Abstract
Background:
A 43-year-old woman with recurrent hiccup and discomfort in the right upper abdomen was diagnosed by computed tomographic (CT) scan with a cystic tumor in the right liver. Echinococcus serology was negative.
Methods:
A laparoscopic procedure was chosen as standard therapy for symptomatic cystic liver tumors. The presumed tumor turned out to be a diaphragmatic cyst 8 cm in diameter at the center of the right hemi-diaphragm. By using the ultrasonic device, the cystic tumor was completely and safely removed from the diaphragm. The defect was closed by using nonabsorbable sutures. A chest drain was inserted for 1 day.
Results:
The postoperative course was uneventful, and the patient was discharged on day 4. The histopathological examination revealed a bronchogenic cyst. No recurrence was noted by CT-scan after 12 and 24 months.
Conclusions:
Due to this rare diagnosis, the intradiaphragmatic location of a bronchogenic cyst is difficult to identify with radiological methods. Complete surgical excision is the treatment of choice. The conventional surgical approach is a posterolateral thoracotomy. In the literature, video-assisted thoracoscopic surgery (VATS) has been described as a safe and effective procedure. In our case, we could demonstrate that the laparoscopic excision of a cyst including partial diaphragmatic resection can be done safely in a diaphragmatic location with all the advantages of minimally invasive surgery.
Keywords: Intradiaphragmatic cyst, Bronchogenic cyst, Laparoscopy, Minimally invasive
CASE REPORT
A 43-year-old woman with recurrent hiccup and discomfort in the right upper abdomen had a cystic tumor in the right liver (S7) discovered by computed tomographic (CT) scan (Figure 1). Echinococcus serology was negative. As usual for symptomatic cystic liver tumors, we chose a laparoscopic procedure. The patient was placed in a combined 30° to 40° reversed Trendelenburg and French position and was rotated to the left side. Four trocars and a 30° optic were used (Figure 2). The right liver was completely mobilized by using the ultrasonic dissector (Ultracision, Ethicon Endo-Surgery, Cincinnati, OH).
Figure 1.
Preoperative computed tomographic scan; cystic tumor (3) in projection to the right liver.
Figure 2.
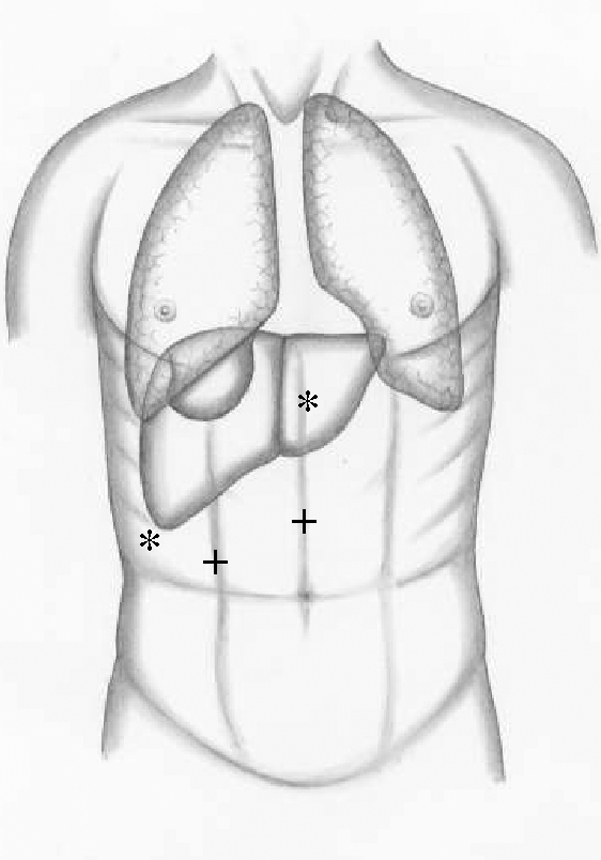
Laparoscopic resection of an intradiaphragmatic bronchogenic cyst. Position of trocars: * 5–mm trocar, + 10-mm trocar.
RESULTS
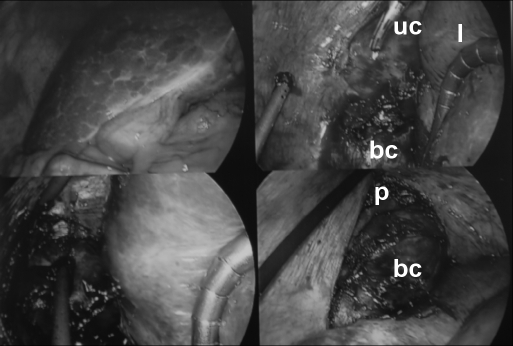
The presumed tumor turned out to be a diaphragmatic cyst at the center of the right hemi-diaphragm. It measured 8 cm in diameter. The cystic tumor was completely resected including a 1-cm muscle margin from the diaphragm (Figure 3). The closure of the diaphragm could be done safely with nonabsorbable sutures (overlapped, interrupted u-stitches, n=5, extracorporeally knotted; 2–0 Ethibond, Ethicon). Operation time was 72 minutes; there was no significant blood loss. The histopathological examination showed a bronchogenic cyst filled with viscous, mucoid material. The surface of the tumor contained cartilaginous plates, smooth muscle, and bronchial mucous glands. It was lined by ciliated pseudo-stratified columnar epithelium. A chest drain was placed for 1 day. The postoperative course was uneventful, and the patient was discharged on day 4. No recurrence was noted by CT-scan during the follow-up period of 24 months.
Figure 3.
Laparoscopic view of the right diaphragm (bc: bronchogenic cyst; l: liver; uc: ultracision; p: pulmo).
DISCUSSION
Bronchogenic cysts are developmental anomalies of the foregut. They are usually located in the mediastinum or lung parenchyma. An intradiaphragmatic location is very rare.
Regardless of their location, bronchogenic cysts are lined by ciliated pseudo-stratified columnar epithelium similar to cells of the respiratory tract. The surfaces contain cartilaginous plates, smooth muscle, and bronchial mucous glands. They are filled with viscous, mucoid material.
An intradiaphragmatic location remains difficult to diagnose with any imaging modality due to the thin, curved structure of the diaphragm.1–4 Any mass lesion may protrude either towards the thoracic or, as shown in our case, the abdominal cavity and can easily be misdiagnosed as a cystic tumor of the liver. In select patients, dynamic ultrasound examination may be helpful to localize the cyst in relation to the diaphragm.
Complete surgical excision is the treatment of choice. The conventional surgical approach is a posterolateral thoracotomy. Chang et al4 showed that video-assisted thoracoscopic surgery (VATS) is effective and safe.
A laparoscopic approach was chosen initially because of a suspected uncomplicated hepatic cyst. Retrospectively, this approach proved to be correct; although the cyst originated from the diaphragm, it expanded mainly into the abdominal cavity, and therefore the margins of the cyst could be visualized best from the abdominal side of the diaphragm. The reverse Trendelenburg position and pneumoperitoneum facilitated a safe suture technique without the risk of liver damage. With the first suture, the diaphragmatic dome was pulled down into the abdominal cavity, thereby providing a safe distance to pulmonary tissue. Double-lumen intubation was not necessary, a very important advantage compared with the thoracoscopic approach. The laparoscopic excision of the cyst including partial diaphragmatic resection proved to be safe. The closure of the diaphragmatic defect by using interrupted u-stitches with nonabsorbable material has already been described as a safe technique.5,6 Also, we were able to create a tension-free repair using single stitches. Therefore, no mesh had to be used.
Contributor Information
Nico P. Zügel, Department of Surgery, Centre Hospitalier Emile Mayrisch (CHEM), Esch-surAlzette/Luxembourg.; Department of Surgery, Klinikum Groβhadern, University of Munich, Munich, Germany.
Martin Kox, Department of Surgery, Centre Hospitalier Emile Mayrisch (CHEM), Esch-surAlzette/Luxembourg..
Reinhold A. Lang, Department of Surgery, Klinikum Groβhadern, University of Munich, Munich, Germany..
Thomas P. Hüttl, Department of Surgery, Klinikum Groβhadern, University of Munich, Munich, Germany..
References:
- 1.Coselli MP, Ipolyi PD, Bloss RS, Diaz RF, Fitzgerald JB. Bronchogenic cysts above and below the diaphragm: report of eight cases. Ann Thorac Surg. 1987;44:491–494 [DOI] [PubMed] [Google Scholar]
- 2.Dagenais F, Nassif E, Dery R, Lapoint R. Bronchogenic cyst of the right hemidiaphragm. Ann Thorac Surg. 1995;59:1235–1257 [DOI] [PubMed] [Google Scholar]
- 3.Rozenblit A, Iqbal A, Kaleya R, Rozenblit G. Case report: intradiaphragmatic bronchogenic cyst. Clinical Radiol. 1998;5:918–920 [DOI] [PubMed] [Google Scholar]
- 4.Chang Y, Chen J, Chang YL, Lee YC. Video-assisted thoracoscopic excision of intradiaphragmatic bronchogenic cysts: two cases. J Laparoendo Advanc Surg Techn. 2006;16:489–492 [DOI] [PubMed] [Google Scholar]
- 5.Meyer G, Hüttl TP, Hatz RA, Schildberg FW. Laparoscopic repair of traumatic diaphragmatic hernias. Surg Endosc. 2000;14(11):1010–1014 [DOI] [PubMed] [Google Scholar]
- 6.Rittler P, Boehm R, Hüttl TP, Meyer G, Schildberg FW. Laparoscopic repair of an extrahiatal hernia caused by congenital dysplasia: a case report. Surg Endosc. 2002;16(2):358. [DOI] [PubMed] [Google Scholar]