Abstract
Background:
Recurrence and reflux are 2 most important remote complications of lap-paraesophageal hernia (PEH) repair. However, the extent of recurrence remains unknown. We sought to determine the true incidence of recurrence after lap-PEH repair.
Methods:
A meta-analysis was carried out. PubMed, EMBASE, Cochrane Library, hand search, and personal communication were used to access and appraise studies. The inclusion criteria were full-text papers published from 1991 to date that describe lap-PEH repair in >25 patients, have at least a 6-month follow-up, and address the issue of recurrence. “Wrap migration” papers were excluded. Papers were appraised and the data were isolated on summary sheets. MS Office Excel 2003 was used to plot the results and represent it in graphs.
Results:
Thirteen studies were eligible (all retrospective case series). A total of 965 patients with 99 recurrences were noted. The overall recurrence rate (in all patients) was 10.2% and was 14% if only the followed up patients (n=658/965) were considered. However, when patients with objective evidence (follow-up Ba esophagogram) were used (301/965), the “true” recurrence rate was 25.5% (ie, 1 in 4 recurred). The learning curve did not appear to be an issue (P=0.27). The studies revealed broad 95 CI and touched the line-of-no-effect, thereby increasing the “chance factor.” When an alternate model was applied, esophageal lengthening (by Collis-Nissen gastroplasty) revealed a significant protective influence (P<0.0001).
Conclusion:
The true incidence of lap-PEH recurrence is 25.5%. The learning curve is not an adequate explanation. Mandatory (protocol) follow-up esophagograms at 1 year are essential. Two emphasis points in the repair have emerged: hiatoplasty and (superadded) esophageal lengthening.
INTRODUCTION
Recurrence and reflux are the 2 main postoperative remote complications of laparoscopic repair of the not-so-rare paraesophageal hernia (PEH). This is supported by the available retrospective studies. We concluded the same at a free paper presentation of a nonexhaustive nevertheless extensive narrative review of lap-PEH repair at the semi-annual meeting (2004) of the Ulster Society of Gastroenterology, a province-wide organization in Northern Ireland, UK. The recurrence of lap-PEH repair is quoted as 5% to 42%. It describes the range between the lowest and the highest figures in the literature. This study was carried out to determine the true incidence of recurrence after lap-PEH repair.
METHODS
A metaanalysis of studies describing lap-PEH repair was carried out. The paper search dates were from 1991 (a year before the start of laparoscopic esophageal practice) to February 2006 (the time to collate the data). The National Library of Medicine (NLM) USA was indirectly accessed via its PubMed outlet. Other search sources include EMBASE, Cochrane Library, hand search, and personal communication. The key words used for database searches were “laparoscopic,” “paraesophageal,” “hernia,” “recurrence” in combinations. Paper inclusion criteria included primary study, full text article, study involving lap-PEH repair, n>25 (learning curve estimated at 20 to 35 operations), >6-month follow-up, recurrence addressed, and studies in the English language. Studies describing repair of failed Nissen fundoplication (wrap migration) alone, were excluded. The primary outcome of this meta-analysis was the detection of recurrence.
Two authors individually critically appraised the papers. No scoring system was used for quality grading (due to the retrospective nature of the participating studies). A third appraiser resolved disputes between appraisers. The “discussion” section of the papers was considered only if directly explaining the original work. For multiple studies from the same institution, only the most recent study or the one with the highest sample power was used, as decided on the basis of consensus. The data were extracted on to summary sheets for instant access and then entered into Microsoft Excel 2003. The graphs were used to analyze and present the data.
The chi-square test was used for pre- and post-2000 comparison, to calculate heterogeneity, and for alternate models (P value accepted at 0.05).
RESULTS
Thirteen studies qualified (Table 1). All were retrospective case series (Level 4 evidence according to Oxford Centre for Evidence-Based Medicine classification 2001). Five studies were released before the year 2000 and 8 thereafter. The paper by Wiechmann (2001)12 was counted as a pre-2000 study, because the evaluated data ranged from 1993 through 1997. The critical appraisal revealed a general tendency among studies for lack of a clearly stated aim, selection bias (underpowered), performance bias (evolving technique over the decade), detection bias (very high follow-up loss, deficiency of objective evidence like follow-up esophagogram or CT). There was no significant confounding due to extraneous factors like age, sex, race, and social class.
Table 1.
Summary of Eligible Trials*
| Study | n | Gastroplasty (E/lengthening) | Overall Recurrence | Recurrence in Esophagograms |
|---|---|---|---|---|
| Mattar 20021 | 125 | 6 | 14 (11.2%) | 14/32 (43.75%) |
| Diaz 20032 | 116 | 6 | 21 (18%) | 21/66 (31.8%) |
| Champion 20033 | 52 | 18 | 1 (1.9%) | 1/27 (3.7%) |
| Pierre 20024 | 200 | 113 | 5 (2.5%) | NS |
| Leeder 20035 | 53 | - | 5 (9.4%) | NS |
| Ferri 20046 | 35 | - | 7 (20%) | 7/31 (22.58%) |
| Perdikis 19977 | 65 | - | 10 (15.3%) | 10/46 (21.73%) |
| Edye 19988 | 55 | - | 5 (9%) | NS |
| Hashemi 20009 | 27 | - | 9 (33.3%) | 9/21 (42.8%) |
| Trus 199710 | 76 | 6 | 5 (6.5%) | NS |
| Gantert 199811 | 55 | - | 2 (3.6%) | NS |
| Wiechmann 200112 | 54 | - | 4 (6.6%) | 4/44 (9.09%) |
| Jobe 200213 | 52 | - | 11 (21%) | 11/34 (32.35%) |
Chi-square test for heterogeneity = 56.99, DF = 12, P < 0.0001.
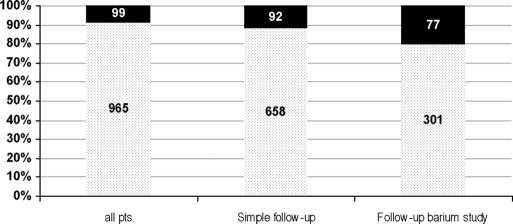
A total of 965 patients had the lap-PEH repair. There were 99 recurrences. The overall incidence of recurrence from all patients (n=965) was 10.2% (mean of all studies=12.2%, median=9.4%, IQR=6.5 to18.1), increasing to 14% (mean of all eligible studies=16.8%, median=16.8%, IQR=8.5 to 21.18) among patients followed up (n=658). When only the patients with a follow-up esophagogram were considered (n=301), the true recurrence rate was 25.5% (mean of all eligible studies=24.7%, median=27.1, IQR=18.5 to 32.5) (Figure 1). Among pre-2000 studies, 26/305 recurrences (8.5%) were seen compared with 73/ 660 (11%) in post-2000 studies (OR=1.33, RR=1.29, P=0.2) (Table 2). This suggests that the learning curve of the cumulative, all-inclusive experience over a decade is probably not the cause for the lack, or otherwise, of differences in the incidence of recurrence.
Figure 1.
Detection of recurrence increases with the vigor of search from simple clinical follow-up to follow-up esophagogram (10.2% overall to 14% in simple follow-up to 25.5% in esophagogram cohort).
Table 2.
Comparison of Recurrence Rate in Pre-2000 and Post-2000 Studies (8.52% vs 11% P = 0.27), Suggesting Lack of Improvement Over a Decade
| Study | n | Recurrence |
|---|---|---|
| Pre-2000 (heterogeneity P = 0.19) | ||
| Perdikis | 65 | 10 (15.3%) |
| Edye | 55 | 5 (9%) |
| Trus | 76 | 5 (6.5%) |
| Gantert | 55 | 2 (3.6%) |
| Wiechmann | 54 | 4 (6.6%) |
| Total | 305 | 26 (8.5%) |
| Post-2000 (heterogeneity P < 0.0001) | ||
| Mattar | 125 | 14 (11.2%) |
| Diaz | 116 | 21 (18%) |
| Champion | 52 | 1 (1.9%) |
| Pierre | 200 | 5 (2.5%) |
| Leeder | 53 | 5 (9.4%) |
| Ferri | 35 | 7 (20%) |
| Hashemi | 27 | 9 (33.3%) |
| Jobe | 52 | 11 (21%) |
| Total | 660 | 73 (11%) |
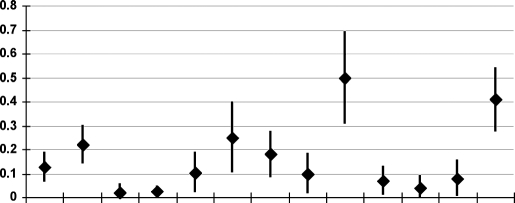
The plotted graphs revealed broad confidence intervals, touching the line of no-effect suggesting an increased chance factor. Clinical heterogeneity existed among plotted individual studies shown by lack of overlap between dot-and-line results (Figure 2). Statistical heterogeneity was shown by chi-square=56.99 with degrees of freedom (DF)=12 (P<0.0001). For the outcome of interest (ie, incidence of recurrence) however, this heterogeneity has been ignored.
Figure 2.
Odds of recurrence in individual studies (n=965, recurrence=99). Statistical heterogeneity (chi squared=56.99, degrees of freedom=12, P<0.0001). “Visual” heterogeneity is revealed by lack of overlap between lines. Believed to be a combination of selection, performance, and detection bias.
For sensitivity analysis, 2 alternate models were constructed. In the first (Table 3), all patients who had esophageal lengthening (added Collis-Nissen procedure) were isolated and compared with those with conventional repair (sac excision, cruroplasty, non-Collis-Nissen fundoplication). It revealed 816 conventional repairs with 99 recurrences (12%) as opposed to 0/149 in the CollisNissen group (P<0.0001).
Table 3.
Sensitivity analysis of Studies With Esophageal Lengthening (Collis or Collis-Nissen gastroplasty). Recurrence Rate for Gastroplasty vs Non-gastroplasty Repairs Within the Given Study (P < 0.0001)
| Study | n | Recurrence |
|---|---|---|
| No Gastroplasty | ||
| Mattar 2002 | 119 | 14 (11.7%) |
| Diaz 2003 | 110 | 21 (19%) |
| Champion 2003 | 34 | 1 (3%) |
| Pierre 2002 | 87 | 5 (5.7%) |
| Leeder 2003 | 53 | 5 (9.4%) |
| Ferri 2004 | 35 | 7 (20%) |
| Perdikis 1997 | 65 | 10 (15.3%) |
| Edye 1998 | 55 | 5 (9%) |
| Hashemi 2000 | 27 | 9 (33.3%) |
| Trus 1997 | 70 | 5 (7%) |
| Gantert 1998 | 55 | 2 (3.6%) |
| Wiechmann 2001 | 54 | 4 (7.4%) |
| Jobe 2002 | 52 | 11 (21%) |
| Total | 816 | 99 (12%) |
| Gastroplasty | ||
| Mattar 2002 | 6 | 0 |
| Diaz 2003 | 6 | 0 |
| Champion 2003 | 18 | 0 |
| Pierre 2002 | 113 | 0 |
| Trus 1997 | 6 | 0 |
| Total | 149 | 0 |
In the second (hypothetical) model (Table 4), the worst-case scenario (WCS) was applied in which all recurrences in a given study were attributed to the Collis-Nissen group. This revealed 76/816 (9.3%) recurrences. The Collis-Nissen group had an incidence of recurrence of 23/149 (15.4%) (OR=1.77, RR=1.65, P=0.03).
Table 4.
Sensitivity analysis of Studies With Esophageal Lengthening (Collis or Collis-Nissen Gastroplasty) Using a Hypothetical “Worst Case Scenario” (WCS)*
| Study | n= | Recurrence |
|---|---|---|
| No Gastroplasty | ||
| Mattar 2002 | 119 | 8 (6.7%) |
| Diaz 2003 | 110 | 15 (13.6%) |
| Champion 2003 | 34 | 0 |
| Pierre 2002 | 87 | 0 |
| Leeder 2003 | 53 | 5 (9.4%) |
| Ferri 2004 | 35 | 7 (20%) |
| Perdikis 1997 | 65 | 10 (15.3%) |
| Edye 1998 | 55 | 5 (9%) |
| Hashemi 2000 | 27 | 9 (33.3%) |
| Trus 1997 | 70 | 0 (1.4%) |
| Gantert 1998 | 55 | 2 (3.6%) |
| Wiechmann 2001 | 54 | 4 (7.4%) |
| Jobe 2002 | 52 | 11 (21%) |
| Total | 816 | 76 (9.3%) |
| Gastroplasty | ||
| Mattar 2002 | 6 | 6 (100%) |
| Diaz 2003 | 6 | 6 (100%) |
| Champion 2003 | 18 | 1 (5.5%) |
| Pierre 2002 | 113 | 5 (4.4%) |
| Trus 1997 | 6 | 5 (83.3%) |
| Total | 149 | 23 (15.4%) |
Recurrences in the given study were attributed to the gastroplasty and the recurrence rate determined for gastroplasty vs nongastroplasty repairs within the given study (9.3% vs 15.4%, P = 0.03).
DISCUSSION
Metaanalyses commonly involve randomized controlled trials. However, for this single-issue metaanalysis, no randomized trials were available to address the knowledge gap about the incidence of arguably the most important outcome parameter of lap-PEH repair. The heterogeneity seen above would tend to preclude a metaanalysis. The methodological flaws in the participating studies were not sufficient to prevent insight into the recurrence rate. The initial studies dwelled on immediate outcome like injuries, conversion, mortality, and above all length of stay. The most important issues of recurrence and reflux have been in the background.
The technique has evolved over the last decade of the 20th century, moving from simple reduction and cruroplasty to detailed sac excision, esophageal mobilization, and synthetic or biological mesh implants. This would explain the performance bias inherent in the studies. The role of antireflux procedures although controversial nevertheless has been adopted almost universally. Recently (since 1998) esophageal lengthening with procedures like Collis gastroplasty coupled with Nissen fundoplication have been used.
Even with low hierarchy evidence, we thought a meta-analysis was an appropriate means to explore the recurrence issue due to PEH being uncommon if not rare. In the participating studies, the authors have concentrated on the hiatus repair by suture, synthetic mesh, and biological small intestinal submucosal (SIS) patches. The recurrence has not been searched for specifically at the follow-up, and contrast esophagogram has been performed on a symptom-driven basis. Because a majority of recurrence is believed to be asymptomatic, detection bias results from lack of specific imaging. The attrition rate (loss of follow-up) has been high among the studies, further contributing to this problem. Unless the papers were appraised, it was difficult to determine whether the quoted recurrence rate is from the overall cohort or from the stringently followed up patients.
Some authors have used esophageal lengthening, and it appears to confer benefit to the repair. It is possible that the hiatoplasty may need to be coupled with an esophageal lengthening procedure. More data are needed on this issue.
CONCLUSION
The most important outcome parameter for lap-PEH repair has not been quantified thus far. Only retrospective evidence was available for metaanalysis. The true incidence of recurrence is 25.5%. The learning curve is not an adequate explanation. Mandatory (protocol) follow-up esophagogram at (for example) 1 year would provide a tool for detection of recurrence. Esophageal lengthening appears to have a positive influence. In addition to conventional hiatoplasty, there may be an additional emphasis point in achieving a tension-free secure repair in the form of esophageal lengthening.
Contributor Information
Munir Ahmad Rathore, Department of Surgery, Antrim Area Hospital, Northern Ireland, United Kingdom..
Syed Imran Hussain Andrabi, Craigavon Area Hospital, Northern Ireland, United Kingdom..
Muhammad Iqbal Bhatti, Lagan Valley Hospital, Lisburn Northern Ireland, United Kingdom..
Syed Muzahir Hussain Najfi, Department of Surgery, Antrim Area Hospital, Northern Ireland, United Kingdom..
Arthur McMurray, Department of Surgery, Antrim Area Hospital, Northern Ireland, United Kingdom..
References:
- 1. Mattar SG, Bowers SP, Galloway KD, Hunter JG, Smith DC. Long-term outcome of laparoscopic repair of paraesophageal hernia. Surg Endosc. 2002;16(5):745–749 [DOI] [PubMed] [Google Scholar]
- 2. Diaz S, Brunt LM, Klingensmith ME, Frisella PM, Soper NJ. Laparoscopic paraesophageal hernia repair, a challenging operation: Medium-term outcome of 116 patients. J Gastrointest Surg. 2003;7(1):59–66 [DOI] [PubMed] [Google Scholar]
- 3. Champion JK, Rock D. Laparoscopic mesh cruroplasty for large paraesophageal hernias. Surg Endosc. 2003;17(4):551–553 [DOI] [PubMed] [Google Scholar]
- 4. Pierre AF, Luketich JD, Fernando HC, et al. Ann Thorac Surg. 74(6):1909–1915, 2002 [DOI] [PubMed] [Google Scholar]
- 5. Leeder PC, Smith G, Dehn TCB. Laparoscopic management of large paraesophageal hiatal hernia. Surg Endosc. 2003;17(9): 1372–1375 [DOI] [PubMed] [Google Scholar]
- 6. Ferri LE, Feldman LS, Stanbridge D, Mayrand S, Stein L, Fried GM. Should laparoscopic paraesophageal hernia repair be abandoned in favor of the open approach? Surg Endosc. 2005;19(1):4–8 [DOI] [PubMed] [Google Scholar]
- 7. Perdikis G, Hinder RA, Filipi CJ, Walenz T, McBride PJ, Smith SL, Katada N, Klingler PJ. Laparoscopic paraesophageal hernia repair. Arch Surg. 1997;132(6):586–589 [DOI] [PubMed] [Google Scholar]
- 8. Edye MB, Canin-Endres C, Gattorno F, Salky B. Durability of laparoscopic repair of paraesophageal hernia. Ann Surg. 1998; 228(4):528–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hashemi M, Peters JH, DeMeester TR, et al. Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg. 2000;190(5):553–560 [DOI] [PubMed] [Google Scholar]
- 10. Trus TL, Bax T, Richardson WS, et al. Complications of laparoscopic paraesophageal hernia repair. J Gastrointest Surg. 1997;1(3):221–228 [DOI] [PubMed] [Google Scholar]
- 11. Gantert WA, Patti MG, Arcerito M, et al. Laparoscopic repair of paraesophageal hiatal hernias. J Am Coll Surg. 1998;186(4): 428–432 [DOI] [PubMed] [Google Scholar]
- 12. Wiechmann RJ, Ferguson MK, Naunheim KS, et al. Laparoscopic management of giant paraesophageal herniation. Ann Thorac Surg. 2001;71(4):1080–1086 [DOI] [PubMed] [Google Scholar]
- 13. Jobe BA, Aye RW, Deveney CW, Domreis JS, Hill LD. Laparoscopic management of giant type III hiatal hernia and short esophagus: objective follow-up at three years. J Gastrointest Surg. 2002;6(2):181–188 [DOI] [PubMed] [Google Scholar]