Abstract
Appendiceal inversion is an uncommon entity that presents a diagnostic dilemma for the gastroenterologist or surgeon. We present 2 cases that illustrate scenarios that may be encountered during colonoscopy. A discussion of the literature on this subject is also presented. An improved awareness of this condition will assist the endoscopist in the identification of this finding and direct the appropriate expectant management.
Keywords: Appendix, Colonoscopy, Appendiceal neoplasm
INTRODUCTION
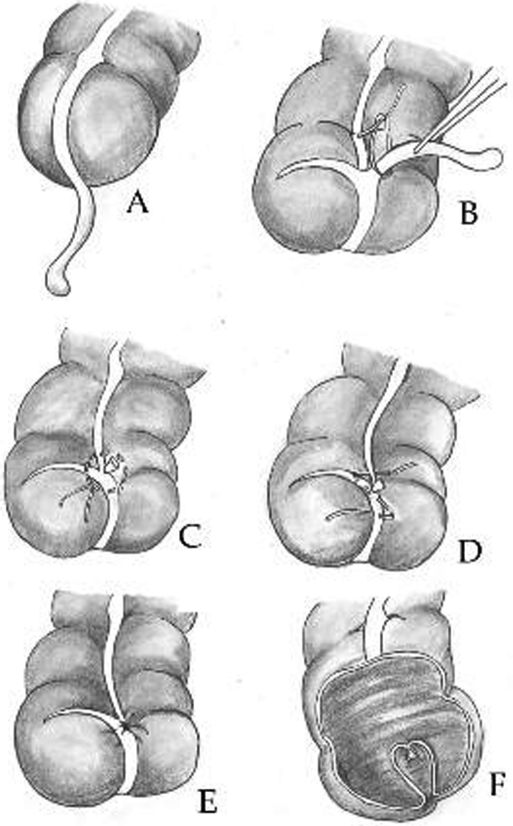
Discovery of appendiceal inversion during colonoscopy is relatively unusual. This finding is often mistaken for other pathologic processes. Whether as a result of intussusception,1 “dunking” during routine appendectomy (Figure 1), or even as a described technique to perform an appendectomy without transection,2 the end result remains the same—additional tissue in the cecal base. Unfortunately, these lesions mimic a neoplastic process both radiologically and endoscopically, and even routine biopsy or attempted “polypectomy” may result in perforation or bleeding requiring urgent surgical exploration. We describe 2 cases of appendiceal inversion found during colonoscopy, and review the potential causes, clinical manifestations, and treatment options.
Figure 1.
Appendiceal inversion procedure. After the base of the appendix (A) is ligated (B) and cut, a seromuscular purse-string suture (C) or a “Z” stitch (D) is placed around the stump. The appendiceal stump is then buried and the suture is tied (E). When the stump is inverted in the lumen of the intestine, it appears as a polypoid lesion entirely covered by mucosa (F).
CASE REPORTS
Case 1
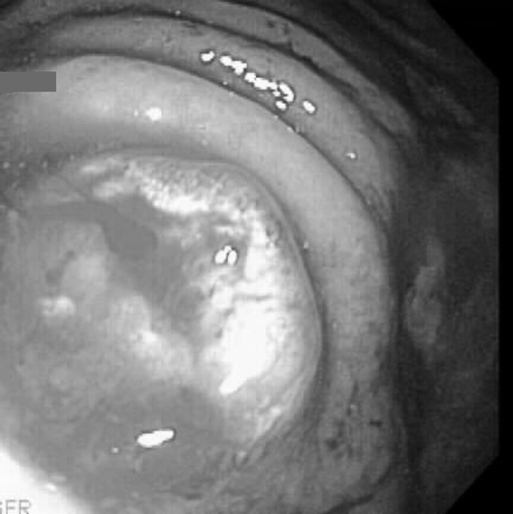
A fifty-year-old female was referred to our service after the discovery on colonoscopy of a 1-cm pedunculated polyp arising from the appendiceal orifice. The patient had a history of previous appendectomy and was undergoing the colonoscopy as a screening procedure. She had a family history of colon cancer. The gastroenterologist was uncomfortable performing a polypectomy, and the patient was referred for possible colectomy. After further discussion, the patient elected to undergo a second attempt at colonoscopy with possible polypectomy. The polypoid lesion was visualized and did look suspiciously like an adenoma (Figure 2). A snare polypectomy was performed after submucosal injection of saline at the polyp's base. It was clear that the entire polyp stalk was not removed during the procedure (Figure 3). The stalk was cauterized, and the 1-cm specimen was sent for pathologic examination. The patient did well after the colonoscopy and returned for follow-up without complications. The pathology tests revealed that the specimen was consistent with an inverted appendiceal stump.
Figure 2.
Endoscopic photograph depicting the polypoid appearance of the appendiceal orifice.
Figure 3.
Endoscopic photograph depicting the remaining “stalk” after attempted snare polypectomy.
Case 2
Our second case is that of a 52-year-old male with a 1.2-cm polyp arising from the appendiceal orifice and discovered during routine colonoscopy. The patient had a history of appendectomy in the 1970s. He underwent a snare polypectomy without complication.
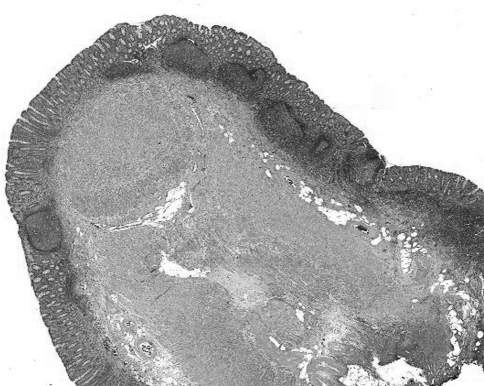
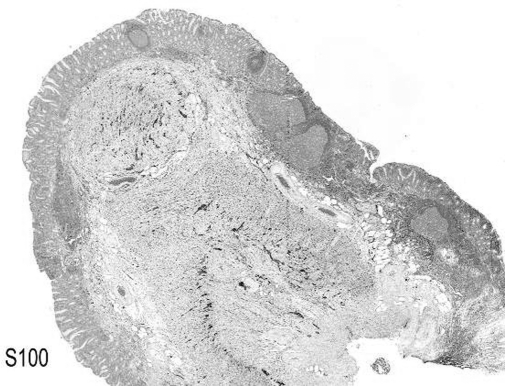
Histopathologic examination of both cases revealed the reversed pattern of the normal appendix (Figure 4). The surface was lined by normal colonic type mucosa with prominent lymphoid follicles. The underlying muscularis propria was disorganized and hypertrophic with a prominent neurogenic component (Figure 5). Fibrosis and intervening adipose tissue were seen at the center.
Figure 4.
Inverted appendiceal stump lined by colonic type mucosa with prominent lymphoid follicles. The underlying muscularis propria appears hypertrophic. (hematoxylin-eosin, original magnification ×20).
Figure 5.
Prominent neurogenic component highlighted by anti S-100. (Immunohistochemistry using anti-S-100, original magnification ×20).
Neither of the above patients had symptoms attributable to carcinoma. Both colonoscopies were performed as screening procedures.
DISCUSSION
Polypoid lesions involving the appendiceal lumen and orifice can be problematic. They can be difficult to remove completely using endoscopic techniques. This is compounded by the increased risk of perforating the adjacent thin-walled cecum. Previous reports address the concern for incomplete removal of these lesions. Less than 250 reports are available in the literature describing invasive adenocarcinoma or adenocarcinoma in situ arising from these uncommon lesions.3–5 Other reports describe appendiceal endometriosis, juvenile polyps, adenomatous polyps, and simple appendiceal inversion.6–11 Despite the low incidence of these lesions, the available evidence suggests they cannot be ignored and should not be managed like colonic polyps.
Several reports in the literature describe appendiceal inversion as having an appearance similar to that of a neoplastic polyp.8–10 This is seen in patients who have undergone previous appendectomy and patients who have appendiceal intussusception. Intussusception of the appendix is rare in the general population, but it is reported to occur more frequently in patients with cystic fibrosis.8 Patients who have undergone appendectomy via the ligation-inversion method appear to be more likely to have an abnormal-appearing appendiceal orifice endoscopically.12,13 This is not unexpected and is more likely to occur when a long appendiceal stump is left behind.
An appendiceal inversion may appear on endoscopy to be a polypoid area covered with normal mucosa or with granulation tissue. It may also resemble an adenomatous polyp. Two recent reports describe 3 cases of visualization of an inverted appendiceal stump on CT colonography.9,10 Both centers describe having difficulty differentiating the stump from an adenomatous polyp. In all 3 cases, patients went on to have a completion colonoscopy, and the diagnosis was made by gross findings and simple biopsy in 2 patients and “polypectomy” in 1 patient. A subsequent letter to the editor written to comment on one of the reports pointed out that evaluation of 2D colonographic images can provide additional information on the makeup of a polyp.14 The author stated that true polyps have a typical radiographic appearance and that this can assist in their differentiation from lesions such as appendiceal inversion or lipomas.
The obvious dangers in performing a “polypectomy” of an appendiceal inversion are related to bleeding and perforation. In the case of a patient who has undergone previous appendectomy, the appendiceal lumen will in all likelihood be fibrosed. The risk of perforation would be theoretically low in this individual, although the true rate of this complication is unknown in this particular scenario. If the appendiceal lumen is patent, such as would be seen in someone with an appendiceal intussusception, then a leak from the polypectomy site would be likely. Bleeding would certainly be more likely to occur from division of an appendix with a patent blood supply. A simple biopsy, ensuring adequate sampling, combined with evaluation of gross findings seems to be the most appropriate approach to ensure that neoplasia is not being overlooked in these uncommon encounters. It is important to note, however, that a simple biopsy is helpful in the assessment of dysplasia or malignancy at the site of the biopsy, but it may not be fully diagnostic of an appendiceal stump because both appendix and colon have a similar mucosal lining. If one combines this evaluation with CT colonography, then it is unlikely that any neoplasia will be missed. In a situation where the diagnosis of appendiceal inversion cannot be confirmed or refuted, and neoplasia is a concern, then a formal resection would seem to be the best alternative given the previously documented nature of appendiceal adenomas.
CONCLUSION
Inversion of the appendiceal base is an expected occurrence after inversion-ligation appendectomy. This procedure is being performed less commonly today with the advent of laparoscopic appendectomy. Appendiceal inversion can occur after appendectomy by any method. Endoscopists should be aware of this entity as well as its endoscopic appearance. It should also be noted that this finding may be encountered in barium enema and contrast computed tomographic investigations. Improved awareness of this finding may lead to the avoidance of unnecessary interventions.
Footnotes
No competing interests declared. The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Defense. Use of commercial products in this project does not imply endorsement by the US Government.
Contributor Information
Eric K. Johnson, Department of Colorectal Surgery, Eisenhower Army Medical Center, Ft. Gordon, Georgia..
Maria E. Arcila, Department of Pathology, Eisenhower Army Medical Center, Ft. Gordon, Georgia..
Scott R. Steele, Department of Colorectal Surgery, Madigan Army Medical Center, Ft. Lewis, Washington..
References:
- 1.Jevon GP, Daya D, Oizilbash AH. Intussusception of the appendix. A report of four cases and review of the literature. Arch Pathol Lab Med. 1992;116(9):960–964 [PubMed] [Google Scholar]
- 2.Voeller GR, Fabian TC. Inversion-ligation appendectomy for incidental appendectomy. Am J Surg. 1991;161(4):483–484 [DOI] [PubMed] [Google Scholar]
- 3.Van Fleet RH, Shabot JM, Halpert RD. Adenocarcinoma of the appendiceal stump. South Med J. 1990;83:1351–1353 [DOI] [PubMed] [Google Scholar]
- 4.Shami VM, Yerian LM, Waxman I. Adenoma and early stage adenocarcinoma of the appendix: diagnosis by colonoscopy. Gastrointest Endosc. 2004;59:731–733 [DOI] [PubMed] [Google Scholar]
- 5.Hardin RD. Colonoscopic diagnosis of an appendiceal polyp with carcinoma in situ. J Clin Gastroenterol. 1986;8:189–191 [DOI] [PubMed] [Google Scholar]
- 6.Langsam LB, Raj PK, Galang GF. Intussusception of the appendix. Dis Colon Rectum. 1984;27:387–392 [DOI] [PubMed] [Google Scholar]
- 7.Weinstock LB, Shatz BA, Swanson PE, et al. Juvenile polyp emerging from the appendiceal orifice. Gastrointest Endosc. 1999;49:759. [DOI] [PubMed] [Google Scholar]
- 8.Ram AD, Peckham C, Akobeng AK, et al. Inverted appendix mistaken for a polyp during colonoscopy and leading to intussusception. J Cyst Fibros. 2005;4:203–204 [DOI] [PubMed] [Google Scholar]
- 9.Koff JM, Choi JR, Hwang I. Inverted appendiceal orifice masquerading as a cecal polyp on virtual colonoscopy. Gastrointest Endosc. 2005;62:308. [DOI] [PubMed] [Google Scholar]
- 10.Prout TM, Taylor AJ, Pickhardt PJ. Inverted appendiceal stumps simulating large pedunculated polyps on screening CT colonography. Am J Roentgenol. 2006;186:535–538 [DOI] [PubMed] [Google Scholar]
- 11.Taban S, Dema A, Lazar D, et al. An unusual tumor of the cecum: the inverted appendiceal stump. Rom J Morphol Embryol. 2006;47:193–196 [PubMed] [Google Scholar]
- 12.Engstrom L, Fenyo G. Appendicectomy: assessment of stump invagination versus simple ligation: a prospective, randomized trial. Br J Surg. 1985;72:971–972 [DOI] [PubMed] [Google Scholar]
- 13.Jarvensivu P, Lehtola J, Karvonen AL, et al. Colonoscopic appearance of the remnant of the appendix after total inversion. Endoscopy. 1982;14:66–68 [DOI] [PubMed] [Google Scholar]
- 14.Gollub MJ. Letter to the Editor. Inverted appendiceal orifice masquerading as a cecal polyp on virtual colonoscopy. Gastrointest Endosc. 2006;63:358. [DOI] [PubMed] [Google Scholar]