am Coll Surg. 1997;185:49–54 [PubMed] [Google Scholar]
- 18. Gigot JF, Lengele B, Gianello P, Etienne J, Claeys N. Present status of laparoscopic splenectomy for hematologic diseases: certitudes and unresolved issues. Sem Lap Surg. 1998;3:147–167 [DOI] [PubMed] [Google Scholar]
- 19. Harold KL, Schlinkert RT, Mann DK, et al. Long-term results of laparoscopic splenectomy for immune thrombocytopenic purpura. Mayo Clin Proc. 1999;74:37–39 [DOI] [PubMed] [Google Scholar]
- 20. Schlinkert RT, Mann D, Weaver A. Laparoscopic splenectomy: reduction of hospital charges. J Gastrointest Surg. 1998;2:278–282 [DOI] [PubMed] [Google Scholar]
- 21. Antevil J, Thoman D, Taller J, Biondi M. Laparoscopic accessory splenectomy with intraoperative gamma probe localization for recurrent idiopathic thrombocytopenic purpura. Surg Laparosc Endosc Percutan Techn. 2002;5:371–374 [DOI] [PubMed] [Google Scholar]
- 22. Gupta A, Watson DI. Effect of laparoscopy on immune function. Br J Surg. 2001;88:1296–1306 [DOI] [PubMed] [Google Scholar]
- 23. Vecchio R, Cacciola E, Di Martino M, Cacciola RR, MacFadyen BV. Modifications of coagulation and fibrinolytic parameters in laparoscopic cholecystectomy. Surg Endosc. 2003;17:428–433 [DOI] [PubMed] [Google Scholar]