Abstract
Background/Objectives:
Despite multiple options for operative repair of parastomal hernia, results are frequently disappointing. We review our experience with parastomal hernia repair.
Methods:
A retrospective chart review was performed on all patients with parastomal hernia who underwent LAP or open repair at our institution between 1999 and 2006. Information collected included demographics, indication for stoma creation, operative time, length of stay, postoperative complications, and recurrence.
Results:
Twenty-five patients who underwent laparoscopic or open parastomal hernia repair were identified. Laparoscopic repair was attempted on 12 patients and successfully completed on 11. Thirteen patients underwent open repair. Operative time was 172±10.0 minutes for laparoscopic and 137±19.1 minutes for open cases (P=0.14). Lengths of stay were 3.1±0.4 days (laparoscopic) and 5.1±0.8 days (open), P=0.05. Immediate postoperative complications occurred in 4 laparoscopic patients (33.3%) and 2 open patients (15.4%), P=0.38. Parastomal hernia recurred in 4 laparoscopic patients (33.3%) and 7 open patients (53.8%) after 13.9±4.5 months and 21.4±4.3 months, respectively, P=0.43.
Conclusion:
Laparoscopic modified Sugarbaker technique in the repair of parastomal hernia affords an alternative to open repair for treating parastomal hernia.
Keywords: Laparoscopic parastomal hernia repair, Parastomal hernia repair, Parastomal hernia
INTRODUCTION
Parastomal hernia (PH) is a frequent complication following creation of colostomy and ileostomy. The development of PH does not always necessitate repair, but when surgical intervention is undertaken, recurrence is common. Standard surgical approaches include local suture repair, local prosthetic mesh placement, and stoma transposition with or without midline laparotomy. Using these approaches, repair can be difficult and associated with significant morbidity and even mortality.1–3 In addition, the recurrence rate has been reported to be up to 76%.1,4 Favorable outcomes following laparoscopic (LAP) PH repair with mesh have been reported in case reports and small case series.3,5–11 We report our experience with LAP PH repair in a colorectal patient population and propose that LAP PH repair is a suitable and effective approach in the management of this disease.
MATERIALS AND METHODS
Data Collection
A retrospective chart review was performed on all patients with PH at the site of an ileostomy or colostomy who underwent LAP or open surgical repair at our institution between November 1999 and November 2006. Repairs involving stoma transposition or stomal closure were excluded. Patients were divided into 2 subgroups, LAP and open. Data were taken from the time of first open repair in the open group and first LAP repair in the LAP group. Patients were sorted into groups on an intent-to-treat basis, and the one converted LAP patient was kept in the LAP group. Data collected included patient demographics, indication for initial stoma creation, operative time, length of stay (LOS), postoperative complications, recurrence, and follow-up. Results were compared by the t test and Fisher's exact test where appropriate. The hospital's institutional review board approved the study.
OPERATIVE TECHNIQUE
Laparoscopic Repair With Slit or Nonslit Mesh
All patients were placed in the supine position with an Ioban drape (3M, St. Paul, MN) placed over the abdomen.
Peritoneal access was achieved with an 11-mm optical trocar (Optiview, Ethicon, Cincinnati, OH) placed diagonally to the hernia. One 5-mm port was placed opposite the 11-mm port, superior to the ostomy, and one 5-mm port was placed inferiorly to the 11-mm port (Figure 1). The herniated bowel and omentum were carefully reduced from the hernia defect (Figure 2A). A spinal needle was then used to gauge the size of the defect. A polytetrafluoroethylene (PTFE) mesh (Dual Mesh, Gore & Associates, Newark, DE) large enough to create at least a 4-cm overlap in all directions was used for all repairs. 0 Prolene sutures were placed in the 4 corners of the mesh. Additional transfascial sutures were placed no more than 5cm apart. The mesh was then rolled and inserted into the abdomen through the 11-mm port. An Endoclose device (US Surgical, Norwalk, CT) was used to grasp the Prolene sutures for tying over the fascia in the subcutaneous space. For the 7 most recent patients, a nonslit flap configuration was used with the bowel (stoma) exiting laterally. A ProTack device (US Surgical, Norwalk, CT) was used to fix the edges of the mesh circumferentially except laterally, where the bowel came around the mesh. The bowel was pinned against the lateral anterior abdominal wall by the mesh to create a modified Sugarbaker hernia repair (Figure 2B).12 Alternatively, in the first 3 patients, a keyhole was cut, and a 3-cm aperture for the bowel was created in the mesh prior to implantation. In another patient, also operated on early within the reviewed time period, a diagonal, lateral slit was made to accommodate passage of the intestine. In the 4 patients with cut or slit mesh, the mesh was fashioned around the bowel. A ProTack device was then used to circumferentially secure the mesh around the bowel and perimeter. Tacks were also placed lateral to the mesh to close the slit, thus creating a 3-cm to 4-cm aperture around the bowel. At the conclusion of the repair, the fascia at the Optiview port site was closed with figure-of-eight Vicryl suture. The wounds were sealed with Dermabond (Ethicon, Cincinnati, OH).
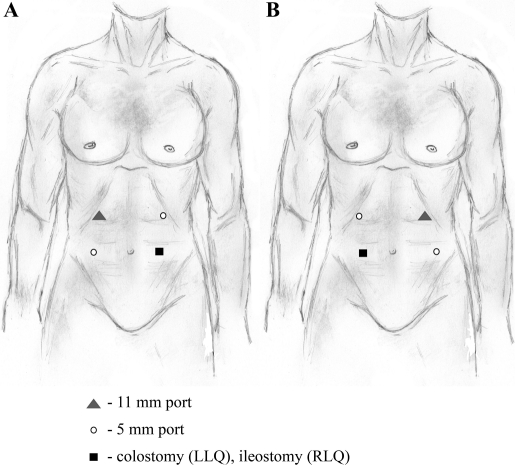
Figure 1.
Location of trocar placement for repair of left-sided PH (A) and for repair of right-sided PH (B).
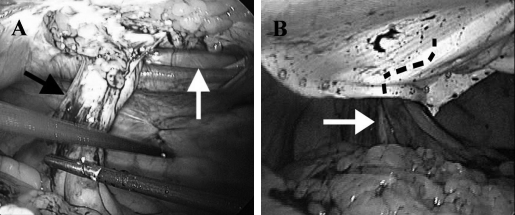
Figure 2.
Colostomy (black arrow) with associated parastomal fascial defect (white arrow) following reduction of herniated bowel (A); Intact Gore-Tex Dual Mesh against anterior abdominal wall with underlying bowel limb (black, dashed line) obliquely exiting from mesh (white arrow) (B).
Local Fascial Repair
A midline incision through the prior incision site at the level of the stoma or a circumstomal, curvilinear incision outside the limits of the stomal faceplate was created. Following subcutaneous dissection and identification of the hernia defect, the hernia sac was entered and freed circumferentially from the stoma. The prolapsed intestine was reduced into the abdomen. The fascial defect was closed with interrupted figure-of-eight or simple stitches of either #1 Prolene or 0 Ethibond. In one case, the terminal ileum was tethered to the anterior abdominal wall. The soft tissue defect was closed with interrupted Vicryl suture, and the skin was closed with running subcuticular Vicryl suture. Mesh was not used in the local fascial repairs.
RESULTS
A total of 25 patients with ileostomies or colostomies underwent PH repair by the open approach or laparoscopic mesh placement between November 1999 and November 2006. The LAP repairs were all performed by 2 surgeons (RH and TS) who had completed minimally invasive surgery fellowships. All of the open repairs were performed by 2 board-certified colon and rectal surgeons (WK and LP). Twelve patients (mean age 60, range 25 to 80 years) underwent LAP approaches, with one patient requiring conversion to laparotomy with primary suture repair of the PH secondary to small-bowel enterotomy. Thirteen patients (mean age 54; range, 35 to 71 years) underwent open PH repair. Patient characteristics are listed in Table 1.
Table 1.
Characterization of 25 Patients Having Undergone Laparoscopic or Open Parastomal Repair
| Patient Information* | Lap | Open | P Value |
|---|---|---|---|
| Total # of Patients | 12 | 13 | – |
| Mean Age (years) ± SE | 60 ±5.13 | 54 ±3.07 | 0.24 |
| Male/Female | 5/7 | 7/6 | – |
| Stoma Type | |||
| Ileostomy | 6 | 9 | – |
| Colostomy | 6 | 4 | – |
| Indication for Initial Stoma Creation | |||
| Inflammatory Bowel Disease | 4 | 8 | – |
| Rectal cancer | 4 | 3 | – |
| Other† | 4 | 2 | – |
| Mean OR Time (minutes) ± SE | 172 ±10.0 | 137 ±19.1 | 0.14 |
| Mean LOS (days) ± SE | 3.08 ±0.43 | 5.08 ±0.83 | 0.05 |
| Complications | 4 (33.3%) | 2 (15.4%) | 0.38 |
| Recurrences | 4 (33.3%) | 7 (53.8%) | 0.43 |
| Mean Time to Recur (months) ± SE | 10.0 ±3.48 | 20.3 ±6.99 | 0.26 |
| Mean Follow-Up (months) ± SE | 13.9 ±4.50 | 14.0 ±4.30 | 0.98 |
SE = standard error; LOS = length of stay.
Diverticulitis, GIST, Paget's disease, radiation proctitis, strangulated abdominal wall abscess, anismus.
Indications for initial stoma creation were ulcerative colitis (3 LAP, 6 open), Crohn's disease (2 open), rectal cancer (4 LAP, 3 open), diverticulitis (1 LAP), anismus (1 LAP), radiation proctitis (1 LAP), gastrointestinal stromal tumor (GIST) (1 open), Paget's disease (1 LAP), strangulated abdominal wall abscess (1 open), and rectal cancer in the setting of Crohn's disease (1 LAP). Five patients had previously undergone open PH repairs: 4 in the LAP group and 1 patient in the open group. Twenty-three of the twenty-five PH repairs (92%) were performed electively. Indications for elective repair included chronic discomfort or progressive pain (7 LAP, 7 open), bulging contributing to difficult maintenance of stomal appliances (4 LAP, 3 open), and chronic obstruction (1 LAP, 1 open). Two repairs (8%) were performed urgently via laparotomy for incarceration.
Operative time for repair was not statistically significant between the 2 groups [172±10.0 min (LAP) versus 137±19.1 min (open)], P=0.14. The difference between LOS for the LAP group (3.1±0.4 days) and open group (5.1±0.8 days) approached significance, P=0.05. Immediate postoperative complications occurred in 4 LAP patients (33.3%) and 2 open patients (15.4%), P=0.38. In the LAP group, complications were 2 wound infections, parastomal cellulitis, and a seroma beneath the mesh. The 2 wound infections resolved with antibiotics and wound care. No complications secondary to mesh erosion into bowel or mesh infection were seen in the LAP group. The 2 complications in the open group were wound infections, one of which was a perineal wound infection separate from the PH repair site following a completion proctectomy that was simultaneously performed with the PH repair. The second complication was a parastomal abscess with subsequent fistula development, subsequently repaired by laparotomy, transection of the fistula tract, and resiting of the ileostomy.
Eleven of the 25 PH recurred (44%). Of these recurrences, 4 (33%) were in the LAP group and 7 (54%) were in the open group. Recurrences were evenly distributed among ileostomies and colostomies within the 2 groups (2 para ileostomal and 2 para-colostomal recurrences in the LAP group; 3 para-colostomal and 4 ileostomal recurrences in the open group). In the LAP patients repaired by a modified Sugarbaker technique, 2 hernias recurred (29%). One of these patients developed a respiratory infection following her repair and experienced severe cough, which may have contributed to an increase in intraabdominal pressure, thus promoting her recurrence. This patient underwent a subsequent laparoscopic repair, and it was noted that one transfascial suture appeared to have torn through the mesh. Among the 3 patients who had undergone mesh repair utilizing a keyhole-cut mesh, 2 recurred, resulting in a 67% recurrence rate among the total of 3 keyhole repairs. Among our 13 patients who had local suture repairs, 7 recurred (54%), although one recurrence was associated with a motor vehicle collision at 10 months postoperative time in which the patient was a restrained driver.
Recurrences in the LAP group occurred after 10.5±3.48 months versus 20.3±6.99 months in the open group. Mean length of follow-up was 13.9±4.50 months for the LAP group and 14.0±4.30 months for the open group.
DISCUSSION
PH, the protrusion of abdominal contents through the fascial defect surrounding a stoma, represents a common complication of stoma construction that remains challenging to manage. Small, asymptomatic hernias are often undiagnosed. When they are diagnosed, they can often be managed without surgery using a hernia support belt, weight loss, avoidance of lifting heavy objects, observation, and patient education. Larger, symptomatic hernias that cause pain, obstruction, and difficulty with maintenance of the appliance, as well as create cosmetic and other quality of life issues, warrant surgical repair.
Classically, 3 methods have been utilized to repair PH: local primary fascial repair, local mesh repair, and stoma transposition. Varying results following repair utilizing these 3 techniques have been reported. Recurrence rates of 46% to 76% following simple fascial repair have been described, with associated complication rates up to 71%, including death.1,2,11,13,14 In our study, we found a recurrence rate with open fascial repair similar to that reported in the literature at 53.8%, but had a much lower complication rate than that occurring in most studies at 15.4%.
The incorporation of synthetic mesh into local PH repairs results in a lower recurrence rate but can be associated with serious complications, such as dense adhesion formation to the mesh, mesh infection, abscess development, and perforation or mesh erosion into the bowel.15,16 Since the 1970s, the preference for type of mesh used in PH repair has changed from polyethylene to polypropylene to PTFE to expanded polytetrafluoroethylene (ePTFE), the last being a softer, smoother, low-porosity membrane that promotes minimal inflammation and adhesion formation while allowing tissue ingrowth.17–21
One consideration in mesh repair is whether to create an opening in the mesh through which the bowel may exit or pin the bowel against the abdominal wall with the mesh. Several studies utilizing mesh through different open approaches and with alternative modifications have reported varying success rates. Tekkis et al22 described a modified Thorlakson technique that incorporated an incomplete circumferential mesh to reinforce fascial repair. This technique was performed on 5 patients in whom, in a short-term follow-up of less than 2 years, PH had not recurred, though 40% experienced complications of hematoma or prolapse. Saclarides et al23 reviewed their experience with in situ Y-split mesh repair and noted an 11% recurrence and complications of hematoma and delayed resumption of oral intake. Stelzner et al24 reported a similar recurrence rate of 15% after repair of paracolostomy hernia with prosthetic nonslit mesh, after a mean follow-up of 3.5 years. Longman and Thompson25 showed promising results with a modification of in situ split mesh repair that included tacking back the triangular flaps from the opening created in the mesh. Over a median follow-up period of 30 months, no recurrences had developed and only one complication of superficial wound breakdown had occurred.
Alternatives to local repair, such as transposition, or resiting of the stoma with repair of the fascial defect, are also not without challenge. Failure rates following stoma resiting are reported to range from 15% to 57%, rates that are improved compared with those associated with fascial repair, but many of which are associated with higher complication rates, up to 88%.1,2,13,26
Regardless of type of PH repair, no one method has emerged as ideal with which to set the standard of surgical treatment. In recent years, expanding knowledge of and experience with laparoscopic techniques have heralded innovative approaches to this dilemma. Results of the first laparoscopic approaches to PH repair with mesh reinforcement were case reports published in 1998 and 1999, by Porcheron et al5 and Bickel et al,6 respectively. A small case series of 4 patients undergoing laparoscopic PH repair with mesh reinforcement was published by Kozlowski et al in 2001.10Operative time was long, an average of 4.3 hours, but no recurrences had developed at 2 months to 33 months. LeBlanc et al3 went on to incorporate the use of overlapping prosthesis in a comparison of single mesh onlay with double-patch techniques of 2 different types versus 2 identical pieces of ePTFE mesh. Of 7 onlay repairs, none recurred; of 5 2-patch repairs, one parastomal hernia recurred. Twenty-five percent of patients experienced complications of intraoperative enterotomy, ileus, seroma, obstruction, and death. In 2007, Hansson et al27 performed a multi-center trial using “funnel-shaped” ePTFE mesh in 55 patients. Eight cases were converted due to dense adhesions or contamination secondary to full-thickness bowel injury. No recurrences were noted in the laparoscopic group. Two patients (one conversion secondary to bowel injury) required mesh removal secondary to mesh infection or abscess.
In our study, we sought to review our experience with PH repair. Early in our laparoscopic experience, we used a slit or keyhole-cut mesh in 4 patients. More recent laparoscopic repairs (subsequent 7 patients) were based on a modified Sugarbaker technique through which 3 essential elements were incorporated: intraperitoneal placement of nonslit mesh, lateralization of the bowel limb between the mesh and abdominal wall, and fixation of transfascial sutures no more than 5cm apart.12 Intraoperative complications occurred in 2 of the 12 laparoscopic patients. The first was a full thickness small bowel injury necessitating conversion to an open procedure. The second was a serosal thermal injury to the colon that was repaired by oversewing the injury laparoscopically, thus avoiding conversion. There were no intraoperative complications in the open group.
The 3 LAP patients who developed wound infections or parastomal cellulitis recovered with antibiotics and wound care. Mesh infection is a serious complication, often requiring mesh removal. No patient in our LAP group had mesh infection or mesh erosion into the bowel. It can also be argued that bowel lateralization following mesh placement can potentially lead to bowel obstruction. However, in our study, no postoperative bowel obstructions were seen, suggesting that securing the intestine against the abdominal wall does not cause obstruction and that a slit may be unnecessary.
Overall, our laparoscopic recurrence rate was 33%. Early in our experience, we used a keyhole mesh technique, resulting in a 67% recurrence rate. We then changed our approach to utilize a modified Sugarbaker technique and have since experienced a recurrence rate of 29%. We believe that this improvement in recurrence rate is due both to increasing experience and a better technique.
CONCLUSION
PH remains a difficult problem. High complication and recurrence rates continue to be associated with surgical repair. Our experience with the laparoscopic modified Sugarbaker technique in the repair of PH continues to increase. This approach provides an alternative strategy to open repair with which to treat the common and difficult problem of PH.
Contributor Information
Danielle M. Pastor, Division of Colon & Rectal Surgery, Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA..
Eric M. Pauli, Section of Minimally Invasive Surgery, Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA..
Walter A. Koltun, Division of Colon & Rectal Surgery, Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA..
Randy S. Haluck, Section of Minimally Invasive Surgery, Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA..
Timothy R. Shope, Section of Minimally Invasive Surgery, Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA..
Lisa S. Poritz, Division of Colon & Rectal Surgery, Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA..
References:
- 1.Rubin MS, Schoetz DJ, Jr., Matthews JB. Parastomal hernia. is stoma relocation superior to fascial repair? Arch Surg. 1994;129(4):413–418 [DOI] [PubMed] [Google Scholar]
- 2.Rieger N, Moore J, Hewett P, Lee S, Stephens J. Parastomal hernia repair. Colorectal Dis. 2004;6(3):203–205 [DOI] [PubMed] [Google Scholar]
- 3.LeBlanc KA, Bellanger DE, Whitaker JM, Hausmann MG. Laparoscopic parastomal hernia repair. Hernia. 2005;9(2):140–144 [DOI] [PubMed] [Google Scholar]
- 4.Thorlakson RH. Technique of repair of herniations associated with colonic stomas. Surg Gynecol Obstet. 1965;120:347–350 [PubMed] [Google Scholar]
- 5.Porcheron J, Payan B, Balique JG. Mesh repair of paracolostomal hernia by laparoscopy. Surg Endosc. 1998;12(10):1281. [DOI] [PubMed] [Google Scholar]
- 6.Bickel A, Shinkarevsky E, Eitan A. Laparoscopic repair of paracolostomy hernia. J Laparoendosc Adv Surg Tech A. 1999;9(4):353–355 [DOI] [PubMed] [Google Scholar]
- 7.Deol ZK, Shayani V. Laparoscopic parastomal hernia repair. Arch Surg. 2003;138(2):203–205 [DOI] [PubMed] [Google Scholar]
- 8.Pekmezci S, Memisoglu K, Karahasanoglu T, Alemdaroglu K. Laparoscopic giant parastomal hernia repair with prosthetic mesh. Tech Coloproctol. 2002;6(3):187–190 [DOI] [PubMed] [Google Scholar]
- 9.Voitk A. Simple technique for laparoscopic paracolostomy hernia repair. Dis Colon Rectum. 2000;43(10):1451–1453 [DOI] [PubMed] [Google Scholar]
- 10.Kozlowski PM, Wang PC, Winfield HN. Laparoscopic repair of incisional and parastomal hernias after major genitourinary or abdominal surgery. J Endourol. 2001;15(2):175–179 [DOI] [PubMed] [Google Scholar]
- 11.Hansson BM, van Nieuwenhoven EJ, Bleichrodt RP. Promising new technique in the repair of parastomal hernia. Surg Endosc. 2003;17(11):1789–1791 [DOI] [PubMed] [Google Scholar]
- 12.Sugarbaker PH. Peritoneal approach to prosthetic mesh repair of paraostomy hernias. Ann Surg. 1985;201(3):344–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Allen-Mersh TG, Thomson JP. Surgical treatment of colostomy complications. Br J Surg. 1988;75(5):416–418 [DOI] [PubMed] [Google Scholar]
- 14.Cheung MT, Chia NH, Chiu WY. Surgical treatment of parastomal hernia complicating sigmoid colostomies. Dis Colon Rectum. 2001;44(2):266–270 [DOI] [PubMed] [Google Scholar]
- 15.Morris-Stiff G, Hughes LE. The continuing challenge of parastomal hernia: failure of a novel polypropylene mesh repair. Ann R Coll Surg Engl. 1998;80(3):184–187 [PMC free article] [PubMed] [Google Scholar]
- 16.Aldridge AJ, Simson JN. Erosion and perforation of colon by synthetic mesh in a recurrent paracolostomy hernia. Hernia. 2001;5(2):110–112 [DOI] [PubMed] [Google Scholar]
- 17.Ballas KD, Rafailidis SF, Marakis GN, Pavlidis TE, Sakadamis AK. Intraperitoneal ePTFE mesh repair of parastomal hernias. Hernia. 2006;10(4):350–353 [DOI] [PubMed] [Google Scholar]
- 18.Toy FK, Bailey RW, Carey S, et al. Prospective, multicenter study of laparoscopic ventral hernioplasty. Preliminary results. Surg Endosc. 1998;12(7):955–959 [DOI] [PubMed] [Google Scholar]
- 19.Christoforoni PM, Kim YB, Preys Z, Lay RY, Montz FJ. Adhesion formation after incisional hernia repair: a randomized porcine trial. Am Surg. 1996;62(11):935–938 [PubMed] [Google Scholar]
- 20.Law N, Ellis H. Adhesion formation and peritoneal healing on prosthetic materials. Clinical Mater. 1988;3:95–101 [Google Scholar]
- 21.Murphy JL, Freeman JB, Dionne PG. Comparison of Marlex and Gore-tex to repair abdominal wall defects in the rat. Can J Surg. 1989;32(4):244–247 [PubMed] [Google Scholar]
- 22.Tekkis PP, Kocher HM, Payne JG. Parastomal hernia repair: modified thorlakson technique, reinforced by polypropylene mesh. Dis Colon Rectum. 1999;42(11):1505–1508 [DOI] [PubMed] [Google Scholar]
- 23.Saclarides TJ, Hsu A, Quiros R. In situ mesh repair of parastomal hernias. Am Surg. 2004;70(8):701–705 [PubMed] [Google Scholar]
- 24.Stelzner S, Hellmich G, Ludwig K. Repair of paracolostomy hernias with a prosthetic mesh in the intraperitoneal onlay position: modified Sugarbaker technique. Dis Colon Rectum. 2004;47(2):185–191 [DOI] [PubMed] [Google Scholar]
- 25.Longman RJ, Thomson WH. Mesh repair of parastomal hernias–a safety modification. Colorectal Dis. 2005;7(3):292–294 [DOI] [PubMed] [Google Scholar]
- 26.Baig MK, Larach JA, Chang S, et al. Outcome of parastomal hernia repair with and without midline laparotomy. Tech Coloproctol. 2006;10(4):282–286 [DOI] [PubMed] [Google Scholar]
- 27.Hansson BM, de Hingh IH, Bleichrodt RP. Laparoscopic parastomal hernia repair is feasible and safe: early results of a prospective clinical study including 55 consecutive patients. Surg Endosc. 2007;21(6):989–993 [DOI] [PubMed] [Google Scholar]