Abstract
Objective:
We evaluated our experience with laparoscopic L5-S1 anterior lumbar interbody fusion (ALIF).
Methods:
This represents a retrospective analysis of consecutive patients who underwent L5-S1 laparoscopic ALIF between February 1998 and August 2003.
Results:
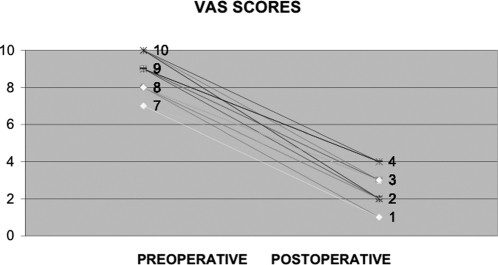
Twenty-eight patients underwent L5-S1 LAIF (15 males and 13 females). The mean age was 43 years (range, 26 to 67). Mean operative time was 225 minutes (range, 137 to 309 minutes). No conversions to an open procedure were necessary. Twenty-four (85.7%) patients underwent successful bilateral cage placement. Four patients (14.3%) in whom only a single cage could be placed underwent supplementary posterior pedicle screw placement. Mean length of stay (LOS) was 4.1 days (range, 2 to 15). Two patients underwent reoperation subacutely secondary to symptomatic lateral displacement of the cage. One patient developed radiculopathy 6 months postoperatively and required reoperation. One patient developed a small bowel obstruction secondary to adhesions to the cage requiring laparoscopic reoperation. Fusion was achieved in all patients. Visual analogue scale scores for back pain were significantly improved from 8.6±0.8 to 2.8±0.8 (P<0.0001) at 1 year.
Conclusion:
L5-S1 LAIF is feasible and safe with all the advantages of minimally invasive surgery. Fusion rates and pain improvement were comparable to those with an open repair.
Keywords: Minimally invasive surgery, Anterior lumbar interbody fusion, Cages, rhBMP-2
INTRODUCTION
Anterior lumbar interbody fusion (ALIF) has been performed for a variety of conditions including spondylolis-thesis, symptomatic degenerative disc disease and as a salvage for failed posterior spinal fusion.1,2 Advantages of the anterior versus posterior approach include avoidance of paraspinal muscle trauma, placement of a larger inter-body cage and a shorter hospital stay.3 Freebody et al4 popularized ALIF in 1963 subsequent to the initial description by Carpener.5 Over the next 4 decades, several anterior transperitoneal and retroperitoneal approaches to the lumbosacral spine were described.6,7
Minimally invasive techniques to ALIF began in 1991 as Obenchain8 first described a noninstrumented L5-S1 discectomy. Zucherman et al9 in 1995 reported the first series of laparoscopic ALIF with threaded interbody metallic cages. Over the next several years, more reports of laparoscopic ALIF surfaced.6,10–12 McAfee et al13 demonstrated the feasibility and safety of endoscopic thoracolumbar fusion in a prospective multicenter study.
Technology has rapidly advanced with respect to inter-body devices from bone dowel ALIF to metal threaded BAK (Spinetech) and RAY (Surgical Dynamics) cages to the lordotic LT cage (Medtronic).14,15 Arthrodesis materials have also progressed from autogenous bone graft to the use of rhBMP-2 thus improving fusion rates.16
We analyzed a series of 28 patients who underwent laparoscopic L5-S1 anterior interbody fusion. Many of the above advances were incorporated during this study.
METHODS
A retrospective review of patients who underwent laparoscopic L5-S1 anterior interbody fusion by a laparoscopic general surgeon (CTF) and orthopedic surgeon (FMP) over a 5-year period (1998 to 2003) was performed. Patients with chronic mechanical lower back pain secondary to degenerative disc disease, spondylolisthesis, or post-laminectomy syndromes were candidates for ALIF. Patients had previously failed at least 6 months of appropriate nonoperative treatment. Patients underwent magnetic resonance imaging (MRI), provocative discography, or both, preoperatively to identify the symptomatic disc level.
Since cages were placed, cefazolin (1 g to 2 g IV) was given with the induction of anesthesia.
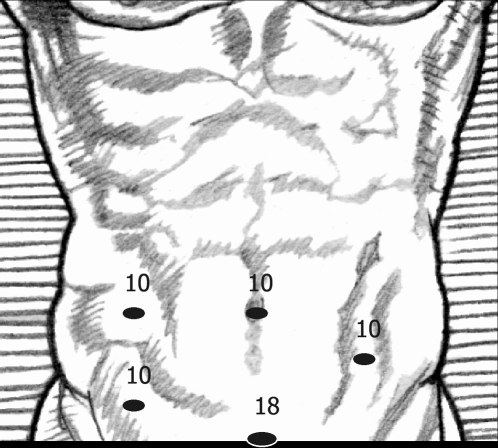
Our technique for L5-S1 LAIF is herein briefly described. An infraumbilical curvilinear incision was used to place a Hasson trocar followed by pneumoperitoneum maintained at 15 mm Hg. Three additional trocars 10 cm to 11 mm were introduced under direct view; one in the right side ipsilateral to the umbilicus, one in the right lower quadrant; and one in the left lower quadrant. The 18-mm trocar, which is the main working port for the spinal surgeon, was placed in the suprapubic midline region (Figure 1). The patient was then placed in a steep Trendelenburg position to facilitate cephalad retraction of the viscera. The sigmoid colon was retracted to the left by using an inflatable balloon retractor (Soft wand retractor, ACMI, San Jose, CA) introduced through the left lateral port. Hook electrocautery was then inserted through the right lower quadrant port, and the peritoneum at the root of the recto-sigmoid mesocolon was opened below the bifurcation of the aorta. Using blunt dissection, the medial sacral artery and vein were identified and ligated with placement of vascular clips. At this point, the L5-S1 intervertebral disc was exposed, and the right and left iliac veins were mobilized by using a palpation probe. Exposure to the L5-S1 was maintained with the inflatable balloon retractor, the sigmoid mesocolon was retracted to the left to give adequate exposure to this area and the orthopedic portion of the procedure was initiated.
Figure 1.
Trocar placement.
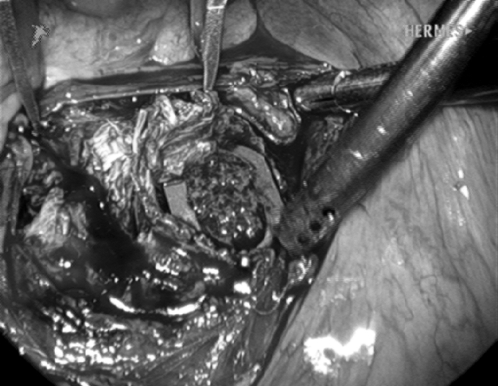
A K-wire was then percutaneously passed from a midline suprapubic position into the diseased disc space. Fluoroscopy confirmed placement into the L5-S1 disc space and allowed correct angulation of the suprapubic 18-mm working trocar (Figure 1). The annulus over the disc space was divided, and the disc evacuated with a trephine and rongeurs until bleeding cancellous bone was exposed. A dilator and a distraction plug were driven into the interspace to restore the native disc space height and distract the vertebral bodies before the disc reaming and cage placement. BAK (Spinetech, Minneapolis, MN) or RAY (Surgical Dynamics, Norwalk, CT) cages were used until May 2001; thereafter, lordotic LT (Medtronic, Minneapolis, MN) cages were used (Figure 2). Iliac bone graft was used to fill the cages until the end of 2001; thereafter, recombinant human bone morphogenetic protein-2 (rhBMP-2) (Infuse, Medtronic, Minneapolis, MN) was used. The posterior peritoneum was left open initially in this series but was reapproximated after a case of small bowel adhesion to the cage.
Figure 2.
Cage placement.
At the completion of the arthrodesis, the fascial defects at the trocar sites were closed using a fascial closer. In some cases, percutaneous posterior pedicle screw placement was performed with the Sextant (Medtronic, Minneapolis, MN) system.17
A clear liquid diet was begun with passage of flatus and advanced to a regular diet as tolerated. The patient was placed on patient-controlled analgesia postoperatively and weaned to oral narcotic analgesics. Patient was discharged when they had an adequate oral intake and pain was controlled on oral analgesics alone. Follow-up consisted of clinic appointments at 1 week, 1 month, 3 months, and yearly thereafter. Visual analogue scale scores1–10 for spinal pain were recorded preoperatively and at 1 year postoperatively. Flexion-extension radio-graphs were used to assess fusion rates 1-year postoperatively. The fusion was deemed healed if there was absence of motion across the operated level and the implant remained stable without surrounding radiolucencies or evidence of bone bridging the interspace. Diagnostic studies such as MRI were ordered during follow-up if a patient developed new symptoms. Data are reported as mean with a range or standard deviation or both. Statistics were done using Graphpad Instat (San Diego, CA).
RESULTS
L5-S1 laparoscopic anterior interbody fusion was undertaken in 28 patients between 1998 and 2003. Five patients had undergone prior discectomy (n=3), laminectomy (n=1), or fusion (n=1). The mean patient age was 43 (range, 26 to 67). Fifteen (54%) patients were male and 13 (46%) were female. The presenting symptoms were back pain in all patients, sciatica in 5 patients (18%), and buttock pain in 1 patient.
Conversion to an open procedure was not required in any patient. The mean duration of surgery was 225±47 minutes (range, 137 to 309). The average operative time was significantly longer (P<0.008, Mann-Whitney) in the first 19 patients of the series who had graft from the iliac bone utilized (241±42 minutes) versus the last 9 patients in whom rhBMP-2 was used (190±39 minutes).
Twenty-four patients (86%) underwent successful bilateral cage placement. Six of these patients underwent additional posterior screw placement. Four patients (14%) could only undergo unilateral cage placement secondary to either difficulties achieving adequate purchase with 2 cages or vessel encroachment limiting access for bilateral cage placement. The first 3 of these patients underwent subsequent posterior screw fixation being discharged on day 15, 5, and 4, while the last underwent concomitant posterior screw fixation and was discharged on day 3.
Intraoperative complications included 2 bladder injuries sustained secondary to K-wire guide pin localization. These were both recognized intraoperatively and repaired primarily. Urinary catheters were maintained until postoperative day 4 at which time a negative cystogram allowed removal. No major vascular injuries occurred, and estimated blood loss was 145±136 mL.
Three patients (10%) had prolonged postoperative ileus that delayed discharge until day 15 (patient also had a delayed secondary procedure for posterior instrumentation), 6, and 5. The length of stay (LOS) for all patients was 4.1±2.4 (range, 2 to 15). Mean LOS was 5.2 days in the first 19 patients versus 3.6±1 days in the last 9 (P=0.43, Mann-Whitney). No perioperative deaths occurred.
Three patients required unplanned spinal procedures. One patient developed displaced bone dowel cages with symptomatic radiculopathy one week after discharge from the hospital. This patient underwent reoperation with posterior pedicle screw instrumentation. A second patient sustained a fall while in the hospital on the third postoperative day and developed acute radiculopathy with EHL weakness. Computed tomography revealed the cages to be slightly laterally positioned extending toward the neural foramen on the symptomatic side. The patient underwent hemifacetectomy, annular excision, foraminotomy and posterior translaminar screw placement. A third patient developed buttock pain 6 months postoperatively. CT myelography revealed subarticular stenosis, and the patient underwent posterior decompression.
One patient developed a small bowel obstruction 4 months postoperatively. The small bowel was adhered to the cage, and a small bowel resection was required. This was completed in a laparoscopic fashion.
Radiographic fusion was achieved in all patients. Visual analog scores (VAS) were significantly improved from 8.6±0.8 before surgery compared with 2.8±0.8 (P<0.0001, Wilcoxon matched pairs) at 1 year following surgery (Figure 3).
Figure 3.
Visual Analogue Scale score.
DISCUSSION
Since the first report of laparoscopic anterior interbody fusion in 1991, several retrospective reviews and prospective trials have emerged.6–8,10–14,18–26 This represents a review of 28 patients who underwent laparoscopic L5-S1 ALIF. The conversion rate in this series to an open procedure was zero.
L4-L5 laparoscopic ALIF is associated with a higher morbidity rate than the open approach,19,23,26 and many authors have ceased performing L4-L5 LAIF after encountering adverse complications and high conversions rates.19,20 The junction of the left iliac vein and the vena cava often lies directly over the L4-L5 disc space making the laparoscopic approach very difficult and may lead to life-threatening vascular injury.
Laparoscopic L4-L5 ALIF was compared with a mini-retroperitoneal open technique by Zdeblick and David26 who concluded that there did not appear to be a benefit to the laparoscopic approach because they encountered a morbidity rate of 20%. They advocated laparoscopic L4-L5 ALIF only if the bifurcation of the great vessels is above the L4-L5 disc space. As a result of the above, we did not perform laparoscopic L4-L5 ALIF.
Although both senior authors (CTF and FMP) have extensive prior laparoscopic experience, this series emphasizes the learning curve associated with laparoscopic ALIF. Mean operative time decreased progressively over the course of this study from 241±42 minutes for the first 19 patients to 190±39 minutes for the last 9. The learning curve is known to be steep with laparoscopic ALIF, and we feel that operative times would likely continue to decrease as further experience is gained.
We were initially concerned that 3 patients underwent reoperation (10.7%) early in our experience. One patient had a displaced bone dowel 1 week postoperatively and required posterior fusion and screw placement. Two other patients developed radiculopathy postoperatively (3 days and 6 months) and underwent foraminotomy with hemifacetectomies to decompress the involved nerve roots and posterior instrumented fusion. All 3 of these cases occurred early in our experience reflecting errors in technique, and no cases occurred of postoperative radiculopathy in the last 20 cases. Kuslich et al14 reported that 8.7% of patients required a second operation after open BAK cage placement.
Ten patients (36%) underwent posterior screw placement to provide additional support to the ALIF. In 4 of these patients, posterior instrumentation was placed because of the inability to place 2 interbody cages secondary to vessel encroachment or inability to gain acceptable bony purchase with both cages. In the remaining 6 cases undergoing posterior stabilization, posterior pedicle instrumentation had been deemed necessary preoperatively to provide additional support to the ALIF construct. We feel that posterior pedicle screw placement in a minimally invasive fashion17 should be used liberally to achieve stability particularly in those cases of unilateral cage placement. The first 2 patients who underwent delayed screw placement had an LOS of 5 and 15 days while the last patient who underwent concomitant screw placement had an LOS of 3 days. Therefore, concomitant placement of the screws with the ALIF will likely decrease hospital stay in those cases of unilateral cage placement.
Mean LOS was 4.1 days (range, 2 to 15). One reason that LOS appears to be longer than that in some reports10,21 is that a liquid diet was not initiated until flatus occurred. Immediate postoperative advancement of the diet and quicker weaning off narcotics would likely have decreased LOS. Patients who undergo laparoscopic procedures tend to have a decreased length of postoperative ileus and length of stay compared with those who undergo an open procedure,21 but recent studies have shown no difference.26
The availability of rhBMP-2 has eliminated the need for iliac bone graft and a separate incision. A prospective study of LAIF with rhBMP-2 by Kleeman et al16 revealed a 100% fusion rate at 6 months. This was our experience as well. An additional benefit of the use of rhBMP-2 is the decreased operative time. Closure of the peritoneum over the metallic cages particularly when rhBMP-2 is used appears to be important because we did have one patient who developed a small bowel obstruction secondary to adhesive disease and required a small bowel resection.
We attribute the good results of this study to 3 factors1: patient selection,2 advanced laparoscopic experience of both the general and the spine surgeon, and3 the presence of both surgeons during the entire procedure.
CONCLUSION
Laparoscopic L5-S1 ALIF can be performed safely with low morbidity with the inherent advantages of minimally invasive surgery.
Contributor Information
Constantine T. Frantzides, Minimally Invasive Surgery Center, Department of Surgery, Evanston Northwestern Healthcare and Northwestern University, Evanston, Illinois, USA..
Tallal M. Zeni, Minimally Invasive Surgery Center, Department of Surgery, Evanston Northwestern Healthcare and Northwestern University, Evanston, Illinois, USA..
Frank M. Phillips, Department of Orthopedic Surgery, Rush University, Chicago, Illinois, USA..
Sameer Mathur, Department of Orthopedic Surgery, Rush University, Chicago, Illinois, USA..
John G. Zografakis, Advanced Laparoscopy – Surgery for Northeast Ohio Centers of Excellence, Akron, Ohio, USA..
Ronald M. Moore, Department of Surgery, Plantation Hospital, Fort Lauderdale, Florida, USA..
Luis E. Laguna, Minimally Invasive Surgery Center, Department of Surgery, Evanston Northwestern Healthcare and Northwestern University, Evanston, Illinois, USA..
References:
- 1. Blumenthal SL, Baker J, Dossett A, Selby DK. The role of anterior lumbar fusion for internal disc disruption. Spine. 1988; 13 (5): 566–569 [DOI] [PubMed] [Google Scholar]
- 2. Flynn JC, Hoque MA. Anterior fusion of the lumbar spine. End-result study with long-term follow up. J Bone Joint Surg Am. 1979; 61 (8): 1143–1150 [PubMed] [Google Scholar]
- 3. Greenough CG, Peterson MD, Hadlow S, Fraser RD. Instrumented posterolateral lumbar fusion. Results and comparison with anterior interbody fusion. Spine. 1998; 23 (4): 479–486 [DOI] [PubMed] [Google Scholar]
- 4. Freebody D, Bendall R, Taylor RD. Anterior transperitoneal lumbar fusion. J Bone Joint Surg. 1971; 53 (4): 617–627 [PubMed] [Google Scholar]
- 5. Carpener N. Spondylolisthesis Br J Surg. 1931; 19: 374 [Google Scholar]
- 6. Cloyd DW, Obenchain TG, Savin M. Transperitoneal laparoscopic approach to lumbar discectomy. Surg Laparosc Endosc. 1995; 5 (2): 85–89 [PubMed] [Google Scholar]
- 7. Hacker RJ. Comparison of interbody fusion approaches for disabling back pain. Spine. 1997; 22 (6): 660–665 [DOI] [PubMed] [Google Scholar]
- 8. Obenchain TG. Laparoscopic lumbar discectomy: case report. J Laparoendosc Surg. 1991; 1 (3): 145–149 [DOI] [PubMed] [Google Scholar]
- 9. Zucherman JF, Zdeblik TA, Bailey SA, Mahvi D, Hsu KY, Kohrs D. Instrumented laparoscopic spinal fusion: preliminary results. Spine. 1995; 20 (18): 2029–2035 [DOI] [PubMed] [Google Scholar]
- 10. Mahvi DM, Zdeblick TA. A prospective study of laparoscopic spinal fusion. Technique and operative complications. Ann Surg. 1996; 224 (1): 85–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mathews HH, Evans MT, Molligan HJ, Long BH. Laparoscopic discectomy with anterior lumbar interbody fusion. A preliminary review. Spine. 1995; 20 (16): 1797–1802 [DOI] [PubMed] [Google Scholar]
- 12. Regan JJ, Yuan H, McAfee PC. Laparoscopic fusion of the lumbar spine: minimally invasive spine surgery. A prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine. 1999; 24 (4): 402–411 [DOI] [PubMed] [Google Scholar]
- 13. McAfee PC, Regan JR, Zdeblick T, et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery. A prospective multicenter study comprising the first 100 consecutive cases. Spine. 1995; 20 (14): 1624–1632 [DOI] [PubMed] [Google Scholar]
- 14. Kuslich SD, Danielson G, Dowdle JD, Sherman J, Fredrickson B, Yuan H, Griffith SL. Four-year follow up results of lumbar spine arthrodesis using the Bagby and Kuslich lumbar fusion cage. Spine. 2000; 25 (20): 2656–2662 [DOI] [PubMed] [Google Scholar]
- 15. Zdeblick TA, Phillips FM. Interbody cage devices. Spine. 2003. 28 (15 Suppl): S2– S7 [DOI] [PubMed] [Google Scholar]
- 16. Kleeman TJ, Ahn UM, Talbot-Kleeman A. Laparoscopic anterior lumbar interbody fusion with rhBMP-2. A prospective study of clinical and radiologic outcomes. Spine. 2001; 26 (24): 2751–2856 [DOI] [PubMed] [Google Scholar]
- 17. Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine. Preliminary clinical results. J Neurosurg. 2002; 97(1 suppl): 7–12 [DOI] [PubMed] [Google Scholar]
- 18. Chung SK, Lee SH, Lim SR, et al. Comparative study of laparoscopic L5-S1 fusion versus open mini-ALIF, with a minimum 2-year follow-up. Eur Spine J. 2003; 12 (6): 613–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cowles RA, Taheri PA, Sweeney JF, Graziano GP. Efficacy of the laparoscopic approach for anterior lumbar spinal fusion. Surgery. 2000; 128 (4): 589–596 [DOI] [PubMed] [Google Scholar]
- 20. Geerdes BP, Geukers CW, van Erp WF. Laparoscopic spinal fusion of L4-L5 and L5-S1. Surg Endosc. 2001; 15 (11): 1308–1312 [DOI] [PubMed] [Google Scholar]
- 21. Kaiser MG, Haid RW, Subach BR, Miller KS, Smith CD, Rodts GE. Comparison of the mini-open versus laparoscopic approach for anterior lumbar interbody fusion: a retrospective review. Neurosurg. 2002; 51 (1): 97–103 [DOI] [PubMed] [Google Scholar]
- 22. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 28(15 suppl): S26–35, 2003 [DOI] [PubMed] [Google Scholar]
- 23. Katkouda N, Campos GM, Mavor E, Mason RJ, Hume M, Ting A. Is laparoscopic approach to lumbar spine fusion worthwhile? Am J Surg. 1999; 178 (6): 458–461 [DOI] [PubMed] [Google Scholar]
- 24. Regan JJ, Aronoff RJ, Ohnmeiss DD, Sengupta DK. Laparoscopic approach to L4-L5 for interbody fusion using BAK cages: experience in the first 58 cases. Spine. 1999; 24 (20): 2171–2174 [DOI] [PubMed] [Google Scholar]
- 25. Zdeblick TA. Laparoscopic spinal fusion. Orth Clinic North Am. 1998; 29 (4): 635–645 [DOI] [PubMed] [Google Scholar]
- 26. Zdeblick TA, David SM. A prospective comparison of surgical approach for anterior L4-L5 fusion: laparoscopic versus mini anterior lumbar interbody fusion. Spine. 2000; 25 (20): 2682–2687 [DOI] [PubMed] [Google Scholar]