Abstract
Objective:
We assessed the learning curve for laparoscopic supracervical hysterectomy.
Methods:
This was a prospective cohort study. We analyzed the first 60 consecutive laparoscopic supracervical hysterectomy procedures performed by a team of 2 gynecological laparoscopic surgeons between May 2001 and July 2006 to examine whether a learning curve exists as defined by a decrease in operating time and complications as the sequence increased. Based on previous reports, we defined the first 30 laparoscopic supracervical hysterectomies as “early” cases and the subsequent cases as “late” cases.
Results:
The mean operating time for laparoscopic supracervical hysterectomy was significantly reduced from 166 minutes to 142.3 minutes (P≤0.05) between the early and the late cases. The mean first postoperative day drop in hemoglobin between the early and the late cases was from 2.4gm/dL to 2.0gm/dL (P=0.08). Two complications occurred in the series: one delayed bowel injury in the early cases and one conversion to laparotomy due to a cystotomy in the late cases. No difference existed between the early and the late patients regarding age, parity, body mass index, uterine weight, previous abdominal surgery, or hospital stay. There was an overall linear correlation between the operating time and uterine weight (R=0.384).
Conclusion:
There is a learning curve for laparoscopic supracervical hysterectomy. After gaining experience in performing 30 cases, the operating time is significantly reduced. The operation can be performed safely during the learning period.
Keywords: Laparoscopic hysterectomy, Supracervical, Learning curve
INTRODUCTION
Laparoscopic supracervical hysterectomy (LSH) has been shown to be a minimally invasive alternative to all methods of total hysterectomy because it is associated with low operative morbidity and a rapid postoperative recovery.1 LSH has received more widespread acceptance in the United States in recent years as the gynecologic surgeons gain more experience in advanced laparoscopic surgery and as the electric laparoscopic morcellators become more readily available and cost effective.
As trainees and preceptors continue to learn and adopt this procedure, it is prudent to ask whether a number of procedures are necessary to achieve competence in performing LSH. This issue has previously been investigated for laparoscopic hysterectomy and laparoscopic-assisted vaginal hysterectomy. It has been established that there is a learning curve for total laparoscopic hysterectomy (TLH) and laparoscopic-assisted vaginal hysterectomy (LAVH).2–9 The data on the learning curve for LSH, however, are scarce in the medical literature. In fact, we are not aware of any reports that specifically investigate the learning curve for LSH. The surgical techniques of LSH are quite different from those for TLH and LAVH, and an adequate assessment of the learning curve for LSH cannot be done based on already published data on other methods of laparoscopic hysterectomy. Our objective was to study the learning curve for LSH at our institution as defined by diminishing operating time and perioperative complications as experience was gained.
METHODS
This was a prospective cohort study. Between May 2001 and July 2006, a team of 2 experienced gynecological laparoscopic surgeons performed their first 60 consecutive cases of LSH for benign gynecologic disease—no concomitant procedures were performed and all LSH cases performed during this time period were included.
The surgeons were proficient in performing LAVH. They were not fellowship trained and had no prior experience with LSH or TLH. The surgeons later added TLH to their surgical armamentarium. The surgical team and the operating room staff had more than 10 years of experience with advanced gynecologic laparoscopy and instrumentation. Our objective was to evaluate factors considered likely to be associated with proficiency in LSH. The data concerning peri- and postoperative surgical information and complications were collected during the patients' hospital stay and postoperative visits. Complications were defined as intraoperative blood loss requiring transfusion; bladder, bowel, and ureteral injury; unintended conversion to laparotomy, postoperative fever, pelvic infection, delayed visceral injury, fistula formation, and thromboembolic events. There were no exclusion criteria. The cases were performed at a university-affiliated teaching hospital.
All patients had normal cervical cytology and normal endometrial histology (if indicated) before surgery. Preoperative counseling emphasized a need for continued cervical screening and a possibility of cyclical bleeding in the future. The surgical technique of LSH is as previously described and remained consistent throughout the series.10,11 The patient is placed in the dorsal lithotomy position. The bladder is catheterized and a disposable uterine manipulator (Conmed, Billerica, MA, USA) is placed. Intravenous antibiotic prophylaxis is administered before the case. Pneumoperitoneum with a pressure of 15mm Hg is established via the Veres needle through the umbilicus. A 10-mm umbilical port followed by two 5-mm lower quadrant ports, lateral to the inferior epigastric arteries, are inserted.
The upper uterine pedicles are coagulated and transected by using a 5-mm bipolar device (Gyrus Medical, Minneapolis, MN, USA). The round ligaments are coagulated and transected bilaterally, and the anterior leaf of the broad ligament is dissected. A bladder flap is created, and the parametria are skeletanized to expose the uterine arteries. The uterine pedicles are then secured by using the bipolar device. The amputation of the uterine corpus from the cervix is initiated using a Harmonic scalpel hook (Ethicon Endo-Surgery, Cincinnati, OH, USA). Following hemostatsis of the cervical stump, uterine morcellation is carried out through a 12-mm suprapubic port with an electric morcellator (Gynecare, Cincinnati, OH, USA).
Following the format of previously published reports on the learning curve for laparoscopic hysterectomy, we defined the first 30 cases of LSH in our series as the “early” cases and the subsequent cases as the “late” cases. We set out to compare the measurable operative outcomes between the early and the late groups to see whether they would point toward a learning curve for the procedure.
The main outcome measure was the length of operating time in minutes. Operating time was defined as the length of time from first skin incision to closure of the last incision. The secondary outcome measure was perioperative complications and morbidity. The research protocol was reviewed and approved by the Institutional Review Board.
We assessed the normality of the data by using a histogram and the Kolmogorov-Smirnov test. We used the Student t test for continuous variables and chi-square test and Fisher's exact test for categorical variables as appropriate. We assessed the linear relationship between operating time and uterine weight by evaluating a scatter plot and using Pearson's correlation coefficient. A 2-sided P value of <0.05 was considered statistically significant. Data analysis was performed using SPSS version 11.0 for Windows (SPSS Inc., Chicago, USA).
RESULTS
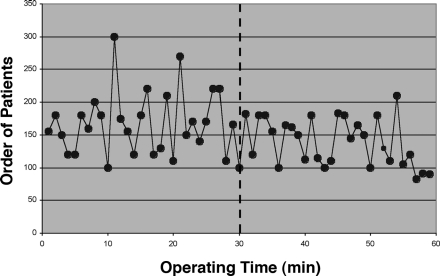
Laparoscopic removal of the uterus was accomplished in 59 patients, and all were discharged home within a 23-hour observation period. Figure 1 illustrates the distribution of operating time with increasing experience. The mean operating time for LSH was significantly reduced from 166 minutes to 142.3 minutes (P=0.02) between the early and the late cases.
Figure 1.
Learning curve according to operating time between the early and late cases.
There were 2 complications in the series; one took place in the early cases and the other took place at the onset of the late cases. The first complication occurred in case number 11. The patient had undergone an LSH for a symptomatic fibroid uterus. She presented to the emergency room on postoperative day 3 with abdominal pain, nausea, low-grade fever, and leukocytosis. Her intraoperative and postoperative events had been uneventful to this point. She underwent an exploratory laparotomy and was found to have a delayed thermal injury to the sigmoid colon, which required a segmental resection and colostomy. She recovered well postoperatively.
The second complication occurred in case number 31 and was a conversion to laparotomy due to incidental cystotomy. The patient had 2 prior Cesarean deliveries and underwent an LSH for menorrhagia. Incidental cystotomy was encountered during sharp bladder dissection. A decision was made to convert the case to laparotomy for cystotomy repair. The cystotomy was repaired in 2 layers by using delayed absorbable sutures. The supracervical hysterectomy was completed via laparotomy. The patient was discharged on postoperative day 3 with an indwelling transurethral catheter. The catheter was discontinued after a normal retrograde cystogram was obtained on postoperative day 7. The patient remains asymptomatic.
The mean first postoperative day hemoglobin drop was from 2.4gm/dL to 2.0gm/dL (P=0.08) between the early and late cases. The uterine weight ranged from 24 grams to 480 grams (mean, 143). There was no difference between the early and the late patients with regard to age, body mass index, parity, previous abdominal surgery, uterine weight, hospital stay (Table 1).
Table 1.
Patient Demographics and Operating Parameters*
| Characteristic | Early Group (n=30) | Late Group (n=30) | P |
|---|---|---|---|
| Age (years) | 42.0±6.1 | 43.3±4.9 | 0.35 |
| Body mass index | 29.3±6.8 | 28.2±5.1 | 0.49 |
| Parity, mean (SEM)† | 1.6 (0.2) | 2.1 (0.2) | 0.06 |
| Previous abdominal surgery, n (%) | 12 (40.0) | 10 (34.5) | 0.79 |
| Operating time (minutes) | 166.0±48.3 | 142.3±35.4 | 0.02 |
| Uterine weight (g) | 132.8±99.3 | 154.6±70.3 | 0.34 |
| Hemoglobin drop (g/dL)‡ | 2.4±0.7 | 2.0±0.9 | 0.08 |
| Hospital stay (hours) | 23.6±2.2 | 23.3±1.5 | 0.56 |
| Complications, n (%) | 1 (3.3) | 1 (3.3) | 1.00 |
Data are presented as mean ± standard deviation unless otherwise indicated. The case with conversion to laparotomy was excluded from analysis for all characteristics except complications.
SEM=standard error of the mean.
Difference between preoperative and first postoperative day hemoglobin.
Dysfunctional uterine bleeding and uterine fibroids comprised 83% and 77% of primary indications for surgery, respectively (Table 2). As shown in Table 3, an overall linear correlation existed between the operating time and uterine weight (R=0.384, P=0.003). A linear correlation existed between the operating time and the uterine weight in the early cases (R=0.690, P<0.001), but not in the late group (R=0.063, P=0.75).
Table 2.
Primary Indication for Hysterectomy
| Indication | Early Group (n=30)* | Late Group (n=30)* | P |
|---|---|---|---|
| Endometriosis | 1 (3.3) | 2 (6.7) | 1.00 |
| DUB | 12 (40.0) | 7 (23.3) | 0.27 |
| Uterine fibroids | 13 (43.3) | 16 (53.3) | 0.61 |
| Chronic pelvic pain | 2 (6.7) | 0 (0) | 0.49 |
| Adenomyosis | 1 (3.3) | 4 (13.3) | 0.35 |
| Dysmenorrhea | 1 (3.3) | 1 (3.3) | 1.00 |
Data are presented as n (%).
†DUB=dysfunctional uterine bleeding.
Table 3.
Correlation Between Operating Time and Uterine Weight
| Group | Correlation Coefficient (R) | P |
|---|---|---|
| Overall | 0.384 | 0.003 |
| Early group | 0.690 | < 0.001 |
| Late group | 0.063 | 0.750 |
DISCUSSION
Any discussion of the learning curve of a surgical procedure should involve identifying measurable outcomes that might signify some form of improvement.2 Reduction in operating time and perioperative complications are the 2 factors most often quoted in the medical literature.3
The learning curve for TLH and LAVH has previously been investigated. Makinen et al4 reported on morbidity of 10,110 hysterectomies by type of approach. They concluded that surgeons who had performed more than 30 cases of laparoscopic hysterectomy (as described by Garry and Reich, 1993) had a significantly lower rate of intraoperative complications. Altgassen et al3 analyzed 929 cases of LAVH performed by 33 surgeons. Their conclusion was that a learning experience of 30 LAVH cases was necessary to reach a low level of complications. Based on these reports, Vaisbuch et al5 also chose a cutoff of 30 procedures in their retrospective study of 167 women, who had laparoscopic hysterectomies (73 had LAVH and 15 had LSH), to assess the learning curve of the procedure.
Surprisingly, there is a paucity of data in the medical literature regarding the learning curve for LSH. We are aware of only one study that commented on the learning curve of LSH. In their retrospective analysis of perioperative complications in 1,706 consecutive cases of LSH, Bojahr et al1 showed that it took 120 operations to reduce the operation time to less than 100 minutes. They did not seem to offer a realistic cutoff point necessary to achieve proficiency and competence. To maintain consistency in the literature, we extrapolated from the previously published data on the learning curve for laparoscopic hysterectomy and defined the first 30 cases of LSH in our series as the early cases and the subsequent cases as the late cases. We set out to investigate whether the measurable operative outcomes between the groups would point toward a learning curve for the procedure.
Our analysis showed a significant reduction in the operating time between the early and the late cases. This finding reflects that there is a learning curve for LSH as defined by a reduction in the operating time after performing 30 cases; this is consistent with the previously published reports on the learning curve for laparoscopic hysterectomy.3–5
As expected, there was an overall correlation between the operating time and uterine weight. This probably reflects the morcellation time, as there is more tissue to be extracted when the uterus is enlarged. In addition, the degree of difficulty of LSH and hence the operating time might increase in correlation with uterine size if exposure to the vascular pedicles is compromised as a result. For example, the dissection and coagulation of the uterine artery and the upper uterine pedicles are more challenging and time consuming in an enlarged uterus. Another factor crucial to determining the time needed to complete the procedure is the amputation of the uterine corpus from the cervical body, especially in an enlarged uterus because exposure of the cervico-uterine junction is reduced.
It is worth noting that our findings did not show a correlation between operating time and uterine weight in the late cases. Because the uterine weight was similar between the early and late cases, a probable explanation for such a finding might be that the surgeons became more proficient in morcellating the uterus; a presumption that would also support the notion of a learning curve with increasing experience. There was a decreasing trend in blood loss after 30 cases, but the difference was not significant.
Operating room setup time, a concerted effort by the operating room staff, and the availability of laparoscopic instruments are pivotal to a timely completion of a laparoscopic case. We eliminated the impact of the operating room setup time by choosing the incision time as the starting point. The operating room staff was well experienced with instrumentation of gynecologic laparoscopic cases, such as LAVH, and received brief training by the manufacturer as to how to set up the uterine morcellator. We do not think that setting up the morcellator had a tangible impact on the operating time. The medical records did not indicate any laps in operating time due to instrument malfunction or unavailability.
In this study, 2 complications were recorded, one during the early cases and the other during the late cases. This would translate to an overall complication rate of 3.3%. Others have shown a drop in the perioperative complications of laparoscopic hysterectomy as the learning curve is achieved.1,4,7,9 Our findings do not support the notion that perioperative complications diminish as experience is accrued. This is in a large part due to the small number of complications encountered in this study. For example, 5 complications in the early cases and none in the late cases would have been needed to demonstrate a statistically significant trend for diminishing complications. In the literature, the reported rate of complications for LSH is between zero and 4.35%.1 A 3.3% complication rate in our series compares favorably with the published reports, and shows that LSH can be safely performed in skilled hands during the learning phase of the procedure.
One of the limitations of the current study is that it only reflects the learning experience of 2 surgeons at our institution. Their experience may not be reproducible and validated by surgeons at other institutions. More studies need to be conducted on the learning curve for LSH because the published reports are scarce.
CONCLUSION
This study demonstrates that there is a learning curve for LSH as defined by the reduction in operating time with experience. Experience in performing 30 cases of LSH may be needed before one achieves proficiency. The operation can be performed safely in skilled hands during the learning phase.
Contributor Information
Ali Ghomi, Department of Gynecology-Obstetrics, University at Buffalo, State University of New York, Buffalo, New York, USA..
Paul Littman, Department of Gynecology-Obstetrics, University at Buffalo, State University of New York, Buffalo, New York, USA..
Aru Prasad, Department of Gynecology-Obstetrics, University at Buffalo, State University of New York, Buffalo, New York, USA..
Jon Ivar Einarsson, Department of Obstetrics and Gynecology, Brigham and Women's Hospital, Harvard Medical School, Boston, Massachusetts, USA..
References:
- 1. Bojahr B, Raatz D, Schonleber, Abri C, Ohlinger R. Perioperative complication rate in 1706 patients after a standardized laparoscopic supracervical hysterectomy technique. J Minim Invasive Gynecol. 2006;13:183–189 [DOI] [PubMed] [Google Scholar]
- 2. Rosen DM, Cario GM, Carlton MA, et al. An assessment of the learning curve for laparoscopic and total laparoscopic hysterectomy. Gynecol Endosc. 1998;7:289–293 [Google Scholar]
- 3. Altgassen C, Michels W, Schneider A. Learning laparoscopic-assisted hysterectomy. Obstet Gynecol. 2004;104(2):308–313 [DOI] [PubMed] [Google Scholar]
- 4. Makinen J, Johansson J, Tomas C, et al. Morbidity of 10110 hysterectomies by type of approach. Human Reprod. 2001;16(7):1473–1478 [DOI] [PubMed] [Google Scholar]
- 5. Vaisbuch E, Goldchmit C, Agmon A, et al. Lparaoscopic hysterectomy versus total abdominal hysterectomy: a comparative study. Eur J Obstet Gynecol Reprod Biol. 2006;126(2):234–238 [DOI] [PubMed] [Google Scholar]
- 6. Harkki-Siren P, Sjoberg J. Evaluation and the learning curve of the first one hundred laparoscopic hysterectomies. Acta Obstet Gynecol Scand. 1995;74:638–641 [DOI] [PubMed] [Google Scholar]
- 7. Perino A, Cucinella G, Venezia R, et al. Total laparoscopic hysterectomy versus total abdominal hysterectomy: an assessment of the learning curve in a prospective randomized study. Hum Reprod. 1999;14(12):2996–2999 [DOI] [PubMed] [Google Scholar]
- 8. Leminen A. Comparison between personal learning curves for abdominal and laparoscopic hysterectomy. Acta Obstet Gynecol Scand. 2000;79:1100–1104 [PubMed] [Google Scholar]
- 9. Jones RA. Complications of laparoscopic hysterectomy: comparison of the first 250 cases with the second 250. Gynecol Endosc. 2000;9:373–378 [Google Scholar]
- 10. Donnez J, Nisolle M, Smets M, et al. Laparoscopic supracervical (subtotal) hysterectomy: a first series of 500 cases. Gynecol Endosc. 1997;6:73–76 [Google Scholar]
- 11. Lyons TL. Laparoscopic supracervical hysterectomy. Obstet Gynecol Clin North Am. 2000;27:441–450 [DOI] [PubMed] [Google Scholar]