Abstract
Background:
The reported advantages of the laparoscopic approach to appendectomy are shortened hospital stay, less postoperative pain, and earlier return to usual activities (work). However, a prospective, randomized, double-blind trial comparing laparoscopic appendectomy with open appendectomy in active-duty males failed to disclose a benefit of laparoscopic appendectomy with regards to postoperative pain and return to work. The aim of our study was to compare open and laparoscopic appendectomy in overweight patients.
Methods:
We conducted a prospective, randomized, double-blind study to determine whether laparoscopic appendectomy or the open procedure in overweight patients offers a significant reduction in lost workdays, postoperative pain, or operative time from. Open appendectomy in overweight patients (those with a body mass index ≥25) may be more difficult due to excessive sub-cutaneous adipose tissue. The open incision may be of considerable size, which may result in increased postoperative pain and a prolonged convalescence.
Results:
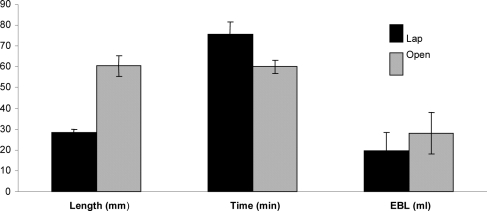
There was a statistically significant increase in operative time for laparoscopic appendectomy of 11 minutes. As expected, the aggregate incision length for open appendectomy was twice that of the laparoscopic appendectomy.
Conclusion:
The data from this prospective, randomized, double-blind study failed to demonstrate any significant reduction in lost workdays, postoperative pain, or operative time with laparoscopic appendectomy.
Keywords: Appendectomy, Body Mass Index
INTRODUCTION
With the explosion of laparoscopic surgery in the 1990s, many surgical procedures have transitioned to the laparoscopic approach. The safety and technical aspects of these approaches have been thoroughly evaluated. This is especially true for laparoscopic appendectomy.1–3 The ability to safely complete this procedure has been exhaustively evaluated, but controversy exists as to the true benefits for this approach. The proposed benefits include shorter hospital stay, lower narcotic requirements (pain), and earlier return to work. Drawbacks include higher operative costs and potentially longer operating room times. Some studies report shorter hospital stays, a reduction in postoperative pain, and earlier return to work while other studies fail to demonstrate such differences.1–5 Some authors suggest that the laparoscopic approach may be best suited for those patients who meet the criteria established by the National Heart, Lung, and Blood Institute as overweight (body mass index (BMI) >24.9); however, these studies may be limited by observer bias and certainly have a hospital stay that is at least twice that at our institution.4–6 Open appendectomy is frequently performed through a right lower quadrant incision that requires a larger skin incision, separation of more abdominal musculature, potentially resulting in more postoperative pain and a longer convalescence in this population. Anecdotal reports suggest that the laparoscopic approach may be easier to perform in obese individuals and results in less postoperative pain and shorter operative time. However, these assertions have only been reviewed by one investigator who demonstrated shorter operative times with laparoscopic appendectomy but noted longer convalescent times and less postoperative pain.4 The purpose of this randomized, prospective, blind trial was to compare laparoscopic appendectomy with traditional open appendectomy in obese patients to determine differences in postoperative pain, length of stay, postoperative complications, lost work days, operative time, and hospital cost of care.
METHODS
The protocol was reviewed and approved by the medical center's institutional review board (IRB) for human research. Prestudy analysis suggested that 52 patients would provide sufficient power to detect at least a 25% difference between groups with respect to postoperative pain, lost workdays, and hospital costs. Fifty-two consecutive over-weight patients (BMI >24.9) presenting with the clinical diagnosis of acute appendicitis were randomized to either undergo laparoscopic appendectomy or open appendectomy. All laparoscopic procedures were performed using the same technique and instruments that were previously demonstrated at our institution to be the most cost effective. These consisted of a Harmonic scalpel to divide the mesentery, Endoloop ties to secure the appendiceal stump, and an endo-catch pouch to retrieve the specimen. All wounds, laparoscopic or open, were infiltrated with bupivacaine before the start of the operative procedure and the first visual analogue pain score was taken on postoperative day number one, well after the local anesthetic had worn off. At completion of the surgery, a large sterile abdominal dressing was placed on the patient's abdomen to obscure the incisions. The patient's postoperative care was provided by members of the surgical team blinded to the surgical approach used. Patients recorded their postoperative pain daily on a visual analogue pain scale (VAS). Hospital discharge decisions were made by the team providing postoperative care based on tolerance of diet, postoperative fever curves, and postoperative pain control. All patients were seen weekly until they returned to work or their usual activity level if not employed. Visual analogue pain scales were collected at these visits and the patients self-reported on their ability to return to work. Data collected included demographics, postoperative pain medication use and pain scores, aggregate incision length, postoperative complications, length of hospital stay, operating room costs (case length and equipment costs), and lost work time, which were analyzed with a one-way analysis of variance (ANOVA). All cost data were actual cost for equipment and not hospital charges.
RESULTS
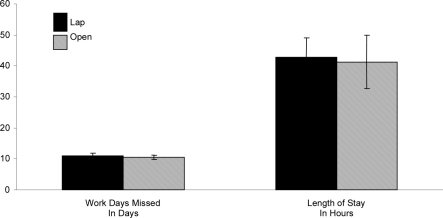
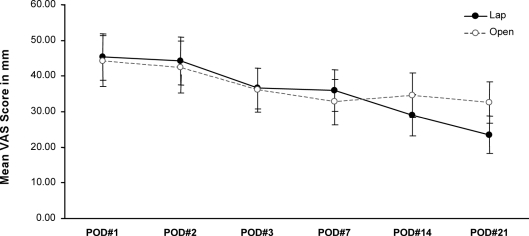
Fifty-two consecutive obese patients with a clinical diagnosis of acute appendicitis were enrolled over an 18-month time frame. Eighty-six percent of the patients enrolled were male, which reflects our military patient population, and the average age was 31 years in both groups. The average BMI for the laparoscopic cases was 30, which was not statistically different from BMI in the open cases at 28.8 (P=.799). The average number of lost workdays in both groups was 10, and there was no significant difference between the 2 groups (P=.712) (Figure 1). The hospital length of stay was equivalent at 43 hours (P=.880), and on average, it took 11 minutes longer to perform the laparoscopic appendectomy than the open counterpart (P=.015) (Figure 2). As expected, the aggregate incision length was greater in the open appendectomy group at 6cm (P<.001), but this did not translate into greater pain for those patients undergoing the open appendectomy (P=.657) (Figure 3). No significant differences were noted in postoperative pain scales, and the use of postoperative oral analgesics was equivalent (Figure 3). The material costs were significantly lower ($1200.00) for the open appendectomy approach, and this was primarily related to consumable operating room supplies. One conversion from laparoscopic to open appendectomy was necessary for technical reasons, and no wound complications occurred in any of the groups. The distribution of pathology was similar between groups with the majority of cases being acute appendicitis (Figure 4).
Figure 1.
Lost workdays.
Figure 2.
Operative time, incision length, estimated blood loss (EBL).
Figure 3.
Visual analogue pain scores.
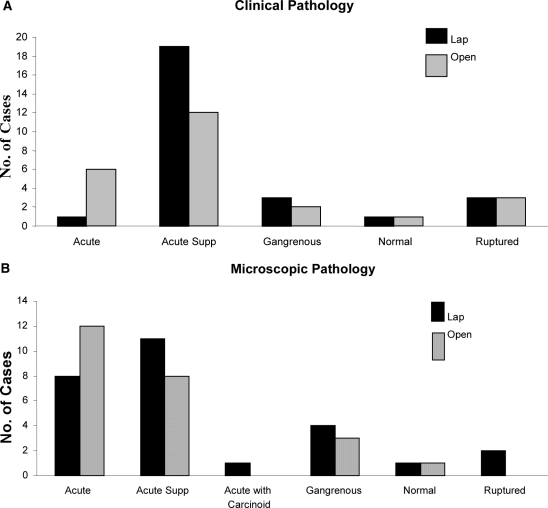
Figure 4.
Distribution of pathology (clinical and microscopic).
DISCUSSION
Our previous report on military males randomized and double-blinded to either laparoscopic or open appendectomy failed to demonstrate any significant advantage to the patients with respect to postoperative pain or lost workdays.7 They did however demonstrate an economic disadvantage of the procedure. Opinion within our department regarding overweight patients was that the laparoscopic approach was technically easier to perform (shorter operative times) and did confer a pain and lost workday advantage for the patient. The patient population used in this study comprised both active-duty military personnel and civilians entitled to care at our facility. Our data fail to confirm that assertion in this population. The length of stay reported time is nearly twice that previously reported by our group as a result of a greater number of complicated appendicitis cases in this review. On combining our previously reported pain data with the current data (same study design) with 104 patients randomized to either laparoscopic or open appendectomy, there was statistically no difference in postoperative self-reported pain; convincing us that laparoscopic appendectomy confers no patient advantage regarding postoperative pain (P=.853) (Figure 5). The economic disadvantage demonstrated for laparoscopic appendectomy may be overcome if the postoperative infectious complication rates between the operative approaches are significantly different as has been argued by previous investigators.7 Our study was not designed to evaluate postoperative complication rates between the 2 approaches, and further investigation is warranted.
Figure 5.
Combined visual analogue pain scores.
CONCLUSION
The data from this prospective randomized double-blind study failed to demonstrate any significant reduction in lost workdays, postoperative pain, or operative time from laparoscopic appendectomy in overweight patients. A statistically significant increase was noted in operative time for laparoscopic appendectomy of 11 minutes and an overall increase in hospital equipment costs of $1200.00. As expected, the aggregate incision length for open appendectomy was twice that of the laparoscopic appendectomy. In the obese patient, laparoscopic appendectomy should be reserved for those in whom the diagnosis remains in question as it is more costly to the institution and does not result in fewer lost workdays or less postoperative pain.
Contributor Information
Robert Ricca, Department of General Surgery, Naval Medical Center, Portsmouth, Virginia, USA..
James J. Schneider, Department of General Surgery, Naval Medical Center, Portsmouth, Virginia, USA..
Harpreet Brar, Department of General Surgery, Naval Medical Center, Portsmouth, Virginia, USA..
Paul A. Lucha, Jr., Division of Colon and Rectal Surgery, Naval Medical Center, Portsmouth, Virginia, USA..
References:
- 1. Hart R, Rajgopal C, Plewes A, et al. Laparoscopic versus open appendectomy: a prospective randomized trial of 81 patients. Can J Surg. 1996;39:457–462 [PMC free article] [PubMed] [Google Scholar]
- 2. Mutter D, Vix M, Bui A, et al. Laparoscopy not recommended for routine appendectomy in men: results of a prospective randomized study. Surgery. 1996;120:71–74 [DOI] [PubMed] [Google Scholar]
- 3. McCahill L, Pellegrini C, Wiggins T, Helton W. A clinical outcome and cost analysis of laparoscopic versus open appendectomy. Am J Surg. 1996;171:533–537 [DOI] [PubMed] [Google Scholar]
- 4. Enochsson L, Hellberg A, Rudberg C, et al. Laparoscopic vs open appendectomy in overweight patients. Surg Endosc. 2001;15:387–392 [DOI] [PubMed] [Google Scholar]
- 5. Ignacio R, Burke R, Spencer D, Bissell C, Dorsainvil C, Lucha P. Laparoscopic versus open appendectomy - what is the real difference? Results of a prospective randomized double blinded trial. Surg Endosc. 2004;18:334–337 [DOI] [PubMed] [Google Scholar]
- 6. Kuczmarski RJ, Carrol MD, Flegal KM, Troiano RP. Varying body mass index cut-off points to describe overweight prevalence among U.S. adults: NHANES III (1988 to 1994). Obes Res. 1997;5:542–548 [DOI] [PubMed] [Google Scholar]
- 7. Hoehne F, Ozaeta M, Sherman B, Miani P, Taylor E. Laparoscopic versus open appendectomy: is the postoperative infectious complication rate different? Am Surg 2005;71:813–815 [PubMed] [Google Scholar]