Abstract
Situs inversus is a rare anomaly characterized by transposition of organs to the opposite side of the body. In patients with this anomaly, cholelithiasis is observed with a frequency similar to that in the normal population. Herein, we report on a patient with situs inversus totalis who underwent laparoscopic cholecystectomy for mucocele of the gallbladder. Diagnostic pitfalls and technical difficulties of the operation with technical options are discussed in the context of the available literature. Difficulty is encountered particularly in skeletonizing the structures in Calot's triangle, which consumes extra time and is more demanding than in patients with a normally located gallbladder. A summary of an additional 32 similar cases reported in the medical literature is also presented.
Keywords: Laparoscopic cholecystectomy, Situs inversus totalis, MRI
INTRODUCTION
Since laparoscopic cholecystectomy has become the standard procedure for the treatment of gallstone disease, several cases have been reported in patients with situs inversus. Laparoscopic cholecystectomy in these patients is technically more demanding and needs reorientation of visuomotor skills to the left upper quadrant. We herein discuss the diagnostic and technical difficulties and review the literature.
CASE REPORT
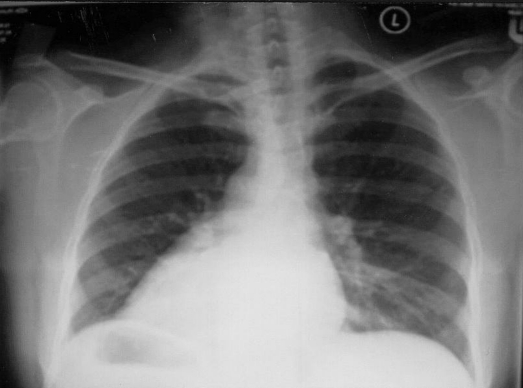
A 65-year-old lady who is epileptic presented with epigastric pain of 1-year duration. The pain was colicky in nature, prominent after meals, and had been of severe intensity in the previous few days. She was afebrile, not jaundiced, and the abdominal examination was unremarkable. A chest radiograph revealed situs inversus (Figure 1). Further evaluation with ultrasound and MRI confirmed situs inversus totalis and the presence of multiple gallstones in a distended gallbladder (Figure 2). The liver function test was normal. After providing informed consent, the patient underwent laparoscopic cholecystectomy.
Figure 1.
Chest x-ray revealing dextrocardia.
Figure 2.
Magnetic resonance image (coronal section) revealing a left sided liver and gallbladder that is distended and has multiple calculi in it.
Laparoscopic cholecystectomy was performed using a zero-degree viewing laparoscope with the patient under general anesthesia. The surgeon and the monitor assistant were positioned on the patient's right side. Pneumoperitoneum with CO2 was created with a pressure ≤12mm Hg, using a Veress needle that was inserted midline just above the umbilicus. Two 10-mm trocars were inserted into the abdominal cavity, one in the position of the Veress needle and the other in the midline in the epigastric region to the left of the falciform ligament. Two more 5-mm trocars were placed in the left subcostal in the midcostal line and anterior axillary line, respectively. On laparoscopic examination, the gallbladder was distended and densely adherent to omentum. The gallbladder was decompressed by needle aspiration. The adherent omentum and adhesions were dissected with the right hand, leading to the need to frequently cross over the hands. The cystic duct and artery were clipped and divided, and the gallbladder was dissected from the liver bed by using electrocautery and was then extracted through the epigastric port. The total duration of the surgery was 80 minutes. On gross examination, the gallbladder was found to have serous exudate and multiple gallstones that were impacted in Hartman's duct and the cystic duct. Pathological examination of the gallbladder revealed an acute or chronic cholecystitis. The postoperative period was uneventful, and the patient was discharged on the first postoperative period.
DISCUSSION
Situs inversus is a term used to describe a condition in which organs are transposed from their normal sites to locations on the opposite side of the body.1 It may include transposition of thoracic viscera, the abdominal organs, and much more commonly, both (SI totalis).1,2 In the year 1600, Fabricus reported the first case of the mirror image transposition in man. This rare condition is associated with a genetic predisposition that is autosomal recessive, occurring in 1:5000 to 1:10,000 hospital admissions.3,4 Since 1992, 32 cases of cholelithiasis in patients with SI have been reported in the English language medical literature that where treated by open surgery.3 In 1991, Campos and Sipes5 were the first to report a successful laparoscopic cholecystectomy (LC) in a patient with situs inversus totalis, and since then another 31 patients with situs inversus (Table 1)1–4,7–10,13–31 have undergone laparoscopic cholecystectomy.
Table 1.
Summary of Patients With Situs Inversus Treated by Laparoscopic Cholecystectomy
| No | Series | Year | Age/sex | Diagnosis* | Partial/Total | Time (min) | Postop stay (days) |
|---|---|---|---|---|---|---|---|
| 1. | Current study | 2005 | 65/f | Mucocele | T | 80 | 1 |
| 2. | Pitiakoudis32 | 2005 | 47/f | CC | T | 65 | 2 |
| 3. | McKay10 | 2005 | 32/f | AC | T | — | — |
| 4. | Docimo31 | 2004 | 41/f | CC | T | — | 2 |
| 5. | Kang16 | 2004 | 64/f | CC/CBD calculi | T | 240 | 7 |
| 6. | Jesudason9 | 2004 | 69/m | CC | T | — | — |
| 7. | Zan8 | 2003 | 70/f | biliary colic | T | — | — |
| 65/m | AC | T | — | — | |||
| 8. | Polychronidis14 | 2002 | 68/m | CC | T | — | — |
| 9. | Tronge A30 | 2002 | 28/f | CC | P | — | — |
| 10. | Wong J | 2001 | 68/f | CC/CBD calculi | T | ||
| 11. | Al Jumaily28 | 2001 | 46/f | microlithiasis | T | — | — |
| 12. | Yaghan RJ7 | 2001 | 48/f | CC | T | 70 | 1 |
| 38/f | AC | T | 80 | 3 | |||
| 13. | Donthi R17 | 2001 | 43/f | CC | U | — | — |
| 39/f | CC | T | — | — | |||
| 14. | Nursal TZ18 | 2001 | 42/f | CC | T | — | 1 |
| 15. | Singh K19 | 2000 | 42/f | CC | T | — | — |
| 16. | Demetriades20 | 1999 | 61/f | AC | T | — | 3 |
| 37/m | CC | T | — | 2 | |||
| 17. | Habib21 | 1998 | 45/f | CC | U | — | — |
| 18. | D’Agata22 | 1997 | 72/f | CC | T | — | — |
| 19. | Elhomsy23 | 1996 | — | AC | P | 90 | — |
| 20. | Crosher1 | 1996 | 63/m | biliary colic | T | — | 1 |
| 21. | Malatani4 | 1995 | 25/f | AC | U | 70 | 2 |
| 22. | McDermott15 | 1994 | 66/m | cholangitis | U | — | — |
| CBD calculi | |||||||
| 23. | Schiffino24 | 1993 | 53/f | CC | T | — | — |
| 24. | Huang25 | 1992 | 36/m | CC | T | — | 1 |
| 25. | Drover26 | 1992 | 29/f | CC | P | — | 1 |
| 26. | Goh27 | 1992 | 62/m | Empyema | T | — | 3 |
| 27. | Lipschutz2 | 1992 | 80/m | cholangitis | T | — | 4 |
| CBD calculi | |||||||
| 28. | Takie3 | 1992 | 51/f | biliary colic | T | — | 1 |
| 29. | Campos5 | 1991 | 39/f | CC | T | — | 1 |
AC = Acute cholecystitis, CC = Chronic cholecystitis, T = total situs inversus, P = partial situs inversus, U = unknown.
SI does not predispose one to gallbladder disease, but it leads to diagnostic confusion.3 Most patients present with left-sided upper abdominal pain.3 However, about 10% of patients with left-sided cholelithiasis present with right-sided abdominal pain.3 This phenomenon has been observed for both visceral biliary pain and somatic pain in cases of cholecystitis and suggests that the central nervous system may not share in the general transposition.6 Our patient experienced pain in the epigastric region, which is reported to occur in 30% of patients.3 A high index of suspicion is hence the key to avoiding mishaps in patients with SI presenting with an acute abdomen. Apart from the confusion related to the site of the pain, the spectrum of clinical presentation related to complications of left-sided cholelithiasis is similar to that occurring in right-handed gallbladder.3
An apical beat in the right fifth intercostal space, reversed side of the liver dullness, and the right testicle hanging lower than the left occasionally suggest SI.3 A chest radiograph and an echocardiogram revealing dextrocardia and an abdominal film demonstrating a stomach bubble on the right side can give quick diagnostic clues.7 Ultrasonography, abdominal CT, chest scan, and MRI will confirm the presence and determine the type of visceral transposition. Several reports in the literature emphasize the feasibility of safe LC in this challenging situation.
The technical difficulties merit consideration. The mirror image reversibility of the abdominal viscera requires the surgeon to stand on the right side with the video monitor above the patient's left shoulder. Two 10-mm ports are placed in the epigastric and subumbilical positions. Two 5-mm ports are placed in the midclavicular and left anterior axillary lines. The lens used could either be a 0-degree or 30° lens, though a 300 lens has been found to be superior in delineating Calot's triangle.7 The dissection of Calot's triangle could either be carried out with the right hand or the left hand. For a right-handed surgeon using the left hand, the manipulation may be cumbersome and not precise. This is most apparent during clip application where both precision and power are required. However, as in our case, using the right hand has technical difficulties of either having to cross the hands or hyperflex the trunk and strike the anesthesia screen with the left elbow. This is a tiring posture.7 From time to time, the surgeon may depend more on the midclavicular port, but this maneuver is usually limited by jamming with the camera. Hence, the skeletonizing of the structures of Calot's triangle consumes extra time and is more difficult than in patients with a normally located gallbladder. However, a left-handed surgeon has a clear advantage, because he is able to alternate the performance of dissection maneuvers between the right and left hand as has been reported in the literature.8 Some have overcome such difficulties by standing between 2 abducted lower limbs.7,9 The problem of crossing the hands to retract Hartmann's pouch while dissecting Calot's triangle has been overcome by some by allowing the first assistant to retract Hartmann's pouch while the primary surgeon dissects Calot's triangle using his right hand via the epigastric port without hindrance.10 It has also been suggested that the dissection be carried out from the left side with the right hand, by adjusting port placement.7 However, the authors feel that the tips of the instruments in this case will point towards the surgeon, who would have to hyperflex the wrists, which will limit maneuvering abilities.7
Although operating time is not recorded in all patients, the general agreement is that the procedure will be lengthier than in patients with a normally located gallbladder.7 The shortest reported time was 65 minutes.31 The need to redirect the visual-motor skills of the surgeon and the cameraman to the left upper quadrant along with the difficulty in skeletonizing Calot's triangle is responsible for the largest portion of the extra operative time.
Apart from mirror image transposition, patients with SI usually do not have associated extrahepatic biliary, venous, and arterial anomalies.3,6,11,12 Hence, it appears that the surgeon should not be discouraged from performing laparoscopic cholecystectomy for SI on the grounds of unexpected associated biliary tract anomalies. In one report, the common hepatic artery originated from the superior mesenteric artery, a variant that is known to occur in 17% of persons with normal anatomy.12 However, in patients with SI partialis, there is an increased possibility of associated biliary tract and vascular anomalies, and such patients may need intraoperative cholangiography and a low threshold for conversion to open surgery.7 However, others still feel it is safer to perform open cholecystectomy in these patients.13 There are also other extra abdominal anomalies, especially cardiac ones that are more frequent in patients with SI.7 The incidence of SI partialis is however much lower with only 3 cases reported among the patients who underwent laparoscopic cholecystectomy.
Review of the world literature revealed an additional 32 cases (Table 1). Among these, 6 patients had acute cholecystitis, 3 had biliary colics, 1 had empyema, 3 had cholangitis, and 19 had chronic cholecystitis. In one of the reports, laparoscopic cholecystectomy was carried out in a patient who had previous abdominal surgery, while in another report laparoscopic appendicectomy was carried out in addition to cholecystectomy.14 Choledocholithiasis was reported in 4 patients, and endoscopic retrograde cholangiopancreaticography was performed in these 3 patients.2,3,15 Although technically more demanding, preoperative cholangiography and ERCP can be performed when clinically indicated. The latter can be performed in the standard fashion except for the initial placement of the patient in the right lateral decubitus position and the orientation of the sphincterotomy into the 1:00 clock position.2,3 Successful laparoscopic exploration of the common bile duct for choledocholithiais in a patient with situs inversus totalis has been reported recently.16 No major complications were reported, and with the exception of patients who initially presented with cholangitis or empyema, almost all patients left the hospital within 48 hours after surgery and did not require any specific postoperative care. To the best of our knowledge, no conversions to open surgery have been reported. We believe that this is attributable to the fact that extra precaution is taken while carrying out laproscopic cholecystectomy in this challenging situation; moreover, authors tend to report the successful cases. The logical assumption is that the rate of conversion to open cholecystectomy in SI should be higher than in patients with normally located gallbladders.
CONCLUSION
Laparoscopic cholecystectomy is the treatment of choice for symptomatic cholelithiasis. This approach should be the same for patients with situs inversus. Change in anatomical disposition of organs not only influences the localization of symptoms and signs arising from a diseased organ but also imposes special demands on the diagnostic and surgical skills of the surgeon. Technical difficulties for a right-handed surgeon include crossing of the hands and visuomotor adjustment of skills leading to additional time in skeletonizing Calot's triangle. However, laparoscopic cholecystectomy can be carried out safely in this group of patients by an experienced laparoscopic surgeon, especially if the surgeon is left-handed.
References:
- 1. Crosher RF, Harnarayan P, Bremner DN. Laparoscopic cholecystectomy in situs inversus totalis. J R Coll Surg Edinb. 1996; 41 (3): 183–184 [PubMed] [Google Scholar]
- 2. Lipschutz JH, Canal DF, Hawes RH, Ruffolo TA, Besold MA, Lehman GA. Laparoscopic cholecystectomy and ERCP with sphincterotomy in an elderly patient with situs inversus. Am J Gastroeneterol. 1992; 87 (2): 218–200 [PubMed] [Google Scholar]
- 3. Takei HT, Maxwell JG, Clancy TV, Tinsley EA. Laparoscopic cholecystectomy in situs inversus totalis. J Laparoendosc Surg. 1992; 2 (4): 171–176 [DOI] [PubMed] [Google Scholar]
- 4. Malatani TS. Laparoscopic cholecystectomy in situs inversus totalis: A case report and review of literature. Ann Saudi Med. 1996; 16: 458–459 [DOI] [PubMed] [Google Scholar]
- 5. Campos L, Sipes E. Laparoscopic cholecystectomy in a 39 year old female with situs inversus. J Laparoendosc Surg. 1991; 1 (2): 123–125 [DOI] [PubMed] [Google Scholar]
- 6. Sato M, Watanabe Y, Iseki S, et al. Hepatolithiasis with situs inversus. First case report. Surgery. 1996; 119: 598–560 [DOI] [PubMed] [Google Scholar]
- 7. Yaghan RJ, Gharaibeh KI, Hammori S. Feasibility of laparoscopic cholecystectomy in situs inversus. J Laparoendosc Adv Surg Tech A. 2001; 11 (4): 233–237 [DOI] [PubMed] [Google Scholar]
- 8. Oms LM, Badia JM. Laparoscopy Cholecystectomy in situs inversus totalis: The importance of being left handed. Surg Endosc. 2003; 17 (11): 1859–1861 [DOI] [PubMed] [Google Scholar]
- 9. Jesudason SR, Vyas FL, Jesudason MR, Govil S, Muthusami JC. Laparoscopic cholecystectomy in a patient with situs inversus. Indian J Gastroenereol. 2004; 23 (2): 79–80 [PubMed] [Google Scholar]
- 10. McKay D, Blake G. Laparoscopic cholecystectomy in situs inversus totalis: a case report. BMC Surg. 2005; 5 (1): 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Watson CJE, Rasmussen A, Jameison NV, et al. Liver transplantation in patients with situs inversus. Br J Surg. 1995; 82: 242–245 [DOI] [PubMed] [Google Scholar]
- 12. Chandraraj S. Observation on some additional abnormalities in situs inversus viscerum. J Anat. 1976; 122: 377–388 [PMC free article] [PubMed] [Google Scholar]
- 13. Torretta A, Zeri KP, Mascagni D, et al. Traditional cholecystectomy in a patient with situs inversus partialis. G Chir. 1999; 20: 293–295 [PubMed] [Google Scholar]
- 14. Polychronidis A, Karayiannakis A, Botaitis S, Perente S, Simopoulos C. Laparoscopic cholecystectomy in a patient with situs inversus totalis and previous abdominal surgery. Surg Endosc. 2002; 16 (7): 1110 Epub 2002 Apr 9 [DOI] [PubMed] [Google Scholar]
- 15. Mc Dermott JP, Caushaj PF. ERCP and laparoscopic cholecystectomy for cholangitis in a 66 year old male with situs inversus. Surg Endosc. 1994; 8 (10): 1227–1229 [DOI] [PubMed] [Google Scholar]
- 16. Kang SB, Han HS. Laparoscopic exploration of the common bile duct in a patient with Situs Inversus Totalis. J Laparoendosc Adv Surg Tech A. 2004; 14 (2): 103–106 [DOI] [PubMed] [Google Scholar]
- 17. Donthi R, Thomas DJ, Sanders D, Schmidt SP. Report of laparoscopic cholecystectomy in two patients with left sided gall bladders. JSLS. 2001; 5 (1): 53–56 [PMC free article] [PubMed] [Google Scholar]
- 18. Nursal TZ, Baykal A, Iret D, Aran O. Laparoscopic cholecystectomy in a patient with situs inversus totalis. J Laproendosc Adv Surg Tech A. 2001; 11 (4): 239–241 [DOI] [PubMed] [Google Scholar]
- 19. Singh K, Dhir A. Laparoscopic cholecystectomy in situs Inversus totalis: a case report. Surg Technol Int. 2002; 10: 107–108 [PubMed] [Google Scholar]
- 20. Demetriades H, Botsios D, Dervenis C, Evagelou J, Agelopoulos S, Dadoukis J. Laparoscopic cholecystectomy in two patients with symptomatic cholelithiasis and situs inversus totalis. Dig Surg. 1999; 16 (6): 519–521 [DOI] [PubMed] [Google Scholar]
- 21. Habib Z, Shanafey S, Arvdsson S. Laparoscopic cholecystectomy in situs viscerum inversus totalis. Minnerva Chir. 1997; 52: 271–275 [DOI] [PubMed] [Google Scholar]
- 22. D’Agata A, Boncompagni G. [Video laparoscopic cholecystectomy in situ viscerum inversus totalis.] Minnerva Chir. 1997; 52 (3): 1103–1108 Italian [PubMed] [Google Scholar]
- 23. Elhomsy G, Matta W, Varaei K, Garcet L, Rahmani M. [The millepede and the surgeon: A propos of laparoscopic cholecystectomy in a case of situs inversus or autonomic gesture constricted by reason.] J Chir. 1996; 133 (1): 43 French [PubMed] [Google Scholar]
- 24. Schiffino L, Mouro J, Levard H, Dubois F. Cholecystectomy via laparoscopy in situs inversus totalis. A case report and review of the literature. Minerva Chir. 1993; 48 (18): 1019–1023 [PubMed] [Google Scholar]
- 25. Huang SM, Chau GY, Lui WY. Laparoscopic cholecystectomy for cholelithiasis in a patient with situs inversus totalis. Endoscopy. 1992; 24 (9): 802–803 [DOI] [PubMed] [Google Scholar]
- 26. Drover JW, Nguyen KT, Pace RF. Laparoscopic cholecystectomy in a patient with situs inversus viscerum: a case report. Can J Surg. 1992; 35 (1): 65–66 [PubMed] [Google Scholar]
- 27. Goh P, Tekant Y, Shang NS, Ngoi SS. Laparoscopic cholecystectomy in a patient with empyema of the gall bladder and situs inversus. Endoscopy. 1992; 24 (9): 799–800 [DOI] [PubMed] [Google Scholar]
- 28. Al Jumaily M, Hoche F. Laparoscopic cholecystectomy in situs invesrus totalis: is it safe? J Laparoendosc Adv Surg Tech A. 2001; 11 (4): 229–231 [DOI] [PubMed] [Google Scholar]
- 29. Wong J, Tang CN, Chau CH, Luk YW, Li MK. Laparoscopic cholecystectomy and exploration of the common bile in a patient with situs inversus. Surg Endosc. 2001; 15 (2): 218. [DOI] [PubMed] [Google Scholar]
- 30. Trongue A, Monestes J, Trongue G, Genna A. Abdominal situs inversus; report of a case. Acta Gastroenterol Latinoam. 2002; 32: 43–45 [PubMed] [Google Scholar]
- 31. Docimo G, Manzi F, Maione L, et al. A case report: Laparoscopic cholecystectomy in situs Viscerum Inversus. Hepatogastroenterology. 2004; 51 (58): 958–960 [PubMed] [Google Scholar]
- 32. Pitiakoudis M, Tsaroucha AK, Katotomichelakis M, Polychronidis A, Simopoulos C. Laparoscopic cholecystectomy in a patient with situs inversus using ultrasonically activated coagulating scissors. Report of a case and review of the literature. Acta Chir Belg. 2005; 105 (1): 114–117 [PubMed] [Google Scholar]