Abstract
Cornual pregnancy often poses a diagnostic and therapeutic challenge, with a significant risk for morbidity and mortality. Traditional treatment for cornual pregnancy has been through laparotomy, wedge resection, or hysterectomy. Early diagnosis is now possible through transvaginal ultrasonography and highly-sensitive β-human chorionic gonadotropin assays. Consequently, several less-invasive therapies and techniques have been introduced over the last 2 decades. We present a simple, stepwise laparoscopic technique for the definitive, minimally-invasive excision of cornual pregnancy, along with a review of the pertinent literature.
Keywords: Cornual pregnancy, Interstitial pregnancy, β-human chorionic gonadotropin, Hysterectomy, Laparoscopy, Laparotomy
INTRODUCTION
Laparotomy with cornual wedge resection or hysterectomy has been the traditional treatment for the rare cases of cornual pregnancy.1 In the last 2 decades, several reports have been published of minimally-invasive surgical techniques used to successfully treat cornual ectopic pregnancies. Consistent with the goals of minimally-invasive surgery, these techniques have introduced a surgical alternative with reduced blood loss, less postoperative pain, shorter hospital stay, and a more expeditious recovery. In this report, we describe a simple, stepwise laparoscopic technique used successfully for the management of two patients with large cornual pregnancies, along with a review of risks, benefits, and the pertinent literature.
CASE REPORT
Carol was a 28-year-old, African American female, gravida 3, para 2 at 8-weeks gestation based on her last menstrual period. She originally presented to the emergency department complaining of intermittent vaginal bleeding for 24 hours. She denied pain or the passage of tissue. Her medical history was significant for morbid obesity, pseudotumor cerebri, sagittal sinus thrombosis, and asthma complicated by a previous lung collapse requiring intubation. Her obstetric history revealed one uncomplicated, full-term pregnancy with a normal vaginal delivery. Her second pregnancy was complicated by cervical incompetence requiring rescue cerclage placement, but ended successfully with a normal vaginal delivery at term. The patient reported no plans for future pregnancies and that this was an undesired pregnancy.
Her physical examination on presentation showed stable vital signs, a benign abdominal and pelvic examination with minimal old blood in the vaginal vault. The cervix was closed, and no cervical motion tenderness was noted.
Abdominal and transvaginal ultrasounds revealed an eccentric gestational sac, 2.7 cm x 2.5 cm, located in the right uterine fundus with a thin myometrial mantle measuring 3.5 mm in thickness, consistent with an interstitial tubal pregnancy. The embryo had a crown-rump length of 7.7 mm, with no cardiac activity. No free fluid was noted within the pelvis.
METHODS
After much discussion and counseling regarding treatment options including the limited data on the risk of uterine rupture with future pregnancy, the decision was made to proceed with laparoscopic surgical excision. During the course of these discussions, the patient received one dose of intramuscular methotrexate with planned outpatient management, but she was then brought back to the hospital on day 3 for definitive surgical management, as the consensus among the providers was that definitive surgical treatment was more prudent.
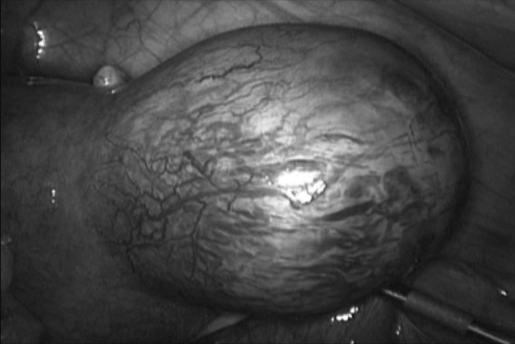
Operative laparoscopy was performed under general anesthesia. An intact 6 cm x 4 cm right cornual pregnancy with a thinned-out hyperemic myometrial capsule was noted (Figure 1). The remainder of the pelvic structures appeared normal.
Figure 1.
Right Cornual Pregnancy (6x4 cm).
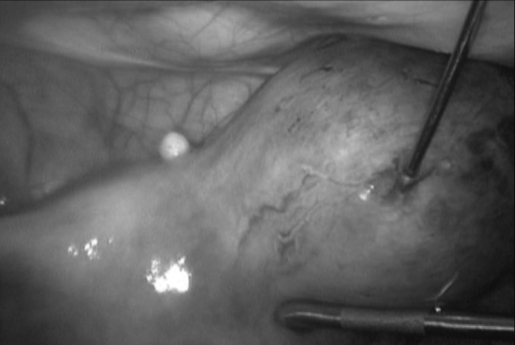
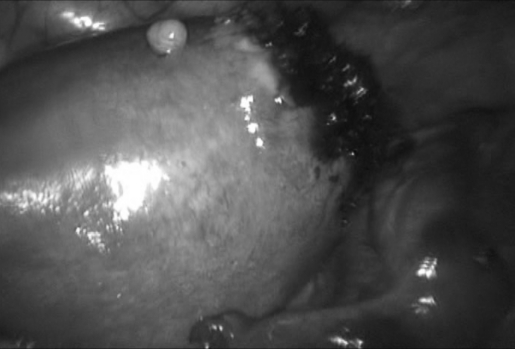
A simple stepwise technique of laparoscopic excision of the cornual pregnancy was performed. Dilute vasopressin (10 IU in 100 mL of normal saline) was prepared, and a total of 46 mL was injected throughout the cornual pregnancy by using a long 20-gauge spinal needle, introduced directly through the anterior abdominal wall in the midline under direct visualization with the laparoscope. Complete blanching of the cornual pregnancy was achieved (Figure 2). A linear incision was made with monopolar cautery in the thin myometrial capsule, along the long axis of the cornual pregnancy. A well-formed gestational sac was clearly identified and expressed from the cornua using blunt, sharp and hydro-dissection (Figure 3). A large, very thin capsule (mantle) overlying the myometrium that had previously housed the ectopic pregnancy was noted and excised at the base in an elliptical fashion, with bipolar cautery and scissors. Significant myometrial thickness was still maintained at the base of the cornua, and no gross myometrial defect was noted. The remaining myometrial bed at the right cornua was judiciously cauterized to obtain excellent hemostasis (Figure 4). The specimen was retrieved from the pelvis with the 10-mm Autosuture Endo Catch (US Surgical, Norwalk, CT) and sent to pathology where the diagnosis of an ectopic pregnancy was confirmed.
Figure 2.
A spinal needle introduced directly through the abdominal wall. Complete blanching achieved with dilute vasopressin.
Figure 3.
A linear incision along the capsule of the cornual pregnancy has been made after complete blanching with vasopressin.
Figure 4.
Only a minimal portion of the right cornua has been removed (minicornual excision) with complete excision of the ectopic gestation.
RESULTS
A large cornual pregnancy was successfully treated with a simple, definitive laparoscopic technique. The patient tolerated the procedure well with a total operative time of 2 hours and estimated blood loss of 50 mL. The patient was discharged home on postoperative day 1. The patient's quantitative β-hCG was closely followed until it returned to essentially zero (Table 1).
Table 1.
Quantitative β-HCG
| Date | Quantitative β-HCG | Treatment |
|---|---|---|
| 08/08/07 | 5423 IU/L | I.M. Methotrexate |
| 08/11/07 | 5172 IU/L | Laparoscopic excision |
| 08/20/07 | 10 IU/L | |
| 08/27/07 | <2 IU/L |
β-HCG = Beta Human Chorionic Gonadotropin.
DISCUSSION
Traditionally, cornual ectopic gestations have been treated with exploratory laparotomy and wedge resection of the uterine cornua or even hysterectomy.1 With the advent of minimally-invasive techniques and the growing evidence and expertise in the field, laparoscopic mini-cornual excision offers a valuable option for patients desiring definitive minimally-invasive surgical treatment of cornual ectopic pregnancy. Because patient safety is always the prime goal, mini-cornual excision for cornual pregnancies should only be recommended to hemodynamically stable patients in a tertiary care facility with the necessary laparoscopic skills and expertise to ensure patient safety. The availability of blood products, immediate anesthesia, and critical care staff, and surgical equipment and facilities are also essential for the safe practice of this minimally-invasive procedure. With these conditions and appropriate patient selection, laparoscopic treatment of interstitial pregnancy offers significant advantages over laparotomy, such as short hospital stay, faster return to normal activities, and decreased health care cost,2 without compromising treatment or patient safety.
As illustrated in this case series, we advocate a simple method of a stepwise, minimally-invasive treatment of cornual ectopic pregnancies. Several reports over the last 2 decades have illustrated various techniques for treatment of cornual pregnancy, including methotrexate injection,3–5 cornuostomy,6 salpingostomy,7 and the use of EndoLoop (Ethicon, Cincinnati, Ohio) for small cornual pregnancies.5,8,9 Several reports have also indicated the need for ligation of the ascending branches of the uterine arteries or mesosalpingeal vessels to maintain hemostasis.1,10 Laparoscopic suturing has been applied in many reports to achieve hemostasis and aid healing.11,12 In contrast, several reports with successful outcomes have not used suturing.13–16 One can argue that suturing may decrease the risk of future uterine rupture, but at this time, evidence is minimal that either approach is superior.
In this stepwise technique of mini-cornual excision (Table 2), excellent hemostasis is adequately achieved with generous injection of dilute vasopressin along with judicious use of cautery to minimize tissue necrosis. No vascular ligation is utilized, maintaining adequate blood supply and avoiding the unnecessary tissue ischemia that potentially impairs healing and compromises the tensile strength of the cornual region, negatively impacting future pregnancies. In our technique, only a minute portion of the cornua is excised (the thin overlying myometrial capsule), preserving most of the integrity and architecture of the uterus and likely maintaining significant tensile strength at the surgical site. The vascular supply of the cornual region is also not compromised. Simply stated, the cornual pregnancy is “deroofed,” leaving the base intact.
Table 2.
Stepwise Approach for Mini-Cornual Excision
| 1 | Liberal Vasopressin injection (10 IU diluted in 100 ml of Saline) |
| 2 | Linear incision with Cautery over the cornual pregnancy, along the long axis of the tube |
| 3 | Evacuation and retrieval of the gestational sac and trophoblastic tissue using EndoCatch. |
| 4 | Cauterization of the base and remaining trophoblastic tissue. |
| 5 | Excision of the thin myometrial capsule on both sides near its connection to the uterine fundus. |
| 6 | Assure excellent hemostasis. Copious irrigation. Adhesion prevention measures |
Several important issues associated with mini-cornual excision must be addressed, including hemorrhage, chronic ectopic pregnancy, recurrent cornual pregnancy, and the care of future pregnancies.
Risk of hemorrhage remains the paramount concern for all clinicians caring for women with cornual ectopic pregnancies. Mini-cornual excision is not advisable in cases of ruptured cornual pregnancy due to the catastrophic hemorrhage and the associated hypovolemic shock commonly encountered in these cases. Expeditious laparotomy after initial resuscitation remains the mainstay in such cases. The same principle applies if uncontrollable hemorrhage is encountered during laparoscopic mini-cornual excision. However, several measures can be used preemptively to minimize this possibility, such as vasopressin and bipolar cautery in this case, and the use of endoloops5,8,9 prior to manipulation of the cornual pregnancy.
The potential for chronic ectopic pregnancy due to inadequate removal of the ectopic gestation is a rare but real concern. Non-excisional management options for cornual pregnancy, such as methotrexate, cornuostomy, salpingostomy, and including mini-cornual excision, all carry a small risk of incompletely removing the cornual gestation and the persistence of chorionic villi in the cornua. This is usually diagnosed by failure of serum hCG to drop to non-pregnant levels. The advantage that mini-cornual excision offers over other methods is that the cornual pregnancy is deroofed, providing easy access that facilitates complete removal of the gestational sac and chorionic villi, minimizing the risk of chronic cornual pregnancy. However, more studies are necessary to examine and compare this new technique with other non-excisional methods.
Recurrent cornual pregnancy remains a risk, similar to any surgical treatment for an ectopic gestation at any site. Conservative management of cornual pregnancy, i.e., without radical cornual resection, obviously carries a risk of recurrence at the same location. Patients should be carefully counseled about the associated risks of cornual pregnancy resection as well as the benefit of maintaining uterine integrity, vascularity, and structure, especially in patients desiring future fertility.
Risk to future pregnancies and the care of any subsequent pregnancies remain valid concerns after mini-cornual excision, particularly regarding the potential risk of uterine rupture. This concern originates from the potential risk of leaving a weakened cornual region following mini-cornual excision, allowing for potential uterine rupture with future gestations. In addition, excessive use of electrocautery may cause significant concealed damage to the myometrium that can further weaken the cornual region and increase the risk of uterine rupture with future pregnancies. Hence, the judicious use of cautery cannot be overemphasized. If a significant gap is created in the cornual region while evacuating the contents, the incision should be approximated with laparoscopic suturing, and, if not feasible, a minilaparotomy may be necessary. Further studies are required to determine the long-term outcome of this technique. These considerations should be clearly addressed when counseling patients regarding their management options and the risk of uterine rupture with future pregnancies.
With regards to the care of future pregnancies, all patients should be carefully counseled on the importance of early presentation with future pregnancies for complete evaluation, primarily to rule out a recurrent cornual or ectopic pregnancy, and also to establish reliable dates and timely delivery plans. Two case reports describe successful, uncomplicated vaginal delivery following laparoscopic management of cornual pregnancy.6,17 However, at this time, we recommend close monitoring of future pregnancies for patients treated conservatively for cornual pregnancy, with a planned cesarean delivery at term or upon failure of tocolytic therapy for preterm labor.
CONCLUSION
Cornual pregnancy is a potentially life-threatening condition that should be managed safely in a timely fashion. Definitive, minimally-invasive laparoscopic excision should be the standard of care. The stepwise approach presented here; mini-cornual excision, achieves a rapid, systematic, safe, and definitive treatment of cornual pregnancy that is minimally-invasive with minimal blood loss and rapid return to normal activities. Careful patient selection and counseling regarding treatment options is essential, particularly for patients desiring future pregnancy.
References:
- 1.Rock JA, Jones HQ., III TeLinde's Operative Gynecology, 9th edition Philadelphia, PA: Lippincott Williams and Wilkins; 2003; 527–528 [Google Scholar]
- 2.Baumann R, Magos AL, Turnbull A. Prospective comparison of videopelviscopy with laparotomy for ectopic pregnancy. Br J Obstet Gynecol. 1991;98:765–771 [DOI] [PubMed] [Google Scholar]
- 3.Lau S, Tulandi T. Conservative medical and surgical management of interstitial ectopic pregnancy. Fertil Steril. 1999;72:207–215 [DOI] [PubMed] [Google Scholar]
- 4.Lin Y, Chen C, Yuan C, et al. Successful rescue of an early interstitial pregnancy after failed systemic methotrexate treatment. J Reprod Med. 2007;52:332–334 [PubMed] [Google Scholar]
- 5.Soriano D, Vicus D, Mashiach R, Schiff E, Seidman D, Golden-beg M. Laparoscopic treatment of cornual pregnancy: a series of 20 consecutive cases. Fertil Steril. 2007. October 11 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Sagiv R, Golan A, Arbel-Alon S, et al. Three conservative approaches to treatment of interstitial pregnancy. J Am Assoc Gyn Lapososc. 2001;8:154–158 [DOI] [PubMed] [Google Scholar]
- 7.Pasic R, Wolfe WM. Laparoscopic diagnosis and treatment of interstitial ectopic pregnancy: a case report. Am J Obstet Gynecol. 1990;163:587–588 [DOI] [PubMed] [Google Scholar]
- 8.Moon HS, Choi Y, Park YH, et al. New simple endoscopic operations for interstitial pregnancies. Am J Obstet Gynecol. 2000;182:114–121 [DOI] [PubMed] [Google Scholar]
- 9.Hill GA, Segars JH, Herbert CA. Laparoscopic management of interstitial pregnancy. J Gynecol Surg. 1989;5:209–212 [Google Scholar]
- 10.Confino E, Gleicher N. Conservative surgical management of interstitial pregnancy. Fertil Steril. 1989;52:600–603 [DOI] [PubMed] [Google Scholar]
- 11.Grobman WA, Milad MP. Conservative laparoscopic management of a large cornual ectopic pregnancy. Hum Reprod. 1998;13:2002–2004 [DOI] [PubMed] [Google Scholar]
- 12.Coric M, Barisic D, Strelec M. Laparoscopic approach to interstitial pregnancy. Arch Gynecol Obstet. 2004;270:287–289 [DOI] [PubMed] [Google Scholar]
- 13.Laury D. Laparoscopic treatment of an interstitial pregnancy. J Am Assoc Gynecol Laparosc. 1995;2(2):219–221 [DOI] [PubMed] [Google Scholar]
- 14.Morita Y, Tsutsumi O, Momoeda M, et al. Cornual pregnancy successfully treated laparoscopically with fibrin glue hemostasis. Obstet Gynecol. 1997;90:685–687 [DOI] [PubMed] [Google Scholar]
- 15.Pasic RP, Hammons G, Gardner JS, et al. Laparoscopic treatment of cornual heterotopic pregnancy. J Am Assoc Gynecol Laparosc. 2002;9(3):372–375 [DOI] [PubMed] [Google Scholar]
- 16.Gezer A, Mutlu H. Laparoscopic management of cornual pregnancy without sutures. Arch Gynecol Obstet. 2004;270(3):194–196 [DOI] [PubMed] [Google Scholar]
- 17.Pansky M, Bukovsky I, Golan A, et al. Conservative management of interstitial pregnancy using operative laparoscopy. Surg Endosc. 1995;9:515–516 [DOI] [PubMed] [Google Scholar]