Abstract
Objectives:
For years, limiting operative wound sepsis and its resultant morbidity in patients with small bowel perforations has been a major headache for surgeons. The present study was intended to extend the benefits of minimally invasive surgery to traumatic and typhoid small bowel perforations, in terms of assessing its feasibility and limiting wound sepsis.
Methods:
Twenty-five patients (20 with typhoid ileal and 5 with traumatic small bowel perforation) presenting within 96 hours of the catastrophe were included in the study. All were explored laparoscopically, and the perforation repaired by intracorporeal suturing.
Results:
Time of operation varied from 45 minutes to 92 minutes. Two patients developed port-site infection. None of the patients developed postoperative fistula, and no mortalities occurred. Postoperative hospital stay was between 7 days and 10 days.
Conclusion:
Benefits of minimally invasive surgery can be safely and efficaciously extended to select patients with small bowel perforation in terms of limiting sepsis-related wound complications.
Keywords: Typhoid ileal perforation, Traumatic small bowel perforation, Laparoscopic repair
INTRODUCTION
Laparoscopic surgery has gained clinical acceptance in recent years for the treatment of patients with a variety of gastrointestinal diseases. It is agreed that patients who undergo laparoscopic surgery benefit from faster recovery, less pain, and a faster return to normal daily activities than do patients who undergo conventional open surgery.1–4 Unfortunately, the increasing success enjoyed by general surgeons in the use of the laparoscope for intestinal perforative diseases has not permeated to its use for the small bowel (SB) perforation, although perforated peptic ulcer and colonic perforation have been repaired laparoscopically since the early 1990s.2,3,5–11
Small bowel perforation, which has been dealt with traditionally by open exploration, still remains a challenge for general surgeons especially in limiting wound-related complications. Wound infection still remains the major reason for morbidity in these patients and may often be so severe as to lead to burst of the abdomen. The purpose of this study was to extend the benefit of minimally invasive surgery (MIS) to traumatic and typhoid SB perforation from the viewpoint of decreasing the postoperative wound complications and hospital stay.
METHODS
Twenty patients with typhoid ileal perforation and 5 patients with traumatic small bowel perforation were included in the study from 2000 to 2003. Twenty-two patients were male, and the average age of presentation was 29.3 years. Only patients presenting within 96 hours of perforation were included in the study group (Table 1). The reference point taken was the time of onset of severe abdominal pain or the time of injury. All patients with traumatic small bowel perforation sustained injury as a result of blunt trauma to the abdomen. The patients with trauma in addition had a computed tomographic scan to rule out retroperitoneal injury. Preoperatively, all patients were resuscitated with IV fluids, appropriate antibiotics, nasogastric tube aspiration, and were catheterized.
Table 1.
Results of Laparoscopic Repair of Small Bowel Perforation
| Nature of Perforation | No. of Patients | Avg. Time of Presentation | Length of Operation (min) | Length of Hospital Stay (days) | Complications |
|---|---|---|---|---|---|
| Typhoid ileal perforation | 20 | 3–5 | 45–92 | 7–10 | 10-mm port site infections: 2 |
| Traumatic | 5 | ||||
| Ileal | 4 | 2–3 | 45–90 | 7–10 | |
| Jejunal | 1 | 2 | 50 | 8 |
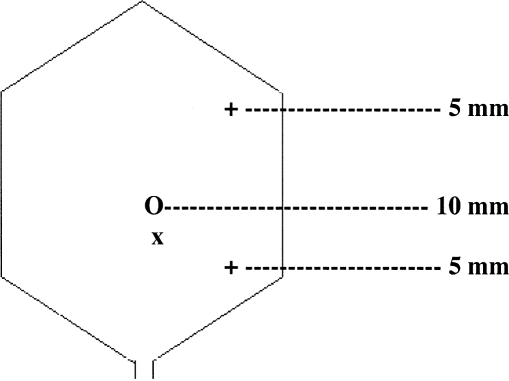
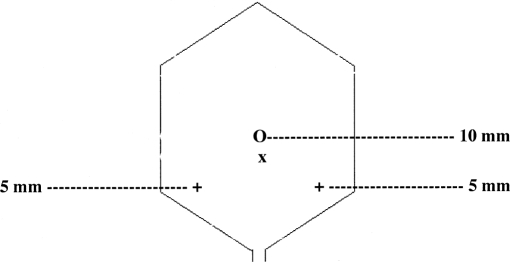
All patients were then explored laparoscopically. Pneumoperitonium was created with carbon dioxide insufflations, and a first 10-mm port was introduced infraumbilically. A second 5-mm port was then introduced in the left iliac fossa. A diagnostic exploration was then carried out and site of perforation identified. The third port was then positioned, depending on the site of perforation. For all ileal perforations (including enteric and traumatic), the 5-mm port was positioned in the left hypochondrium and for traumatic jejunal perforation the third 5-mm port was introduced in the right iliac fossa. The perforations were then repaired with single-layer Polydioxanone 3– 0 sutures applied intracorporeally. After a thorough peritoneal lavage, the rectovesical/rectouterine pouch of Douglas was drained by a PVC tube drain. Time of operation ranged from 45 minutes to 92 minutes.
RESULTS
Twenty-five patients with typhoid ileal and traumatic small bowel perforation were included in the study. One patient with typhoid perforation presented with 2 perforations. The average time of presentation in patients with typhoid ileal perforation was 3 days to 5 days. Patients with traumatic perforation, however, presented early within 2 days to 3 days. Only those patients presenting within 4 days after onset of symptoms were included in the study. Three ports were used to repair the perforations (Figures 1 and 2). All the patients with typhoid had ileal perforations while 2 patients with traumatic small bowel perforation had jejunal and the other 3 had ileal perforations. All the patients were found to have fecal peritonitis. The time of operation varied from 45 minutes to 92 minutes. Port sites were closed with PDS 3– 0 suture. The postoperative period in these patients was uneventful. The average time of postoperative hospital stay varied from 7 days to 10 days. The patients were followed postoperatively for 2 weeks following discharge from the hospital.
Figure 1.
Port sites for ileal perforation.
Figure 2.
Port sites for jejunal perforation.
Except for port-site infection in 2 patients, no major wound complications occurred. None of the patients developed postoperative fistulas, and no mortalities occurred.
DISCUSSION
The morbidity and mortality with perforative peritonitis does not need to be further emphasized. Wound-related morbidity plays a major role in delaying such patients' discharge and may even be a cause of mortality.10
The first report of laparoscopic surgery for perforative peritonitis was for a perforated peptic ulcer and appeared in the literature in the early 1990s. Nathanson, Easter, and Cuscheri,11 and Mouret and colleagues10 were among the first to report successful closure of perforated duodenal ulcers laparoscopically.2,3,5–11 Numerous other case reports and small case series soon followed for duodenal and colonic perforations.3,6,9,10,12,13 The perforations have been variously repaired laparoscopically with glue,8,9 or omental patch sticking,2,4,7,8,14 suturing,3,8 or by omental plug.9 All these studies confirmed the potential benefits of MIS in terms of reduced morbidity, less requirement of analgesics, shorter hospital stay, and quicker recovery compared with these things in open surgery.1,2,4,11
Patients with duodenal perforations when treated by open surgery are not usually associated with a high rate of wound sepsis or dehiscence mainly because of fewer chances of secondary infection, but patients with small bowel perforation and especially typhoid ileal perforation with its associated fecal peritonitis almost always have a high incidence of wound infection and various grades of wound dehiscence.
Extensive review of the literature did not reveal any reports on SB perforation being managed laparoscopically. We compared our results with the results of SB perforation managed by open surgery in various other studies and considered them as control groups.
The methods of repair, especially those utilizing the omentum, as in duodenal perforation, are not possible in the small bowel perforation. All the perforations were thus sealed with single- or more interrupted full-thickness sutures. A careful analysis of results of open surgery reveals that wound-related morbidity, which includes wound infection and various grades of wound dehiscence may be as high as 66% to 95%.15,16 Wound infection leads to persistent septicemia and is often fatal when it becomes a complete dehiscence. This could be offset in a major way by laparoscopic intervention. Postoperative fistula formation more often than not is a result of a fresh perforation rather than a leak from the original site, and its incidence would not be affected by surgical or laparoscopic intervention. But the wound infection and dehiscence-related complications are altered remarkably. Thus, compared with the above-quoted wound infection rate, we had an infection rate of only 3 of 25 patients (12%).
However, laparoscopic intervention too has its limitations. The main limitation is adhesions, which in turn are related to the time interval of presentation. Thus, patients presenting within 96 hours of the catastrophe are more easily manageable laparoscopically. Patients presenting beyond this time interval usually develop more dense small bowel adhesions, and their adhesiolysis becomes problematic laparoscopically as edematous bowel is always susceptible to traction injury during manipulation. Because we are occasionally managing traumatic SB perforations and enteric perforations laparoscopically, the results of postoperative fistulas cannot be properly interpreted. SB perforations as a result of other causes like solitary ischemic perforations, sharp injury, and tubercular perforations can all be treated similarly in select cases.
Thus, apart from the potential benefits of shorter hospital stay, postoperative comfort, quicker recovery, and less postoperative pain, a major advantage is the remarkably low morbidity and mortality.
CONCLUSION
Based on our study, we conclude that laparoscopic intervention in SB perforation is technically feasible and that it yields favorable outcomes, especially with regards to wound complications that are a major factor influencing the morbidity in such patients. As the surgical technique matures and laparoscopic instruments improve, such procedures will likely become safer. It is our hope that increasing numbers of patients with SB perforation will be able to receive the benefits of laparoscopic repair in the near future.
References:
- 1. Druart ML, Var Hee R, Etienne J, et al. Laparoscopic repair of perforated duodenal ulcer: a prospective multicenter clinical trial. Surg Endosc. 1997;11:1017–1020 [DOI] [PubMed] [Google Scholar]
- 2. Kathkhouda N, Movor E, Mason RJ, Campos GM, Soroshyari A, Berne TV. Laparoscopic repair of perforated duodenal ulcers. Outcome and efficacy in 30 consecutive patients. Arch Surg. 1999;134:845–850 [DOI] [PubMed] [Google Scholar]
- 3. Lau WY, Leung KL, Kwong KH, et al. A randomized study comparing lap vs. open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996;224:131–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. So JB, Kum CR, Fernandes ML, Goh P. Comparison between laparoscopic and conventional omental patch repair for perforated duodenal ulcer. Surg Endosc. 1996;10:1060–1063 [DOI] [PubMed] [Google Scholar]
- 5. Laws HL, McKernan JB. Endoscopic Management of peptic ulcer disease. Ann Surg. 1993;217:548–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kathkouda N, Mouriel J. A new technique of surgical treatment of chronic duodenal ulcer without laparotomy by video coelioscopy. Am J Surg. 1991;161:361–364 [DOI] [PubMed] [Google Scholar]
- 7. Lau WY, Leung KL, Zhu XL, Lam YH. Lap repair of perforated peptic ulcer. Br J Surg. 1995;82:814–816 [DOI] [PubMed] [Google Scholar]
- 8. Lee PY, Lang KL, Lai PB, Lau JW. Selection of patients for lap repair of perforated Peptic ulcer. Br J Surg. 2001;88:133–136 [DOI] [PubMed] [Google Scholar]
- 9. Mouiel J, Kathkhouda N. Lap repair truncal and selective vagotomy. In: Zucker KA, Bailey RW, Reddick EJ. eds. Surgical Laparoscopy. St. Louis, MO: Quality Medical Publishing; 1991; 263–279 [Google Scholar]
- 10. Mouret P, Francois V, Vignal J, Barth X, Lombard-Platet R. Laparoscopic treatment of perforated peptic ulcer. Br J Surg. 1990;77:1006. [DOI] [PubMed] [Google Scholar]
- 11. Nathanson LK, Easter DW, Cuchieri A. Laparoscopic repair / peritoneal toilet of perforated duodenal ulcer. Surg Endosc. 1990;4:232–233 [DOI] [PubMed] [Google Scholar]
- 12. Sunderland GT, Chisholm EM, Lau WY, Chung SC, Li AK. Lap repair of perforated peptic ulcer. Br J Surg. 1992;79:785. [DOI] [PubMed] [Google Scholar]
- 13. Walsh CJ, Khoo DE, Motson RW. Laparoscopic repair of perforated peptic ulcer. Br J Surg. 1993;80:127. [PubMed] [Google Scholar]
- 14. Darzi A, Cheshire NJ, Somers SS, Super PA, Gwillou PJ, Monson JR. Lap omental patch repair of perforated duodenal ulcer with an automated stapler. Br J Surg. 1993;80:1552. [DOI] [PubMed] [Google Scholar]
- 15. Ajao OG. Typhoid Perforation: Factors effecting mortality and morbidity. Int Surg. 1982;67:317–319 [PubMed] [Google Scholar]
- 16. Adesunkanmi ARK, Ajao OG. The prognostic factors in typhoid ileal perforation—A prospective study of 50 patients. J R Coll Surg Edinb. 1997;42:395–399 [PubMed] [Google Scholar]