Abstract
Background and Objectives:
Debate continues as to the merits of hand-assisted versus pure laparoscopic nephrectomy. Using evidence-based analysis, we compared the outcomes of both.
Methods:
We performed a systematic review and meta-analysis of studies directly comparing hand-assisted with pure laparoscopic nephrectomy. We searched PubMed, the OVID database (from 1980), the Biosis previews ISI Web of Knowledge (1926–2007), and abstracts from annual meetings of the American Urological Association (2002–2007). Primary outcomes were operative blood loss, operative time, hospital length of stay, perioperative transfusions, and perioperative complications. We estimated standardized mean differences and risk ratios using the random effects models.
Results:
Twenty-five studies (N=3051) met the inclusion criteria. Hand-assisted nephrectomy was associated with significantly less operative blood loss and decreased risk of conversion. There were no significant differences in mean operative time, length of stay, or risks of perioperative transfusion or complication.
Conclusions:
In this analysis, hand-assisted nephrectomy was associated with significantly less operative blood loss and risk of open conversion than was pure laparoscopic nephrectomy. The clinical significance of these findings is unclear; however, the pure and hand-assisted techniques appear to result in generally similar perioperative outcomes.
Keywords: Laparoscopy, Nephrectomy, Hand-assisted
INTRODUCTION
Laparoscopic nephrectomy is a safe, effective, and well-established surgical technique. Compared with open nephrectomy, advantages of laparoscopic nephrectomy include improved cosmesis, decreased operative blood loss, shorter hospital stay, and decreased postoperative pain.1 Many investigators believe that laparoscopic nephrectomy should now be considered the surgical standard of care in the treatment of renal neoplasm or in the performance of donor allograft nephrectomy.2,3
Still, debate persists as to the preferred approach for performing laparoscopic nephrectomy: pure laparoscopy entails use of trocars only, and hand-assisted laparoscopy combines trocars with a larger hand port. Some investigators assert that hand assistance constitutes a bridge for allowing less experienced surgeons to progress through a learning curve toward pure laparoscopy4; others argue that, because it results in outcomes identical to those of pure laparoscopy, hand assistance is an alternate technique that does not necessarily require subsequent adoption of pure laparoscopy.5
This debate stems in part from the hypothesis that hand-assisted and pure laparoscopy have different perioperative outcomes. While to our knowledge there has been only one small randomized trial comparing outcomes,6 there have been several uncontrolled cohort studies that have directly compared the laparoscopic and hand-assisted approaches in a nonrandomized fashion. Nevertheless, most of these studies were single-institution case series from which robust assumptions regarding external validity of results—and thus generalizability to clinical practice—are difficult to make.
Metaanalyses allow for the pooling and quantification of results from different studies. To our knowledge, a systematic review and metaanalysis comparing different laparoscopic techniques for nephrectomy has not been performed. Therefore, we compared outcomes of hand-assisted and laparoscopic nephrectomy utilizing evidence-based analysis.
METHODS
Search Strategy
As of July 10, 2007, separate searches were conducted of the PubMed database (January 1966 to January 2007), the OVID database (from 1980), the Biosis previews, and the ISI Web of Knowledge database (1926 to 2007). Additionally, our search included the electronic database of abstracts presented at the annual meetings of the American Urological Association from 2002 to 2007.
We retrieved citations by using combinations of the Medical Subject Heading (MeSH) term “nephrectomy” and text words “nephrectomy” and “hand.”
Study Selection, Data Abstraction, and Primary Outcomes
We included case series or cohorts that directly compared hand-assisted with pure laparoscopy within the same study. We excluded case series or cohorts of a single surgical approach that compared results to the published literature, review articles, cost analyses, and studies from which data could not be reliably extracted, including those that did not report means with standard deviations or standard errors. Studies that included alternate minimally invasive techniques for kidney extraction, including retroperitoneal laparoscopic nephrectomy or retroperitoneal hand-assisted nephrectomy, were excluded from our analyses. In cases of eligibility disagreement, the senior investigator (JKP) made the final decision regarding inclusion or exclusion of the study. If multiple studies were identified based on the same case series or cohort, the overlapping data were excluded.
The primary outcomes were operative blood loss, operative time, length of hospital stay, perioperative transfusions, and perioperative complications. We estimated standardized mean differences (SMD) and risk ratios (RR) by using random effects models.
Statistical Analysis
All statistical analyses were performed using Stata version 8.0 commercial software with latest updates for meta-analysis (Stata Corporation, College Station, TX). Subgroup analysis was performed based on indication for nephrectomy (live donor versus nephrectomy for other indications).
The DerSimonian and Laird random effects models were used. For operative blood loss, operative time, and length of stay, SMD was calculated. For perioperative transfusion, open conversions, and complications, the risk ratio and absolute risk difference (RD) were calculated.
Subgroup analyses were performed based on likely sources of between-study heterogeneity. We performed the chi-square test to evaluate the Q statistic for heterogeneity and determined the influence of each individual study on the pooled SMD, RR, and RD for each outcome. Publication bias was assessed using the Egger regression asymmetry test and the Begg adjusted rank correlation test.
RESULTS
Study Selection
The literature search yielded 3336 citations. A total of 3140 studies were excluded based on title alone; 99 were excluded after their abstracts were reviewed and 72 after their manuscripts were reviewed. Based on our criteria, we identified 25 studies (3051 patients) eligible for data extraction. The majority of studies focused on patients undergoing living related donor nephrectomy (15 studies, n = 2277 patients), with a smaller number analyzing those with other indications (10 studies, n = 774 patients).
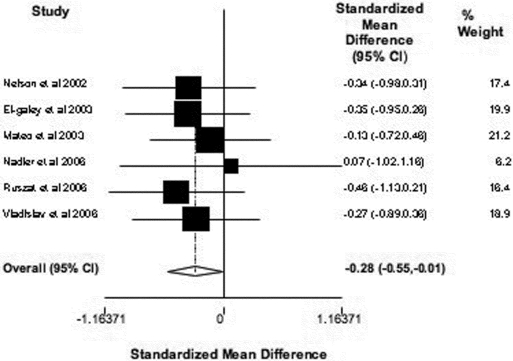
Operative Blood Loss
Six studies (n=228) evaluated operative blood loss.6–11 Compared with the pure laparoscopy group, the hand-assisted laparoscopy group was associated with significantly less operative blood loss (SMD -0.28, 95% CI -0.55 to -0.01, P=0.05) (Figure 1).
Figure 1.
Six studies (n = 228 patients) comparing operative blood loss in hand-assisted and pure laparoscopic nephrectomy. The diamond represents pooled SMD with 95% confidence limits for all studies; the squares and horizontal lines represent individual studies with 95% confidence limits.
Sequential omission of each study from the analysis, one study at a time, resulted in only slight, nonsignificant changes in the magnitude or precision of the effect estimates (data not shown). No evidence existed of publication bias by Begg's test (P=0.85) or Egger's test (P=0.34).
Four studies included only transplant patients6,8,9,11; subgroup analysis produced similar, marginally significant results (SMD -0.29, 95% CI -0.60 to -0.02, P = 0.07). Two studies included nontransplant patients7,10; subgroup analysis produced similar effect estimates but were non-significant (SMD -0.23, 95% CI -0.79 to 0.33, P=0.42).
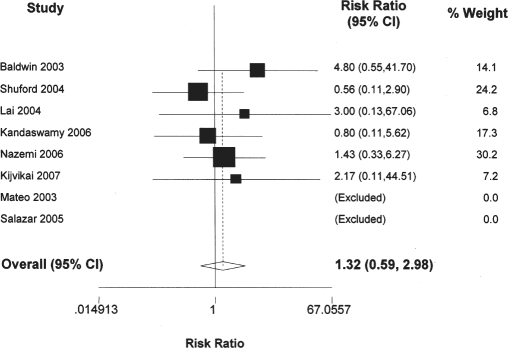
Perioperative Transfusion
Eight studies (n=817) evaluated perioperative transfusion.9,12–18 There were no significant between-group differences in overall risk (RR 1.32, 95% CI 0.95, 0.59 to 2.98, P=0.50) (Figure 2) or incidence (RD 0.00, 95% CI -0.01 to 0.01, P=0.88) of perioperative transfusion.
Figure 2.
Eight studies (n = 817 patients) comparing perioperative transfusion in hand-assisted and pure laparoscopic nephrectomy. The diamond represents pooled RR with 95% confidence limits for all studies; the squares and horizontal lines represent individual studies with 95% confidence limits. “Excluded” means 0 events.
Sequential omission of each study from the analysis, one study at a time, resulted in only nonsignificant changes in the magnitude or precision of the effect estimates (data not shown). No evidence was found of publication bias determined by using Begg's test (P=0.73) or Egger's test (P=0.47).
Four studies included only transplant patients9,14–16; subgroup analysis produced similar results (RR 1.16, 95% CI 0.95, 0.22 to 6.06, P=0.48; RD 0.00, 95% CI -0.01 to 0.01, P=0.87). Four studies included nontransplant patients12,13,17,18; subgroup analysis produced similar effect estimates but were nonsignificant (RR 1.38, 95% CI 0.54 to 3.51, P=0.50; RD 0.02, 95% CI -0.14 to 0.17, P=0.85).
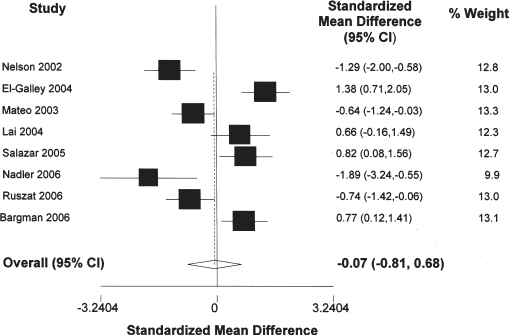
Operative Time
Eight studies (n=287) evaluated operative time.6–11,14,15 There were no significant between-group differences in mean operative time (SMD -0.07, 95% CI -0.81 to 0.68, P=0.81) (Figure 3).
Figure 3.
Eight studies (n = 287 patients) comparing operative time of hand-assisted and pure laparoscopic nephrectomy. The diamond represents pooled SMD with 95% confidence limits for all studies; the squares and horizontal lines represent individual studies with 95% confidence limits.
Sequential omission of each study from the analysis, one study at a time, resulted in only nonsignificant changes in the magnitude or precision of the effect estimates (data not shown). No evidence was found of publication bias by Begg's test (P=0.49) or Egger's test (P=0.56).
Six studies included only transplant patients6,8,9,11,14,15; subgroup analysis produced similar results (SMD 0.37, 95% CI -0.35 to 1.09, P=0.32). Two studies included nontransplant patients7,10; subgroup showed significantly reduced operative time with the hand-assisted approach (SMD -1.42, 95% CI -2.05 to -0.79, P<0.001).
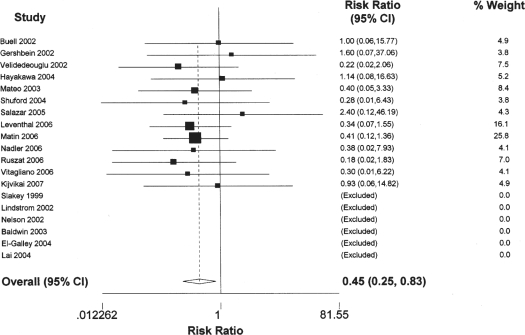
Conversions
Nineteen studies (n = 2,018) evaluated conversion rates.7–15,18–27 Hand-assisted nephrectomy was associated with a significantly decreased risk (RR 0.45, 95% CI 0.25 to 0.83, P=0.01) (Figure 4) and incidence (RD -0.01, 95% CI -0.02 to -0.001, P=0.03) of conversion.
Figure 4.
Nineteen studies (n = 2018 patients) comparing risk of conversion in hand-assisted and pure laparoscopic nephrectomy. The diamond represents the pooled RR with 95% confidence limits for all studies; the squares and horizontal lines represent individual studies with 95% confidence limits. “Excluded” means 0 events.
Sequential omission of each study from the analysis, one study at a time, resulted in only nonsignificant changes in the magnitude or precision of the effect estimates (data not shown). No evidence was found of publication bias by Begg's test (P=0.88). Egger's test indicated a marginally significant probability of bias (P=0.07).
Eleven studies included only transplant patients8,9,11,14,15,19–23,25; subgroup analysis produced similar results, although with decreased statistical significance (RR 0.44, 95% CI 0.19 to 1.02, P=0.06; RD -0.01, 95% CI -0.02 to 0.00, P=0.12). Eight studies included nontransplant patients7,10,12,13,18,24,26,27; subgroup analysis produced similar results, although with decreased statistical significance (RR 0.47, 95% CI 0.19 to 1.13, P=0.09; RD -0.02, 95% CI -0.05 to 0.00, P=0.08).
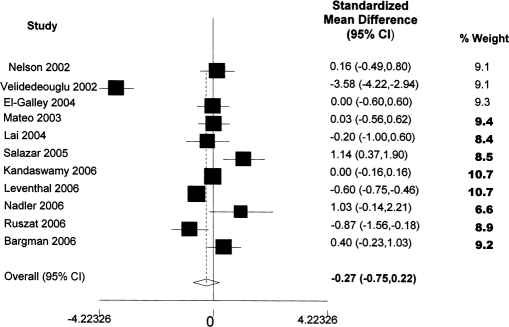
Hospital Length of Stay
Eleven studies (N=1787) evaluated hospital length of stay.6–11,14–16,23,25 No significant between-group differences were found in hospital length of stay. (SMD -0.27, 95% CI -0.75 to 0.22, P=0.28) (Figure 5).
Figure 5.
Eleven studies (n = 1787 patients) comparing length of stay for hand-assisted and pure laparoscopic nephrectomy. The diamond represents pooled SMD with 95% confidence limits for all studies; the squares and horizontal lines represent individual studies with 95% confidence limits.
Sequential omission of each study from the analysis, one study at a time, resulted in only nonsignificant changes in the magnitude or precision of the effect estimates (data not shown). No evidence was found of publication bias according to Begg's test (P=0.87) or Egger's test (P=0.86).
Nine studies included only transplant patients6,8,9,11,14–16,23,25; subgroup analysis showed similar, nonsignificant results (SMD -0.41, 95% CI -0.95 to 0.12, P=0.13). Two studies included nontransplant patients7,10; subgroup analysis also showed no significant difference between groups (SMD 0.45, 95% CI -0.36 to 1.26, P=0.27).
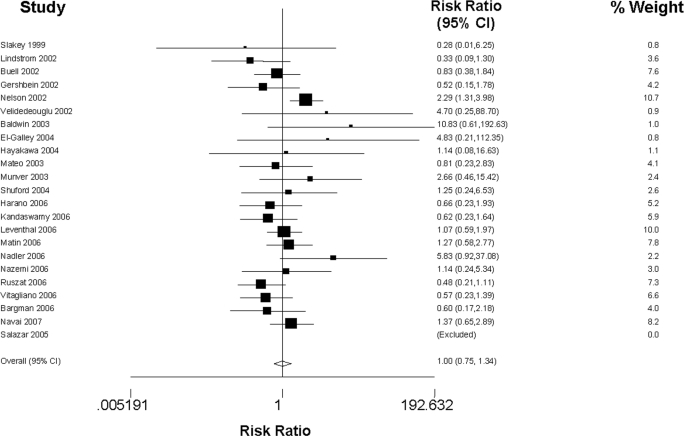
Perioperative Complication
Twenty-three studies (n=2999) evaluated complications.6–13,15–17,19–30 There were no significant between-group differences in overall risk (RR 1.00, 95% CI 0.75 to 1.34, P=0.99) (Figure 6) or incidence (RD 0.01, 95% CI -0.02 to 0.05, P=0.50) of perioperative complication.
Figure 6.
Twenty-three studies (n = 2999 patients) comparing risk of complication in hand-assisted and pure laparoscopic nephrectomy. The diamond represents pooled RR with 95% confidence limits for all studies; the squares and horizontal lines represent individual studies and their 95% confidence limits.
Sequential omission of each study from the analysis, one study at a time, resulted in only nonsignificant changes in the magnitude or precision of the effect estimates (data not shown). No evidence was found of publication bias according to Begg's test (P=0.96) or Egger's test (P=0.12).
Fourteen studies included only transplant patients.6,8,9,11,15,16,19–23,25,28,29 Subgroup produced similar results; although there was a marginally significant trend for decreased risk of complications for the hand-assisted group (RR 0.76, 95% CI 0.56 to 1.03, P=0.08) there was no significant difference for incidence (RD -0.002, 95% CI -0.03 to 0.02, P=0.87). Nine studies included nontransplant patients7,10,12,13,17,24,26,27,30; subgroup analysis produced similar results (RR 0.88, 95% CI 0.50 to 1.55, P=0.65; RD -0.02, 95% CI -0.04 to 0.004, P=0.11).
DISCUSSION
Clayman et al31 first reported laparoscopic nephrectomy in 1991 and Bannenberg et al32 first described the hand-assisted technique in the porcine model in 1996. Advocates of the hand-assisted approach cite the potentially steep learning curve and loss of tactile sensation involved with pure laparoscopy, asserting that a hand port allows surgeons better tactile sense, manipulative ability, and confidence. These factors, they argue, enhance performance of the operation with respect to identification of anatomic structures, dissection of the upper pole and hilum, improved vascular control, and decreased operative time.33 Advocates of pure laparoscopy, in turn, argue that hand ports are unnecessary for experienced laparoscopic surgeons and costly and that standard laparoscopy results in a smaller incision, decreased postoperative pain, and shorter convalescence.
In this analysis, hand-assisted laparoscopic nephrectomy was associated with significantly less operative blood loss and a decreased risk of conversion compared with pure laparoscopic nephrectomy. There were no differences with respect to operative time or risks of perioperative transfusion or complication.
These results suggest that the pure and hand-assisted techniques result in generally similar perioperative outcomes. Although the lower operative blood loss and decreased risk of conversion favor the hand-assisted approach, these findings are of uncertain clinical significance. For operative blood loss, we applied the standardized mean difference method to account for potential interstudy variations in data collection. Because standardized mean differences are expressed in units of standard deviation,34 these results are expressed in standard deviation units rather than volume units, which potentially limits the clinical relevance of this finding. Notably, there were no significant differences in transfusion between groups, suggesting that the diminished blood loss was not clinically significant.
Likewise, conversion is a problematic outcome measure to interpret in laparoscopic surgery because it generally fails to reveal the underlying reasons for—and clinical relevance of—the conversion. In addition, patient selection biases may influence study outcomes. Conversion from the laparoscopic approach to the open approach may result from a technically challenging procedure, failure to progress, or a catastrophic event such as a major vascular injury. Still, one possible explanation for the decreased risk of conversion with hand assistance is that increased tactile sensation and ability to manipulate tissues associated with the hand port may facilitate the performance of challenging cases. Mateo et al,9 for example, evaluated the conversion risk for high-risk (age>60, BMI>30 kg/m2, multiple vessels, right kidney donors, or refusal to accept transfusions) laparoscopic donor nephrectomy and noted a significantly higher conversion rate in pure compared with hand-assisted laparoscopy (13.8% vs 5.5%, respectively).
In this analysis, there was no difference in operative time between groups. At least 3 explanations are possible. First, several of the studies included in our analysis were cohorts in which the investigators had initially gained familiarity with hand assistance prior to performing pure laparoscopy; perhaps there exists an initial benefit to hand assistance that wanes as familiarity with laparoscopy increases. Second, even if the hand port reduces the time it takes to perform the nephrectomy, total operative time may be similar to pure laparoscopy because of the increased time required for hand port placement. Third, systematic bias may have been introduced in that only the more challenging cases were specifically selected to be performed with the hand-assisted technique.
Subgroup analysis, however, revealed that there was a statistically significant difference demonstrating decreased operative time for hand-assisted laparoscopy performed for nontransplant purposes. It may be that hand assistance plays a significant role in decreasing operative time when complex renal pathology is encountered, such as with renal neoplasm. Renal tumors often have neovascularity, irregular contours, and local inflammatory response, and it may be that only in these instances the additional benefit of using tactile sensation is fully realized. However, given the small group (2 studies, n=51 patients), the clinical significance is uncertain.7,10
Our results also indicate no significant difference in the overall length of hospitalization or complication rates with these 2 techniques. Complication rates are a problematic outcome to assess in this type of analysis because of the varied definitions of complication.
Our metaanalysis is novel in that it represents the first pooled analysis of data comparing different laparoscopic approaches with nephrectomy. We focused on transperitoneal nephrectomy, rather than retroperitoneal nephrectomy, for 2 interrelated reasons: first, the transperitoneal method is more common; second, substantially more published data are available on the transperitoneal method. Although randomized clinical trials are considered the gold standard for clinical research, our results provide the best available summary of evidence-based outcomes data and thus a potentially important source of information for treatment planning. The cohort studies included in this metaanalysis examined outcomes differences among largely nonrandomized patients and thus were subject to confounding by selection biases, which in turn may have influenced the results.
One potential limitation of metaanalysis is publication bias, though we did not find any evidence of significant publication bias in this analysis. Other limitations of meta-analysis include results dependent on the methodological quality of component trials, inclusion criteria bias, and outcome.
A potential source of heterogeneity was indication for nephrectomy, which we attempted to address with subgroup analyses. It may be that with the smaller number of nephrectomies performed for nontransplant indications, this study was underpowered to detect significant differences in the nontransplant group. Additional heterogeneity may have been introduced by intersurgeon and inter-institutional variations in technique, differences in outcome assessment, and differences in patient selection criteria.
CONCLUSION
Compared with pure laparoscopic nephrectomy, the hand-assisted technique was associated with significantly less operative blood loss; however, the clinical significance of these findings is unclear as there was no significant difference in transfusion rates. Additionally, the hand-assist technique had fewer conversions to open nephrectomy; however, the reasons for this difference cannot be fully elucidated in a metaanalysis. Operative time, hospital length of stay, and perioperative complication demonstrated no significant differences in our analysis, suggesting that the pure and hand-assisted techniques result in similar perioperative outcomes.
References:
- 1.Nanidis TG, Antcliffe D, Kokkinos C, et al. Laparoscopic versus open live donor nephrectomy in renal transplantation: a meta-analysis. Ann Surg. 2008;247:58–70 [DOI] [PubMed] [Google Scholar]
- 2.Portis AJ, Clayman RV. Should laparoscopy be the standard approach used for radical nephrectomy? Curr Urol Rep. 2001;2:165–170 [DOI] [PubMed] [Google Scholar]
- 3.Buell JF, Lee L, Martin JE, et al. Laparoscopic donor nephrectomy vs. open live donor nephrectomy: a quality of life and functional study. Clin Transplant. 2005;19:102–109 [DOI] [PubMed] [Google Scholar]
- 4.Wolf JS. Basic laparoscopy: hand-assisted techniques. In Smith AD, Badlani GH, Bagley DH, et al., eds. Smith's Textbook of Endourology. 2nd ed St. Louis, MO: Quality Medical Publications; 2006;415–421 [Google Scholar]
- 5.Lowry PS, Nakada SY. Hand-assisted laparoscopic radical nephrectomy. J Endourol. 2004;18:337–344 [DOI] [PubMed] [Google Scholar]
- 6.Bargman V, Sundaram CP, Bernie J, Goggins W. Randomized trial of laparoscopic donor nephrectomy with and without hand assistance. J Endourol. 2006;20:717–722 [DOI] [PubMed] [Google Scholar]
- 7.Nelson CP, Wolf JS., Jr Comparison of hand assisted versus standard laparoscopic radical nephrectomy for suspected renal cell carcinoma. J Urol. 2002;167:1989–1994 [PubMed] [Google Scholar]
- 8.El-Galley R, Hood N, Young CJ, Deierhoi M, Urban DA. Donor nephrectomy: a comparison of techniques and results of open, hand assisted and full laparoscopic nephrectomy. J Urol. 2004;171:40–43 [DOI] [PubMed] [Google Scholar]
- 9.Mateo RB, Sher L, Jabbour N, et al. Comparison of outcomes in noncomplicated and in higher-risk donors after standard versus hand-assisted laparoscopic nephrectomy. Am Surg. 2003;69:771–778 [PubMed] [Google Scholar]
- 10.Nadler RB, Loeb S, Clemens JQ, Batler RA, Gonzalez CM, Vardi IY. A prospective study of laparoscopic radical nephrectomy for T1 tumors—is transperitoneal, retroperitoneal or hand assisted the best approach? J Urol. 2006;175:1230–1234 [DOI] [PubMed] [Google Scholar]
- 11.Ruszat R, Sulser T, Dickenmann M, et al. Retroperitoneoscopic donor nephrectomy: donor outcome and complication rate in comparison with three different techniques. World J Urol. 2006;24:113–117 [DOI] [PubMed] [Google Scholar]
- 12.Baldwin DD, Dunbar JA, Parekh DJ, et al. Single-center comparison of purely laparoscopic, hand-assisted laparoscopic, and open radical nephrectomy in patients at high anesthetic risk. J Endourol. 2003;17:161–167 [DOI] [PubMed] [Google Scholar]
- 13.Shuford MD, McDougall EM, Chang SS, LaFleur BJ, Smith JA, Jr., Cookson MS. Complications of contemporary radical nephrectomy: comparison of open vs. laparoscopic approach. Urol Oncol. 2004;22:121–126 [DOI] [PubMed] [Google Scholar]
- 14.Lai IR, Tsai MK, Lee PH. Hand-assisted versus total laparoscopic live donor nephrectomy. J Formos Med Assoc. 2004;103:749–753 [PubMed] [Google Scholar]
- 15.Salazar A, Pelletier R, Yilmaz S, et al. Use of a minimally invasive donor nephrectomy program to select technique for live donor nephrectomy. Am J Surg. 2005;189:558–563 [DOI] [PubMed] [Google Scholar]
- 16.Kandaswamy R, Casingal V, Sturdevent M, et al. Laparoscopic donor nephrectomy (LDN): robotic-assisted (RALDN) vs pure (PLDN) vs hand-assisted (HALDN) [abstract]. Am J Transplant. 2006;6(suppl 2):796–797 Abstract 2209 [Google Scholar]
- 17.Nazemi T, Galich A, Sterrett S, Klingler D, Smith L, Balaji KC. Radical nephrectomy performed by open, laparoscopy with or without hand-assistance or robotic methods by the same surgeon produces comparable perioperative results. Int Braz J Urol. 2006;32:15–22 [DOI] [PubMed] [Google Scholar]
- 18.Kijvikai K, Maynes LJ, Cookson M, et al. Laparoscopic, hand assisted laparoscopic and open simple nephrectomy for technically challenging cases [abstract]. J Urol. 2007;177(4 suppl):234 Abstract 698 [Google Scholar]
- 19.Slakey DP, Wood JC, Hender D, Thomas R, Cheng S. Laparoscopic living donor nephrectomy: advantages of the hand-assisted method. Transplantation. 1999;68:581–583 [DOI] [PubMed] [Google Scholar]
- 20.Lindstrom P, Haggman M, Wadstrom J. Hand-assisted laparoscopic surgery (HALS) for live donor nephrectomy is more time- and cost-effective than standard laparoscopic nephrectomy. Surg Endosc. 2002;16:422–425 [DOI] [PubMed] [Google Scholar]
- 21.Buell JF, Koffron A, Hanaway MJ, Potter SR, Leventhal J, Woodle ES. Comparision of hand-assisted and traditional laparoscopic live donor nephrectomy: a superior method or surgeons preference [abstract]. Am J Transplant. 2002;2 (suppl):415 Abstract 1102 [Google Scholar]
- 22.Gershbein AB, Fuchs GJ. Hand-assisted and conventional laparoscopic live donor nephrectomy: a comparison of two contemporary techniques. J Endourol. 2002;16:509–513 [DOI] [PubMed] [Google Scholar]
- 23.Velidedeoglu E, Williams N, Brayman KL, et al. Comparison of open, laparoscopic, and hand-assisted approaches to live-donor nephrectomy. Transplantation. 2002;74:169–172 [DOI] [PubMed] [Google Scholar]
- 24.Hayakawa K, Aoyagi T, Ohashi M, Hata M. Comparison of Gas-less laparoscopy-assisted surgery, hand-assisted laparoscopic surgery and pure laparoscopic surgery for radical nephrectomy. Int J Urol. 2004;11:142–147 [DOI] [PubMed] [Google Scholar]
- 25.Leventhal JR, Baler TB, Kocak B, Koffron AJ. Hand assisted or “pure” laparoscopic donor nephrectomy? Single center retrospective experience of 800 cases [abstract]. Am J Transplant. 2006;6 (2 suppl):794 Abstract 2200 [Google Scholar]
- 26.Matin SF, Dhanani N, Acosta M, Wood CG. Conventional and hand-assisted laparoscopic radical nephrectomy: comparative analysis of 271 cases. J Endourol. 2006;20:891–894 [DOI] [PubMed] [Google Scholar]
- 27.Vitagliano G, Castillo O, Kerkebe M, et al. Laparoscopic radical nephrectomy: a comparison between hand-assisted and pure laparoscopic surgery [abstract]. J Endourol. 2006;20(suppl):A59 Abstract VP10–09 [Google Scholar]
- 28.Munver R, Sosa RE, Del Pizzo JJ. Hand-assisted laparoscopy facilitates a smooth transition from open to laparoscopic live donor nephrectomy: 6-year experience at single institution [abstract]. J Urol. 2003;169(4 suppl):484–485 Abstract 1814 [Google Scholar]
- 29.Harano M, Eto M, Yokomizo A, Tatsugami K, Hamaguchi M, Naito S. Laparoscopic radical nephrectomy for renal cancer: a comparison of the hand assisted procedure vs. the standard procedure in a single institute [abstract]. J Endourol. 2006;20(suppl):A205 Abstract MP16–20 [Google Scholar]
- 30.Navai N, Lee CZ, Okotie O, et al. Comparison of surgical outcomes between pure and hand-assisted laparoscopic radical nephrectomy [abstract]. J Urol. 2007;177(4 suppl):235 Abstract 699 [Google Scholar]
- 31.Clayman RV, Kavoussi LR, Soper NJ, et al. Laparoscopic nephrectomy. N Engl J Med. 1991;324:1370–1371 [DOI] [PubMed] [Google Scholar]
- 32.Bannenberg JJG, Meijer DW, Bannenberg JH, Hodde KC. Hand-assisted laparoscopic nephrectomy in the pig: initial report. Minim Invasive Ther Allied Technol. 1996;5:483 [Google Scholar]
- 33.Wolf JS, Jr., Moon TD, Nakada SY. Hand assisted laparoscopic nephrectomy: comparison to standard laparoscopic nephrectomy. J Urol. 1998;160:22–27 [PubMed] [Google Scholar]
- 34.Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In Egger M, Smith GD, Altman DG. Systematic Reviews in Health Care: Meta-analysis in Context. London, UK: BMJ Publishing Group; 2001;285–312 [Google Scholar]