Abstract
Background and Objectives:
The safety and efficacy of female hysteroscopic sterilization using the Essure system has been well documented. Given the marked differences in the execution of hysteroscopic and laparoscopic sterilization, the objective of this study was to assess the experience of pain postprocedure between the 2. Secondary end-points included postoperative pain medication, time to return to normal activities, postprocedure bleeding, and patient satisfaction.
Methods:
Twenty cases each of laparoscopic sterilization (LS) and hysteroscopic sterilization (HS) were performed. Patients were surveyed regarding their experience of pain immediately postoperatively, 1 week, and 4 weeks post-procedure.
Results:
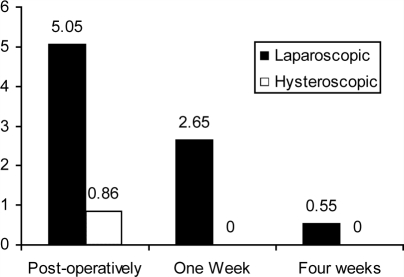
The average pain score immediately postprocedure was significantly lower among HS patients than among LS patients (t=−8.17, P<.0001). One-week post-procedure, none of the patients in the HS group reported any pain, while the average pain score among the LS patients was 2.65 (t =−9.67, P<.0001). Four weeks post-procedure, women in the HS group continued to report no pain, 35% of the LS group continued to report some pain (t=−3.04, P=.004).
Conclusions:
Hysteroscopic sterilization offers a minimally invasive, less painful, equally efficacious modality for sterilization than laparoscopic sterilization and should be available to all women seeking permanent birth control.
Keywords: Hysteroscopic sterilization, Laparoscopic sterilization, Essure, Female sterilization, Permanent birth control
INTRODUCTION
The safety and efficacy of female hysteroscopic sterilization using the Essure system (Conceptus, Inc., Mountain View, CA) has been well documented, and this system is the only hysteroscopic method of sterilization approved for use by the FDA.1–4 There are marked differences in the execution of hysteroscopic and laparoscopic sterilization. Whereas laparoscopic sterilization is performed with the administration of general anesthesia in the majority of cases, hysteroscopic sterilization can be performed with minimal sedation, as the procedure is less invasive and involves no incisions. The methods also differ in that laparoscopic sterilization offers immediate contraception. The Essure method requires the patient to use a back-up method of contraception for 3 months postprocedure and provides confirmation of sterility with a follow-up hysterosalpingogram (HSG). Given these distinctions between the two, it is possible that patient experiences differ between the methods. Fraser5 reported that pain after tubal ligation is a significant problem and greatly affects a patient's ability to return to normal activities. Reports of pain after laparoscopic tubal ligation and hysteroscopic procedures have reported greater pain scores following laparoscopy. Duffy6 surveyed women who had undergone either hysteroscopic sterilization or laparoscopic sterilization. The data demonstrated an advantage of the hysteroscopic method over the laparoscopic approach.
The objective of this study was to more thoroughly assess the experience of pain postprocedure. Patients were surveyed regarding their experience of pain immediately postoperatively, 1 week, and 4 weeks postprocedure. Secondary end-points included, postoperative recovery time, postoperative pain medication, time to return to normal activities, postprocedure bleeding, and patient satisfaction at 3 months.
METHODS
Study participants were a sample of convenience recruited at Staten Island University Hospital over a period of 6 months from July 2003 to February 2004. All patients signed a written consent form. Twenty cases of laparoscopic sterilization (LS) were performed using Faloperings, and 20 cases of hysteroscopic sterilization (HS) were performed using the Essure system. All procedures were performed in an ambulatory surgical center. All patients undergoing LS received general anesthesia with endotracheal intubation. Among the HS cases, 12 were performed using local anesthesia and IV sedation, and 8 were performed using general anesthesia. Injection Toradol was given 30 to 40 minutes before hysteroscopy to prevent tubal spasm. To ensure contraception for 3 months postprocedure, all HS patients were given either a preprocedure injection of Depo Provera or a prescription for oral contraceptives. Those patients then underwent an HSG 3 months postprocedure to ensure tubal occlusion.
Postprocedure pain was assessed in the recovery room by using a scale ranging from 0=“No pain” to 10=“Worst pain ever experienced.” Pain scores were compared by independent t tests, assuming unequal variances, due to the distributions of the data. Patient satisfaction was assessed 3 months postprocedure by using a scale ranging from 1% to 100%. Patient report of pain medication use, return to normal activity, and patient satisfaction was collected via telephone individually by the authors or their designee after 3 months. The HS patients were surveyed at their HSG appointment.
RESULTS
Before sterilization, 12.5% of the study participants were using a barrier method for contraception, 32.5% were using a hormonal method, 2.5% were using an IUD, and 52.5% reported using no contraception. The patients in both sterilization groups were similar in parity (LS group median, 3 children; HS group median, 2) and gravidity (median, 3 pregnancies among LS patients and 3.5 among HS patients). Both groups were 40% Caucasian. The HS patients tended to be older (median, 42.5 years of age) than the LS patients (median, 38 years). The HS patients also tended to have lower body mass index (BMI) scores (BMI mean, 23.52, median, 22.60) than did the LS patients (BMI mean, 30.11, median, 27.21).
Additional procedures were performed concomitantly in 9 of the 20 (45%) HS cases and in 1 (5%) of the LS cases. Concomitant procedures are listed in Table 1. Among cases performed without concomitant procedures, average HS procedure time was 26 minutes, and average LS procedure time was 75 minutes. No complications occurred during any of the procedures.
Table 1.
Procedures Performed Concomitantly With Sterilization
| Hysteroscopic Sterilization (n=9) |
| Submucosal resection |
| Endometrial biopsy (n=2) |
| Vulva biopsy |
| Fibroid removal |
| Umbilical hernia repair |
| Dilatation and curettage (n=3) |
| Laparoscopic Sterilization (n=1) |
| Lysis of omental adhesions |
Pain was assessed immediately postoperatively. The average pain score at that time was significantly lower among HS patients (mean, 0.60, median, 0) than among LS patients (mean, 5.05, median, 6; t=−8.17, P<.0001). Pain medication postprocedure was required for 3% of the HS group and 85% of the LS group. All LS patients remained under observation for 2 hours postprocedure; HS patients remained an average of 51 minutes.
Pain was assessed again 1 week postprocedure. None of the patients in the HS group reported any pain, while the average pain score among the LS patients was 2.65 (median, 3; t=−9.67, P<0001). HS patients reported returning to work an average of 1.35 days after the sterilization procedure, and LS patients returned to work an average of 14 days postprocedure. Among the LS group, 25% reported minimal spotting, and 75% reported mild bleeding during the week following the procedure. Within the HS group, 40% reported minimal spotting, and the remaining 60% reported no bleeding. Four weeks postprocedure, the women in the HS group continued to report no pain, 35% of the LS group continued to report some pain (mean pain score, 0.60, median, 0; t=−3.04, P=.004). Pain data comparisons are summarized in Figure 1.
Figure 1.
Comparison of mean pain scores at 3 time points after sterilization.
Tubal occlusion was evidenced in all HSGs performed within the HS group at 3 months postprocedure. All HS patients reported 100% satisfaction with the procedure; the mean satisfaction rating within the LS group was 69% (median, 60%).
CONCLUSION
The results of this study indicate that patients undergoing hysteroscopic sterilization experience significantly less pain than those undergoing laparoscopic sterilization. While no pain was reported in the hysteroscopic group at 1-week follow-up, some laparoscopic patients continued to report pain as long as a month following surgery. Our study has confirmed the findings of Duffy et al6 in their series published in November 2005. An additional observation in this study is that in a 2-year follow-up, no pregnancies have been reported.
There are some weaknesses in this study. Tolerance to pain was not assessed before the procedures. It is possible that there was an inherent difference in the pain tolerance between the members of both groups. The sample size is small and therefore limits the generalization of the results. All laparoscopic sterilization procedures were performed using the Falope ring; therefore, this study cannot address differences in pain with other methods. In addition, several of the hysteroscopic patients had other procedures performed concomitantly with their sterilizations. However, this is more likely to increase the potential to experience greater pain postoperatively, rather than creating a favorable bias.
There are many advantages to hysteroscopic over laparoscopic sterilization. Hysteroscopically sterilized patients do not require general anesthesia, and they receive confirmation of their sterilization with a follow-up HSG. Hysteroscopic patients in this study reported less pain and required less postprocedure pain medication than did laparoscopic patients. Hysteroscopic patients returned to normal activity sooner and expressed a greater level of overall satisfaction. However, there are some contraindications to hysteroscopic sterilization, and not all women are appropriate candidates. These findings suggest that hysteroscopic sterilization offers a higher standard of patient care than laparoscopic sterilization offers, and, where available, should be offered to women seeking sterilization.
Contributor Information
Radha Syed, Staten Island University Hospital, Staten Island, New York, USA..
Jenna Levy, Staten Island University Hospital, Staten Island, New York, USA..
Meredith E. Childers, Conceptus, Inc, Mountain View, California, USA..
References:
- 1. Kerin JF, Carignan CS, Cher D. The safety and effectiveness of a new hysteroscopic method for permanent birth control: results of the first Essure pbc clinical study. Aust N Z J Obstet Gynaecol. 2001;41(4):364–370 [DOI] [PubMed] [Google Scholar]
- 2. Cooper JM, Price T, Herendael BJ, Cayuela-Font E, Cher D, Carignan CS. Hysteroscopic sterilization using a micro-insert device: results of a multicentre Phase II study. Hum Reprod. 2003;18(6):1223–1230 [DOI] [PubMed] [Google Scholar]
- 3. Cooper JM, Carignan CS, Cher D, Kerin JF, Selective Tubal Occlusion Procedure 2000 Investigators Group Microinsert nonincisional hysteroscopic sterilization. Obstet Gynecol. 2003;102(1):59–67 [DOI] [PubMed] [Google Scholar]
- 4. Kerin JF, Munday DN, Ritossa MG, Pesce A, Rosen D. Essure hysteroscopic sterilization: results based on utilizing a new coil catheter delivery system. J Am Assoc Gynecol Laparosc. 2004;11(3):388–393 [DOI] [PubMed] [Google Scholar]
- 5. Fraser RA, Hotz SB, Hurtig JB, Hodges SN, Moher D. The prevalence and impact of pain after day-care tubal ligation surgery. Pain. 1989;39(2):189–201 [DOI] [PubMed] [Google Scholar]
- 6. Duffy S, Marsh F, Rogerson L, et al. Female sterilisation: a cohort controlled comparative study of ESSURE versus laparoscopic sterilization. BJOG. 2005;112(11):1522–1528 [DOI] [PubMed] [Google Scholar]