Abstract
Laparoscopy is now considered the gold standard for treating benign monolateral adrenal lesions. We present the case of a patient affected by Cushing's syndrome due to large bilateral adrenal adenomas (7.5cm) who underwent simultaneous laparoscopic bilateral adrenalectomy. An anterior, lateral transperitoneal approach was used. Operative time was 200 minutes, and blood loss was 200mL. No intraoperative complications were encountered. The postoperative course was uneventful, and the patient was discharged after 3 days. Laparoscopic bilateral adrenalectomy is a safe, effective procedure when performed by experienced hands and may be an alternative treatment for large adrenal lesions.
Keywords: Bilateral laparoscopic adrenalectomy, Large adrenal lesions
INTRODUCTION
Laparoscopic adrenalectomy (LA) is at present considered the gold standard for treating all small (<6cm) benign adrenal tumors; it guarantees decreased perioperative morbidity, postoperative disability and discomfort, as well as shorter hospital stay compared with the open approach.1–4
Several recent studies, reviewing laparoscopic adrenalectomies performed for large (>6 cm) and potentially malignant adrenal lesions,5–7 demonstrated that LA performed by experienced hands can be a feasible, safe procedure in terms of operative and postoperative outcomes, and can be extended to any adrenal tumor, as long as no radiological evidence is present of periadrenal infiltration or venous invasion.8,9
Although the benefits of unilateral LA have been well documented, only a few cases of simultaneous bilateral LA have been reported. Bilateral LA is, in fact, an uncommon occurrence and is frequently performed as a staged (metachronous) procedure to avoid prolonged operating time and to minimize morbidity.10 The management of bilateral adrenal disease has been traditionally approached by means of open surgery, with no definitive consensus regarding the feasibility and effectiveness of the laparoscopic approach.
Herein, we discuss our experience with LA11,12 reporting the case of a simultaneous, bilateral laparoscopic transperitoneal adrenalectomy performed for 2 voluminous adenomas in a patient with Cushing syndrome.
CASE REPORT
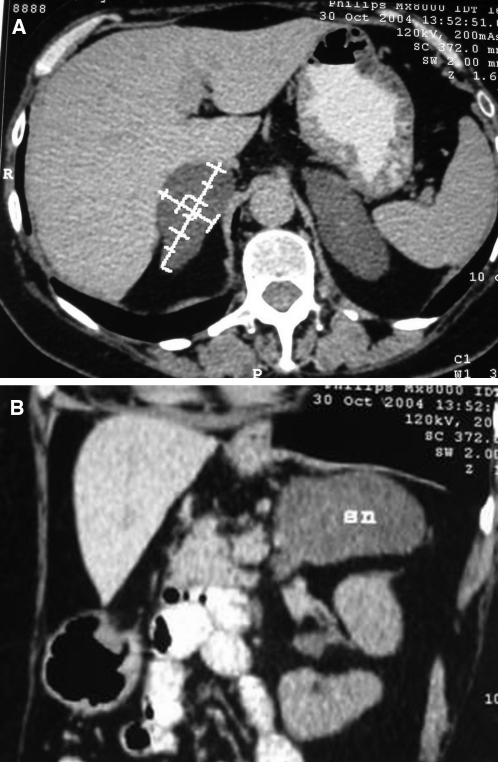
In November 2004, a 53-year-old woman was admitted to our department with signs and symptoms of Cushing's syndrome. Clinical features were moon facies, buffalo humps, and central obesity. She had gained 3 kg of body weight during the previous year, and complained of muscle weakness since 2002. She had also suffered from hypertension for the past 3 years. The serum cortisol basal level was 260 ng/mL (normal range, 50 to 250), and urinary free cortisol excretion was elevated (195 μg/24h). Serum cortisol levels were 959 nmol/L at 8:00, 705 nmol/L at 12:00, and 686nmol/L at 23:00. The serum basal level of ACTH was 4.70 pg/mL (normal range, 10 to 90), and it was <5 pg/dL at 8:00, 12:00, and 23:00. Plasma cortisol level was not suppressed after a high-dose overnight dexamethasone suppression test: 919nmol/L after 8mg. These findings suggested excessive autonomous secretion of cortisol from the adrenal tissues. An abdominal CT scan showed 2 large bilateral adrenal masses both 7.5 cm in diameter, compatible with benign adrenal adenomas (Figures 1 and 2). Adrenocortical scintigraphy confirmed this diagnosis.
Figure 1.
High-resolution abdomen computed tomographic scan, particularly of the adrenal glands.
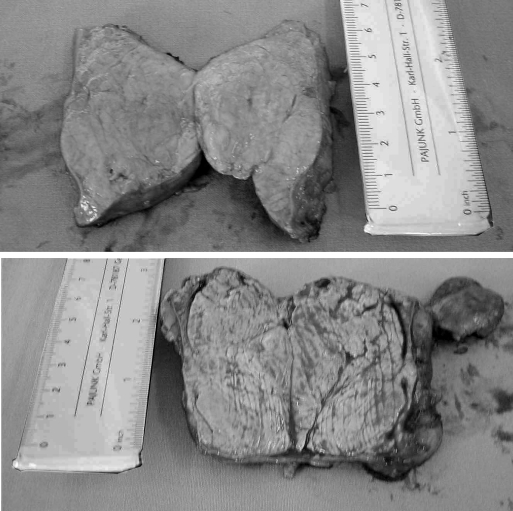
Figure 2.
Gross appearance of surgically resected adrenal gland.
The patient underwent simultaneous bilateral laparoscopic transperitoneal adrenalectomy.
An anterior, lateral transperitoneal approach was performed with the patient in a lateral decubitus position to allow gravity-facilitated exposure of the adrenal gland. The costoiliac space was opened by elevation of the contralateral flank and by the lowering of the legs.
The procedure began with the right adrenalectomy; the liver was mobilized using a fan retractor until the subhepatic area was discovered. The right triangular ligament was incised. The dissection began by creating a hockeystick-shaped incision with sharp dissection and with the Harmonic scalpel, along the retroperitoneal attachment of the right lobe of the liver, and the lateral border of the inferior vena cava. Tissue dissection along the lateral rime of the inferior vena cava allowed the identification of the transversely oriented short adrenal vein, which was clipped and divided. Then, by dissecting from medial to lateral and from inferior to superior, using the kidney as a dissection plane, the gland was mobilized by blunt dissection and electrocautery of vessels until it was completely free.
For left-sided procedures, the first step was to incise the lienal attachments to the diaphragm along the lateral border of the spleen and the splenocolic ligaments. The dissection was stopped when the tail of the pancreas was identified posteriorly. Once the spleen was mobilized, it was moved medially with the short gastric vessels, and the adrenal area was viewed. By dissecting the inferior and the medial border of the gland, the vein was isolated and clipped close to the gland. Then, the dissection was continued from inferior to superior and from medial to lateral following the anterior surface of the kidney. The gland was finally cleaned of the small vessels by a Harmonic scalpel, while any accessory vein or larger artery was clipped and divided. At the end of the procedure, both tumors were removed in a retrieval bag through a 6-cm incision in the left iliac fossa.
The operative time was 200 minutes; blood loss was 200cc. No intraoperative complications were encountered. The pathology examination confirmed the 2 masses as being benign adenomas. The postoperative course was uneventful, and the patient was discharged after 3 days.
DISCUSSION
Since 1992,4 laparoscopic adrenalectomy (LA) has been considered the first-line treatment in patients with virtually any adrenal tumour. Compared with open adrenalectomy, LA offers less perioperative morbidity and mortality, a shorter length of hospitalization and better cosmetic results13,14 LA was promptly introduced in our department as a relatively simple ablative procedure with no reconstructive time needed. From 1994 to 2003, 50 patients underwent laparoscopic adrenalectomy in the Department of Surgery “Pietro Valdoni,” University of Rome “La Sapienza.”11,12
Presenting the case of a simultaneous, bilateral laparoscopic transperitoneal adrenalectomy performed for 2 voluminous adenomas in a patient with Cushing's Syndrome, we evaluated the safety and feasibility of monolateral or bilateral LA, for large-volume adrenal masses, focusing the discussion on the operative, postoperative, and oncological aspects.
Some authors6,15 suggest that patients with benign adrenal lesions larger that 5cm to 6cm should not be treated with LA because of the longer operative time and the high risk of bleeding represented by the numerous vessels that usually surround the neoplasia.
However, recent reports2,3,7 showed that LA for large and radiological benign tumors is technically feasible and safe. In these studies, no correlation exists between tumor size and blood loss, morbidity and mortality rate, and hospital stay. Porpiglia2 demonstrated only a slight correlation between tumor size and operative time.
Hobart16 compared retrospectively the results of 3 different groups of patients; first group (14 patients) underwent LA for large-volume adrenal lesions (>5cm), a second group (14 patients) treated with open adrenalectomy for large adrenal masses, and a third group (45 patients) underwent LA for small adrenal masses (<5cm). He shows, for the first group, a higher complication rate (21.4% vs 8.9%) compared with the third group, but lower (21.4% vs. 50%) compared with the open technique (second group). Hobart described also, for the first group, a higher operative time (205 min vs 158 min) compared with time for the third group but lower compared with time for the second group (205 min vs 216 min); a blood loss of 400mL for the first group and of 584mL for the second one; a length of hospitalization of 2.4 days for the first group versus 7.7 days for the second group.
Eventually, the risk for the surgeon, during laparoscopic dissection of a large adrenal tumor, is the possibility of treating an unknown adrenal cortical cancer (ACC), a risk that Grumbach17 observed as being clearly related to tumor size.
Copeland,18 by examining the data from 6 series of patients with adrenal tumors, reported that 92% of 114 ACC were >6 cm. Ross and Aron19 calculated that in the absence of radiological features of malignancy, less than 1 in 10 000 adrenal neoplasms >6 cm are carcinomas, concluding that the likelihood of ACC for masses >6 cm is between 35% to 98%.
Imaging studies can help surgeons evaluate malignant lesions; abdominal ultrasound, CT, and MRI scans can demonstrate irregular tumor margins, local invasion of the periadrenal tissue, heterogeneity and hyperdensity, although these features of malignancy may also be observed in benign tumors.20
Kebebew et al,21 however, analyzing a series of 20 LA performed for suspected and unsuspected malignant adrenal tumors, found a 65% rate of overall disease-free survival at a mean follow-up of 3.3 years and a 60% rate of locoregional recurrence; these rates are similar to the reported open adrenalectomy rates.21 Henry et al,7 in a series of LA for tumors >6cm that included 6 cases of reported ACC, reported at a mean follow-up of 34 months one patient death and 5 disease-free patients.
The bilateral synchronous laparoscopic adrenalectomy literature offers just a few reports. Up to now, bilateral laparoscopic adrenalectomy has been reported in cases of Cushing's syndrome after failed transsphenoidal ablation for a pituitary adenoma,23–26 Cushing's syndrome is due to an ectopic adrenocorticotropic hormone (ACTH)-producing tumor,27 macronodular adrenal hyperplasia,28 some types of congenital adrenal hyperplasia,29–31 and phaeochromocytoma, either with or without multiple endocrine neoplasia type 2.32 These earlier studies showed that the bilateral procedure is feasible and safe. However, Porpiglia et al33 recently reported that laparoscopic bilateral adrenalectomy can be safe and effective, but longer operatives times than those for open surgery may represent a limitation especially in high-risk patients. Also Hsu,34 comparing synchronous with metachronous laparoscopic procedures, suggests that in synchronous bilateral adrenalectomy the surgical time was longer, but no differences were noted in intraoperative blood loss, postoperative resumption of oral intake, physical activity, analgesia requirement, hospital stay, and convalescence. We suggest that in a planned synchronous bilateral laparoscopic procedure, close monitoring of the cardiopulmonary status of the patient is mandatory, and the surgeon must be prepared to postpone the second procedure to a later date, on the basis of the intraoperative course during the first procedure. Therefore, the patient must be so counseled preoperatively.
In our patient, preoperative investigation demonstrated a well-compensated cardiopulmonary status. Laboratory tests (hormones serum levels) and the radiological findings clearly demonstrated 2 large bilateral adrenal masses both of 7.5cm in diameter, compatible with benign adrenal adenomas.
CONCLUSION
LA for large, bilateral adrenal masses is a feasible and safe procedure and may be a valid alternative treatment, offering the advantages of the laparoscopic approach. Data reported in the literature, suggest that preoperatively an accurate evaluation of patient's clinical status is necessary as is an accurate radiological study of the adrenal lesion (TC and MRI) with a view of demonstrating local, vascular infiltration, and distant metastases, which represent absolute contraindications for LA. Once this eventuality can be ruled out, the indication is to convert the procedure into open adrenalectomy if there is, intraoperatively, any difficulty in dissection that may jeopardize incomplete resection of the tumour, or if patient's cardiopulmonary status could be compromised by a longer operative time.
References:
- 1. Sturgeon C, Kebebew E. Laparoscopic adrenalectomy for malignancy. Surg Clin N Am. 2004; 84: 755–774 [DOI] [PubMed] [Google Scholar]
- 2. Porpiglia F, Destefanis P, Fiori C, et al. Does adrenal size really affect safety and effectiveness of laparoscopic adrenalectomy? Urology. 2002; 60 (5): 801–805 [DOI] [PubMed] [Google Scholar]
- 3. Novitsky YW, Czerniach DR, Kercher KW, Perugini RA, Kelly JJ, Ltwin DE. Feasibility of laparoscopic adrenalectomy for large adrenal masses. Sur Laparosc Endosc Percut Tech. 2003; 13: 106–110 [DOI] [PubMed] [Google Scholar]
- 4. Gagner M, Lacroix A, Bolte E. Laparoscopic adrenalectomy in Cushing's syndrome and Phechromocytoma. N Engl J Med. 1992; 327: 1033. [DOI] [PubMed] [Google Scholar]
- 5. Hazzan D, Shiloni E, Golijamin D, Jurim O, Gross D, Reissman P. Laparoscopic versus open adrenalectomy for benign adrenal neoplasm: a comparative study. Surg Endosc. 2001; 15: 1356–1358 [DOI] [PubMed] [Google Scholar]
- 6. Terachi T, Matsuda T, Terai A, et al. Transperitoneal laparoscopic adrenalectomy: experience in 100 patients. J Endourol. 1997; 11: 361–365 [DOI] [PubMed] [Google Scholar]
- 7. Henry JF, Sebag F, Iacobone M, Mirallie E. Results of laparoscopic adrenalectomy for large potentially malignant tumors. World J Surg. 2002; 26: 1043–1047 [DOI] [PubMed] [Google Scholar]
- 8. Gagner M, Lacroix A, Printz RA, et al. Early experience with laparoscopic approach for adrenalectomy. Surgery. 1993; 114: 1120–1125 [PubMed] [Google Scholar]
- 9. Gagner M, Pomp A, Heniford BT, Pharand D, Lacroix A. Laparoscopic adrenalectomy: lesson learned from 100 consecutive procedures. Ann Surg. 1997; 226: 238–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Soulie M, Mouly P, Caron P, et al. Retroperitoneal laparoscopic adrenalectomy: clinical experience in 52 procedures. Urology. 2000; 56: 921–925 [DOI] [PubMed] [Google Scholar]
- 11. Ramacciato G, Lombardi M, Amodio PM, et al. Laparoscopic adrenalectomy: a worthwhile procedure performed in a general surgery department. Am Surg. 2003; 69: 427–433 [PubMed] [Google Scholar]
- 12. Ramacciato G, Mercantini P, Amodio PM, et al. Ten years of laparoscopic adrenalectomy; lesson learned from 104 procedures. Am Surg. 2005; 71 (4): 321–325 [PubMed] [Google Scholar]
- 13. Assalia A, Gagner M. Laparoscopic adrenalectomy. Br J Surg. 2004; 91: 1259–1274 [DOI] [PubMed] [Google Scholar]
- 14. Lal G, Duh QY. Laparoscopic adrenalectomy: indications and technique. Surg Oncol. 2003; 12: 105–123 [DOI] [PubMed] [Google Scholar]
- 15. Terzolo M, Pia A, Berruti A, et al. Low-dose monitored mitomane treatment achieves the therapeutic range with manageable side effect in patients with adrenocortical carcinoma. J Clin Endocrinol Metab. 2000; 85: 2234–2238 [DOI] [PubMed] [Google Scholar]
- 16. Hobart MG, Gill IS, Schweizer D, Sung T, Bravo EL. Laparoscopic adrenalectomy for large-volume (> or =5 cm) adrenal masses. J Endourol. 2000; 14: 149–154 [DOI] [PubMed] [Google Scholar]
- 17. Grumbach MM, Biller BM, Braunstein GD, et al. Management of the clinically unapparent adrenal masses (“incidentaloma”). Ann Intern Med. 2003; 138: 424–429 [DOI] [PubMed] [Google Scholar]
- 18. Copeland PM. The incidentally discovered adrenal mass. Ann Intern Med. 1983; 98: 940–945 [DOI] [PubMed] [Google Scholar]
- 19. Ross NS, Aron DC. Hormonal evaluation of the patient with an incidentally discovered adrenal mass. N Engl J Med. 1990; 323: 1401–1405 [DOI] [PubMed] [Google Scholar]
- 20. Bernini GP, Miccoli P, Moretti A, Vivaldi MS, Iacconi P, Solvetti A. Sixty adrenal masses of large dimensions hormonal and morphologic evaluation. Urology. 1998; 51: 920–925 [DOI] [PubMed] [Google Scholar]
- 21. Kebebew E, Siperstein AE, Clarck OH, et al. Results of laparoscopic adrenalectomy for suspected and unsuspected malignant adrenal neoplasm. Arch Surg. 2002; 137: 948–953 [DOI] [PubMed] [Google Scholar]
- 22. Acosta E, Pantoja JP, Gamino R, Rull JA, Herrera MF. Laparoscopic versus open adrenalectomy in Cushing's syndrome and disease. Surgery. 1999; 126: 1111–1116 [DOI] [PubMed] [Google Scholar]
- 23. Bax TW, Marcus DR, Galloway GQ, Swanstrom LL, Sheppard BC. Laparoscopic bilateral adrenalectomy following failed hypophysectomy. Surg Endosc. 1996; 10: 1150–1153 [DOI] [PubMed] [Google Scholar]
- 24. Chapuis Y, Pitre J, Conti F, Abboud B, Pras-Jude N, Luton JP. Role and operative risk of bilateral adrenalectomy in hypercortisolism. World J Surg. 1996; 20: 775–779 [DOI] [PubMed] [Google Scholar]
- 25. Lanzi R, Montorsi F, Losa M, et al. Laparoscopic bilateral adrenalectomy for persistent Cushing's disease after transsphenoidal surgery. Surgery. 1998; 123: 144–150 [PubMed] [Google Scholar]
- 26. Vella A, Thompson GB, Grant CS, van Heerden JA, Farley DR, Young WF., Jr Laparoscopic adrenalectomy for adrenocorticotropin-dependent Cushing's syndrome. J Clin Endocrinol Metab. 2001; 86: 1596–1599 [DOI] [PubMed] [Google Scholar]
- 27. Ferrer FA, MacGillivray DC, Malchoff CD, Albala DM, Schichman SJ. Bilateral laparoscopic adrenalectomy for adrenocorticotropin-dependent Cushing's syndrome. J Urol. 1997; 157: 16–18 [PubMed] [Google Scholar]
- 28. Shinbo H, Suzuki K, Sato T, Kageyama S, Ushiyama T, Fujita K. Simultaneous bilateral laparoscopic adrenalectomy in ACTH-independent macronodular adrenal hyperplasia. Int J Urol. 2001; 8: 315–318 [DOI] [PubMed] [Google Scholar]
- 29. Bruining H, Bootsma AH, Koper JW, Bonjer J, de Jong FF, Lamberts SW. Fertility and body composition after laparoscopic bilateral adrenalectomy in a 30-year-old female with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2001; 86: 482–484 [DOI] [PubMed] [Google Scholar]
- 30. Chabre O, Portrat-Doyen S, Chaffanjon P, et al. Bilateral laparoscopic adrenalectomy for congenital adrenal hyperplasia with severe hypertension, resulting from two novel mutations in splice donor sites of CYP11B1. J Clin Endocrinol Metab. 2000; 85: 4060–4068 [DOI] [PubMed] [Google Scholar]
- 31. Warinner SA, Zimmermann D, Thompson GB, Grant CS. Study of three patients with congenital adrenal hyperplasia treated by bilateral adrenalectomy. World J Surg. 2000; 24: 1347–1352 [DOI] [PubMed] [Google Scholar]
- 32. Fernandez-Cruz L, Saenz A, Benarroch G, Sabater L, Taura P. Total bilateral laparoscopic adrenalectomy in patients with Cushing's syndrome and multiple endocrine neoplasia (IIa). Surg Endosc. 1997; 11: 103–107 [DOI] [PubMed] [Google Scholar]
- 33. Porpiglia F, Fiori C, Bovio S, et al. Bilateral adrenalectomy for Cushing's syndrome: a comparison between laparoscopy and open surgery. J Endocrinol Invest. 2004; 27: 654–658 [DOI] [PubMed] [Google Scholar]
- 34. Hsu TH, Gill IS. Bilateral laparoscopic adrenalectomy: retroperitoneal and transperitoneal approaches. Urology. 2002; 59: 184–189 [DOI] [PubMed] [Google Scholar]