Abstract
Objectives:
In the current climate of increasing awareness, patients are demanding more knowledge of the operative process. We report a new protocol for consenting patients. In addition to the normal consent process, patients are invited to watch a video of the operation to gain a perspective of what is involved. We applied this novel method of consent and assessed its impact on patient satisfaction.
Methods:
As part of postoperative follow-up, prospective data from 43 consecutive laparoscopic patients was obtained in the form of a self-constructed, patient-directed questionnaire regarding the consenting process. Patients were also invited to complete the Client Satisfaction Questionnaire (CSQ-8) 4 weeks after their operation. Laparoscopic workload included nephrectomy (n=27), deroofing of cysts (n=2), pyeloplasty (n=6), exploration for undescended testis (n=6), lymph node dissection (n=1), and nephropexy (n=1). To reduce bias, an individual independent of the team treating the patient conducted these surveys.
Results:
All study participants read the information leaflet before laparoscopic surgery, and 81% thought we should give patients the option to watch a video before their surgery. The leaflet information was understood by 92% of patients. All patients who opted to watch a video found it helpful to their understanding, and 75% requested a copy of the video of their own operation. The mean patient satisfaction (CSQ-8) score was 29.8 of a possible maximum score of 32.
Conclusions:
This novel approach to informed consent has had a positive impact on the patient journey as is evident from high satisfaction scores. Additional randomized, controlled trials need to be conducted to evaluate video consenting methods in laparoscopic urology.
Keywords: Video consent, Laparoscopic urology, Patient satisfaction, CSQ-8 questionnaire
INTRODUCTION
In the current era of increased awareness, patients are demanding more knowledge about their operative procedure. The prospect of surgery is often frightening, and fear can be alleviated to a certain extent by a clear and thorough informed consent process. The information provided needs to be simple but comprehensive and balanced. Patients are then able to grasp what is involved, understand potential complications with their respective incidences, and make logical, rational decisions.
The British Medical Association's working party on consent stated that “current awareness of the relevant ethical and legal principles relating to consent among the medical profession is largely inadequate.”1 The working party proposed that the consent process should give patients the opportunity to express concerns about treatment. In 2002, new consent forms were introduced in the United Kingdom with checklists incorporated to make sure clinicians offered the appropriate information. A study of the quality of written information provided to patients before surgery found much information inadequate, especially regarding the risks of treatment.2
Within our laparoscopic unit in the urology department at Guy's Hospital, we found that during the traditional consenting process, patients were having difficulty in retaining the vast load of information presented to them. In addition, patients often could not visualize how the procedure would take place through small incisions. We therefore decided to address this issue with the addition of a video-assisted informed consent process working on the principle that “a video means more than a thousand words.”
METHODS
In addition to the new United Kingdom consent forms and a laparoscopic information leaflet, the patient consent process was modified to include a video presentation of the important points of the procedure. This video detailed insertion of ports, creating a pneumoperitoneum, examples of dissection, removal of the organ (if appropriate), and skin closure. In addition, patients were educated about postoperative pain, approximate length of time in the surgical theater, hospital stay, time to full recovery, and wound management.
The video was shown to patients on their day of admission to the hospital if they so desired. A member of the laparoscopy team who was able to answer any queries the patients had supervised the viewing. During and after the video presentation, the patient was informed of the relevant potential complications and benefits.
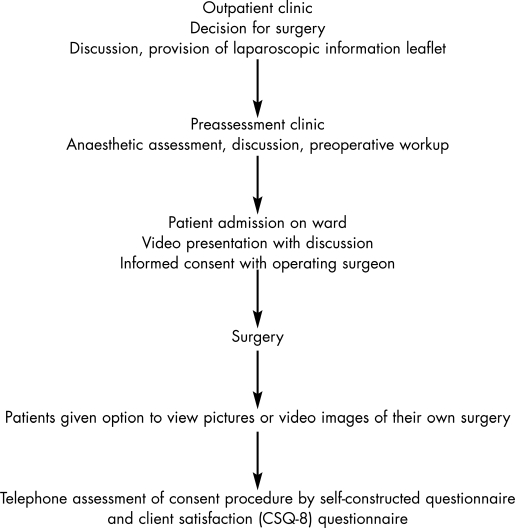
For this pilot study, we recruited 51 consecutive laparoscopic urology patients, irrespective of indication, and applied our novel method of informed consent. We gave patients the option of viewing the video presentation or declining, depending on their feelings. All other aspects of the consent process were unchanged. All patients attended a preassessment clinic to analyze the feasibility for surgery, read patient information leaflets specific to their procedure, and finally to provide consent after the video presentation by the operating surgeon on the ward a day before surgery. Patients were given the opportunity to ask questions at each step of the process (Figure 1).
Figure 1.
Flow chart summary: patient education and study design.
Eight patients could not be contacted, and so data were collected on 43 patients undergoing nephrectomy (giant hydronephrosis n=6; small nonfunctioning kidney n=11; kidney confined cancer n=10), deroofing of renal cysts (n=2), pyeloplasty (n=6), exploration of intraabdominal testes (n=6), lymph node dissection (n=1), and nephropexy (n=1), all performed laparoscopically. Four weeks after surgery, prospective data were collected in the form of a telephone based self-constructed, patient-directed questionnaire regarding the consenting process. Patients were also invited to complete the validated Client Satisfaction Questionnaire (CSQ-8). To remove bias, an individual independent of the team treating the patient conducted these surveys.
RESULTS
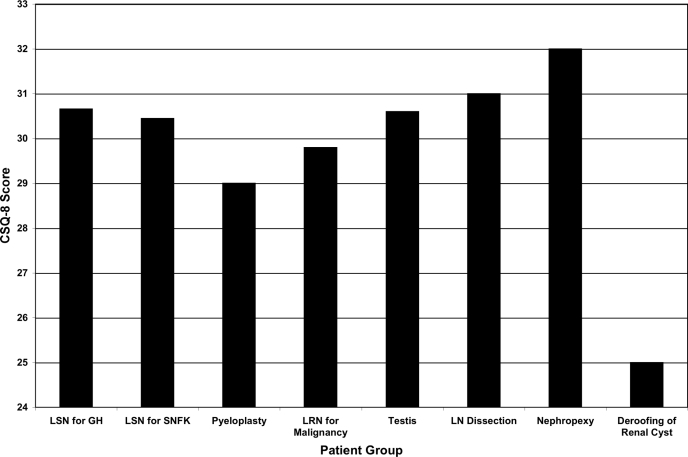
Of the 43 patients, 14 were male and 29 were female, with a mean age of 44 years. The mean patient satisfaction score (CSQ-8) for all groups was 29.8 of a possible maximum of 32. The CSQ-8 scores for the individual groups can be seen in Figure 2. Fifteen percent failed to read the patient information leaflet before their procedure despite being given it to read, while 8% despite reading the leaflet did not feel happy that they understood the information contained inside it. However, they were happy that they received enough information about the operation from other formats of the consent process. Thirty-three percent said they would feel uncomfortable if they watched a video of the proposed surgery and decided against seeing it as part of their consent process. Ninety-five percent of patients who saw a video found it useful. Eighty-one percent felt that showing a video preoperatively to all laparoscopic patients would be of great value to their understanding of the procedure. Perhaps most interestingly, 75% of patients stated that they would like to take home a copy of a video of their own operation. The results of quality of life assessment using the short form questionnaire (SF-8) in this patient population are the subject of a separate report.
Figure 2.
Mean Client Satisfaction (CSQ-8) scores depending on type of laparoscopic surgery. LSN = laparoscopic simple nephrectomy; GH = giant hydronephrosis; SNFK = small, nonfunctioning kidney; LRN = laparoscopy radical nephrectomy; LN = lymph node.
DISCUSSION
With increasing awareness and availability of unsolicited information on the Internet, patients need to be given appropriate, clear information to aid their decision process. As the procedures get more advanced and technical, they necessitate a more sophisticated understanding of the process before a patient can consent to it. One such field is laparoscopic surgery, where the patient undergoes a major operation through relatively small incisions and thus finds it hard to understand the magnitude of care needed postoperatively. In the last decade as the emphasis on informed consent has increased, newer tools are being used and identified to aid the decision process. These decision aids can be of different types. The most commonly used in the NHS are information leaflets, but their role has been limited because differences in age, sex, and socioeconomic classes require different levels of information. They are also not suitable for people with impaired cognitive function or those who are unable to read.
O'Connor et al3 reviewed the literature on decision aids used in health care and prepared an inventory of the various types available or developed. Over 200 decision aids were identified; however, only 131 were available. Some of the newer decision aids include audiovisual presentations followed by discussions between patients and the surgical team. These presentations are easier to understand and can divulge comprehensive information in a simple fashion. The conclusions drawn from this review were that randomized, controlled trials consistently demonstrate that decision aids improve the patient's knowledge regarding options, thus enhancing realistic expectations about the benefits and potential side effects. Decision aids reduce decisional conflict and improve patient participation in decision making compared with traditional methods of consenting. This metaanalysis also concluded that patients giving consent in the traditional manner had less than adequate knowledge and understanding of probable outcomes. Williams et al4 also reported that when assessing essential educational components of the consent process, such as the operation, the anesthetic, time spent in the operating theater, amount of postoperative pain, duration of hospital admission, and time required to return to normal fitness, 60% of patients responded that nobody had provided an adequate explanation.
Laparoscopic surgery allows video footage to be easily obtained for the purposes of education and operator appraisal. These should be coded with patient consent and be made anonymous. For this pilot study, we chose an audiovisual presentation using video clips from laparoscopic urological procedures. The hypothesis was that this would improve patient's knowledge and understanding and aid the process of informed consent. To our knowledge, this is the first such study in the expanding field of laparoscopic urology.
Agre et al5 have also reported on the successful implementation of video presentations to augment the consent process. In their study, patients were randomized into video and discussion, video alone, and discussion alone, when consenting for colonoscopy. All patients then filled a knowledge-based questionnaire. Patients in the 2 groups who were shown the video presentation scored significantly better than those in the discussion-only group. Another randomized, controlled study by Mason et al,6 using additional video for information as part of the consenting process in patients undergoing a laparoscopic technique for sterilization, showed that patients who watched the video were better informed compared with controls.
Marteau et al7 felt that too much information about potential adverse effects and complications may lead to increased fear and anxiety among patients with the possibility of refusal of necessary treatment. However, Mason et al6 showed that the anxiety scores between the patients providing consent with a videotape or with discussion alone were not significant, suggesting that the process of watching the video did not increase the anxiety levels.
With the recent increase in awareness of medical negligence and need for better doctor-patient communication, it is becoming imperative to judge our practices from the patient's point of view as well as clinical outcomes. Hospitals are following industry's example and adopting various client satisfaction assessment tools to understand and improve services from a patient perspective. To assess the impact of our consenting process, we adopted the client satisfaction questionnaire (CSQ-8). This is a validated shortened version of the original 36-item measure. The CSQ-8 can be used to assess patient satisfaction in most clinical settings and is a direct measure in which patients are asked to think about the services they have received from a particular program or kind of care.8
The mean CSQ-8 score of 29.8 out of a maximum of 32 indicates a high level of satisfaction for patients using this service. The vast majority (95%) of patients who watched the video felt that it helped their understanding of the operation. Most patients in this study felt that future patients who were to undergo laparoscopic urological procedures should be shown a video, although they stated that the patients should be given the option to decline to view it if they felt viewing it might heighten their anxiety.
We feel that video consent is beneficial to patient understanding of their procedure. The initial feedback from the patients and the operators has helped us in refining the content of the video presentation. We plan to utilize this novel method for all future laparoscopic cases within our department.
We are aware of the limitations of this study; therefore, a randomized, controlled trial comparing conventional and video-assisted consent in laparoscopic urology with subsequent assessment of patient knowledge of the procedure is planned.
CONCLUSION
Video consent is a novel method of informed consent in laparoscopic urology. Feedback from patients and operators suggests that this method can be of benefit to patients. This has had a positive effect on the patient journey as evidenced by high satisfaction scores. This method needs to be further evaluated by randomized, controlled studies.
Contributor Information
Arun Sahai, Department of Urology, Guy's Hospital and St. Thomas’ NHS Trust and GKT School of Medicine, London, UK..
Rajesh Kucheria, Department of Urology, Guy's Hospital and St. Thomas’ NHS Trust and GKT School of Medicine, London, UK..
Ben Challacombe, Department of Urology, Ashford Hospital, Kent, UK..
Prokar Dasgupta, Department of Urology, Guy's Hospital and St. Thomas’ NHS Trust and GKT School of Medicine, London, UK..
References:
- 1. General Medical Council Seeking patients’ consent: the ethical considerations. London: General Medical Council; 1998 [Google Scholar]
- 2. Coulter A, Entwhistle V, Gilbert D. Informing patients: an assessment of the quality of patient information materials. London: King's Fund Publishing; 1998 [Google Scholar]
- 3. O'Connor AM, Stacey D, Entwistle V, et al. Decision aids for people facing health treatment or screening decisions (Cochrane Review). The Cochrane Library, Issue 1 Chichester, UK: John Wiley & Sons, Ltd; 2004 [Google Scholar]
- 4. Williams OA. Patient knowledge of operative care. J R Soc Med. 1993; 86: 328–331 [PMC free article] [PubMed] [Google Scholar]
- 5. Agre P, Kurtz RC, Krauss BJ. A randomised trial using videotape to present consent information for colonoscopy. Gastrointest Endosc. 1994; 40: 271–276 [DOI] [PubMed] [Google Scholar]
- 6. Mason V, McEwan A, Walker D, Barrett S, James D. The use of video information in obtaining consent for female sterilisation: a randomised study. BJOG. 2003; 110: 1062–1071 [PubMed] [Google Scholar]
- 7. Marteau TM, Kidd J, Michie S, Cook R, Johnston M, Shaw RW. Knowledge and satisfaction in women receiving false positive results on routine pre-natal screening. A randomised controlled trial. J Psychosom Obs Gyn. 1993; 14: 185–196 [DOI] [PubMed] [Google Scholar]
- 8. Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine. 2000; 25: 3167–3177 [DOI] [PubMed] [Google Scholar]