Abstract
Background:
Appendicectomy has traditionally been a training operation for junior surgical trainees. With the increased incidence of laparoscopic appendicectomy, concern has increased about the safety of this far more technically demanding procedure in the hands of junior surgical trainees. The learning curve of a junior surgeon is presented.
Methods:
Consecutive patients having laparoscopic appendicectomy were studied. A 3-port Hasson technique was used. Patient demographics, conversion rate and reason for conversion, operation times, number of complicated cases (retrocecal position, dense adhesions, perforated/gangrenous/abscess associated appendicitis), and postoperative complications were recorded. The moving average and cumulative sum (CUSUM) methods were used to delineate the learning curve.
Results:
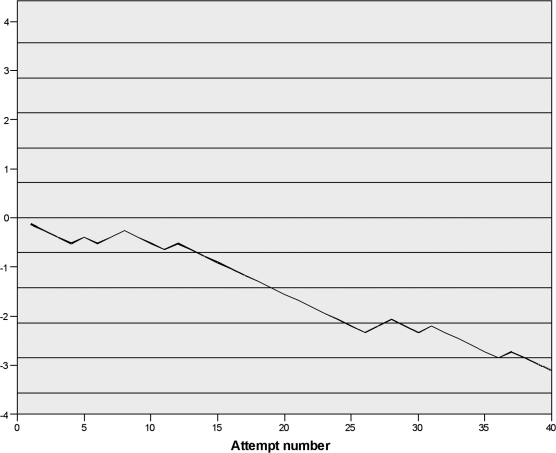
Forty patients were studied. Median age was 24 (IQR: 18, 40). Twenty-nine (72.5%) patients were female. Data were not available for 3 patients (6%); the remaining patients form the basis of this study. A statistically significant improvement occurred in operating time between group 2 and group 3, P<0.0001 (95% CI, 21.23 to 47.99). The CUSUM plot demonstrates that the learning curve was surmounted by 20 cases performed.
Conclusions:
Laparoscopic appendicectomy is a safe procedure for junior trainees, and the learning curve stabilizes by 20 cases performed.
INTRODUCTION
Open appendicectomy has traditionally been a training operation for junior surgical trainees. With the increased incidence of laparoscopic appendicectomy (LA), there has been concern about the safety of this far more technically demanding procedure in the hands of junior surgical trainees.1,2 The learning curve of a UK surgical registrar in the first year of training is presented.
METHODS
From May 2005 to November 2006, consecutive patients with suspected appendicitis were taken to the surgical theater with the intent to perform LA. A 3-port technique was used, with 10-mm ports inserted in the infraumbilical and suprapubic positions and a 5-mm port in the left iliac fossa. The first puncture was open and infraumbilical. The appendix was skeletonized by using mono-polar hook diathermy, and appendicectomy was performed between preformed ligatures, 2 placed proximally on the appendix base and 1 distally. The appendix was removed either though a 10-mm port or via a retrieval bag. Peritoneal lavage was performed where evidence was present of peritoneal contamination, and fascial closure of all 10-mm port incisions was achieved with delayed absorbable suture material.
Patient demographics, conversion rate and reason for conversion, operation duration, number of complicated cases (perforated/gangrenous/abscess-associated appendicitis), and postoperative complications were recorded. This study is a single trainee learning curve evaluation. The moving average and cumulative sum methods were used to delineate the learning curve. For the moving average analysis, the series of 40 patients consecutively operated on was divided into 4 groups of 10 patients each.
Statistical Analysis
The moving average method for operating time has been described in constructing learning curves for attaining new procedural skills.3
The cumulative sum (CUSUM) method is a statistical process developed to assure quality in a continuous process and has been applied to constructive learning curves for acquisition of new procedural skills.4,5 The CUSUM value is a mixture of sequential increments (1-s) and decrements (s), corresponding to failure and success at the task being examined. Boundary lines on the CUSUM plot are based on acceptable and unacceptable failure rates and the defined type 1 (false positive) and type 2 (false negative) error rates. The CUSUM plot may cross an acceptable boundary line (from above) or an unacceptable boundary line (from below). Previously described CUSUM formula and graphical representation were used.6
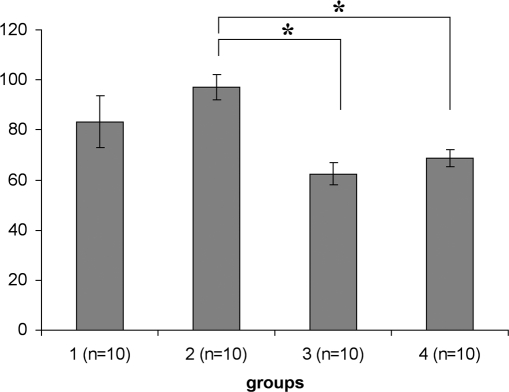
Figure 1.
Operating times by moving average method for consecutive groups of 10 patients (mean ± SEM): group 1 = 83.16±10.37; group 2 = 97.11±5.13; group 3 = 62.5±4.5; group 4 = 68.75±3.24. *P<0.0005.
Figure 2.
CUSUM plot for conversion to open appendicectomy. Solid horizontal lines represent threshold values. Two threshold values crossed by 20 cases indicating learning curve plateau.
Type 1 and type 2 errors were defined as 0.1.7 For purposes of analysis, the acceptable failure rate was considered 10%, and the unacceptable failure rate was considered 30%.
Data are presented as mean ± standard error of mean (SEM) or median, interquartile range (IQR). Statistical analysis was performed using the Student t test. Data were analyzed using Microsoft Excel (version 2003, Microsoft Corp, Redmond, WA, USA) and SPSS for Windows (version 15, SPSS Inc, Chicago IL, USA).
RESULTS
Forty patients were studied. Median age was 24 (IQR: 18, 40). Twenty-nine (72.5%) were female. Data were not available for 3 patients (6% due to missing records); the remainder form the basis of this study.
In Group 1, one procedure was converted to open due to the preference of the consultant surgeon responsible for the patient. The negative appendicectomy rate was 6 (15%).
Operating time decreased from 97.11±5.13 minutes in group 2 to 62.5±4.5 minutes in group 3 (P<0.0001; 95% CI 21.23 to 47.99), which remained unchanged in group 4.
Overall conversion rate to open surgery was 20%; all cases converted were of acute appendicitis with peritonitis secondary to perforation of the appendix. The rate of complicated appendicitis was 47.5% (19 cases).
CONCLUSION
The prevalence of complicated appendicitis (perforation or abscess) in our series was high at 19 (47.5%). Other reports of experience with LA report far lower incidences of complicated appendicitis, for example 10%.8 The high rate of conversion to open surgery (20%) may reflect the high incidence of complicated appendicitis.
In this series, the rate of negative appendicectomy was low (6 of 40; 15%). This may be explained by a tendency in our hospital to initially observe patients presenting with suspected appendicitis. This high threshold for operating may also explain the unusually high rate of complicated appendicitis seen in this series.
A large retrospective review9 of cases found that a clinical course of 48 to 72 hours is associated with a 34% incidence of gangrenous or perforated appendicitis compared with 4% for an interval of less than 12 hours. Another retrospective review10 reports an increased perforation rate, incidence of abscesses, and length of postoperative stay associated with a waiting time between admission to operation of greater than 24 hours. We suggest an aggressive approach to operative management should continue to be the gold standard in the era of LA.
Operation time stabilized to 62.5±4.5 minutes in the third quarter of this series. This compares favorably with that reported from the American residency program (95.7 min).11
The appendix was removed in all patients in this series. Although it has been suggested that LA may reduce the negative appendicectomy rate, a comparison of macroscopic to histological findings demonstrated that a normal-looking appendix was microscopically inflamed in 25.6% of cases.12
LA has become commonplace in the management of acute appendicitis; the improved intra-abdominal visualization being particularly useful for the female patient. Although the potential for severe complications exists, the procedure is safe. We suggest that the advent of LA should not alter indications for operating on patients with right iliac fossa pain.
The learning curve of an experienced laparoscopic surgeon suggests that 20 cases represents the number needed to gain competence.12 The consensus statement from the education committee of the European Association of Endoscopic Surgery states that LA should be part of the resident's curriculum and recommends that at least 20 cases are needed for accreditation in general surgery.13
Our series demonstrates a similar learning curve in a single UK surgical trainee. LA is a safe procedure for junior trainees, and the learning curve may stabilize by 20 cases performed. Further data from multiple trainees is required to confidently conclude that LA can be introduced early in training without compromising patient care.
Footnotes
Honorable Mention Scientific Paper presented at the 16th SLS Annual Meeting and Endo Expo 2007, San Francisco, California, September 5–8, 2007.
References:
- 1.Grunewald B, Keating J. Should the ‘normal’ appendix be removed at operation for appendicitis? J R Coll Surg Edinb. 1993;38(3):158–160 [PubMed] [Google Scholar]
- 2.Monson JR. Advanced techniques in abdominal surgery. BMJ. 1993;307(6915):1346–1350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dincler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P. Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum. 2003;46(10):1371–1378 [DOI] [PubMed] [Google Scholar]
- 4.Tekkis PP, Fazio VW, Lavery IC, et al. Evaluation of the learning curve in ileal pouch-anal anastomosis surgery. Ann Surg. 2005;241(2):262–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Molloy M, Bower RH, Hasselgren PO, Dalton BJ. Cholangiography during laparoscopic cholecystectomy– cumulative sum analysis of an institutional learning curve. J Gastrointest Surg. 1999;3(2):185–188 [DOI] [PubMed] [Google Scholar]
- 6.Kestin IG. A statistical approach to measuring the competence of anaesthetic trainees at practical procedures. Br J Anaesth. 1995;75(6):805–809 [DOI] [PubMed] [Google Scholar]
- 7.Bolsin S, Colson M. The use of the Cusum technique in the assessment of trainee competence in new procedures. Int J Qual Health Care. 2000;12(5):433–438 [DOI] [PubMed] [Google Scholar]
- 8.Levard H, Mouro J, Karayel M, Schiffino L, Berthelot G, Dubois F. Appendectomies by celioscopy. Results in 78 patients. Ann Chir. 1992;46(5):430–435 [PubMed] [Google Scholar]
- 9.Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg. 2006;244(5):656–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Omundsen M, Dennett E. Delay to appendicectomy and associated morbidity: a retrospective review. Aus N Z J Surg. 2006;76(3):153–155 [DOI] [PubMed] [Google Scholar]
- 11.Scott-Conner CE, Hall TJ, Anglin BL, Muakkassa FF. Laparoscopic appendectomy. Initial experience in a teaching program. Ann Surg. 1992;215(6):660–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meinke AK, Kossuth T. What is the learning curve for laparoscopic appendectomy? Surg Endosc. 1994;8(5):371–375 [DOI] [PubMed] [Google Scholar]
- 13.Neugebauer E, Troidl H, Kum CK, Eypasch E, Miserez M, Paul A. The E.A.E.S. consensus development conferences on laparoscopic cholecystectomy, appendectomy, and hernia repair. Consensus statements—September 1994. The Educational Committee of the European Association for Endoscopic Surgery Surg Endosc. 1995;9(5):550–563 [DOI] [PubMed] [Google Scholar]