Abstract
Introduction:
Spigelian hernia is an uncommon ventral hernia characterized by a defect in the linea semilunaris. Repair of spigelian hernia has traditionally been accomplished via an open transverse incision and primary repair. The purpose of this article is to present 2 case reports of incarcerated spigelian hernia that were successfully repaired laparoscopically using Gortex mesh and to present a review of the literature regarding laparoscopic repair of spigelian hernias.
Methods:
Retrospective chart review and Medline literature search.
Results:
Two patients underwent laparoscopic mesh repair of incarcerated spigelian hernias. Both were started on a regular diet on postoperative day 1 and discharged on postoperative days 2 and 3. One patient developed a seroma that resolved without intervention. There was complete resolution of preoperative symptoms at the 12-month follow-up.
Conclusion:
Minimally invasive repair of spigelian hernias is an alternative to the traditional open surgical technique. Further studies are needed to directly compare the open and the laparoscopic repair.
Keywords: Spigelian hernia, Laparoscopic hernia repair
INTRODUCTION
The semilunar line was first described by the Belgian anatomist Adriaan van der Spieghal in 1645. Almost a century later, a Flemish anatomist, Josef Klinkosch, coined the term “spigelian hernia” to describe a defect in the semilunar line.1 Throughout history, spigelian hernias have also been known as “spontaneous lateral ventral hernias,” “hernia of the semilunar line,” and “hernias through the conjoint tendon.”2
Spigelian hernias constitute approximately 1% to 2% of all abdominal wall hernias.3 Previous studies have suggested that the total number of previously reported cases worldwide is around 900.4,5 In the initial stages of development, Spigelian hernias are often difficult to diagnose by physical examination because the hernia originates inferior to an intact external oblique aponeurosis.6 Physical diagnosis correctly identifies spigelian hernias approximately 50% of the time; thus, with the advances in radiological imaging, an increase has occurred in the number of spigelian hernia cases diagnosed in the past decade compared with previous decades. Both ultrasound and computed tomography are useful radiological adjuncts for diagnosing spigelian hernias.6
Traditionally, spigelian hernias have been repaired with an open surgical technique. However, in the past few decades, laparoscopic repair has become a promising alternative for repair. The purpose of this article is twofold: first, to present 2 case reports of incarcerated spigelian hernias that were successfully repaired laparoscopically using a dual-sided polytetrafluoroethylene (ePTFE, Gortex) mesh, and second, to compare the various laparoscopic repair techniques reported in the published literature to date.
CASE REPORT ONE
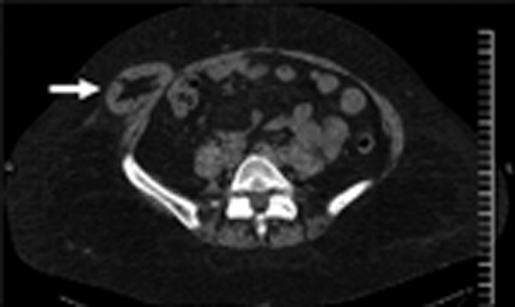
A 54-year-old woman presented with intermittent, crampy, abdominal pain of several months duration. The patient complained of a bulge on the right side of her abdomen that had developed rather suddenly over several weeks. The patient denied any nausea, vomiting, or constipation. Her past surgical history included 2 cesarean deliveries and a total abdominal hysterectomy with bilateral salpingo-oophorectomy. On physical examination, a tender bulge was found on the right side of the patient's abdomen that was most prominent while the patient was standing. An abdominal computed tomography scan showed a large right-sided incarcerated spigelian hernia (Figure 1). The patient elected to have a laparoscopic spigelian hernia repair with mesh. The operation was performed with the patient under general anesthesia. Four trocar sites were used, duration was approximately 1.5 hours, estimated blood loss (EBL) was minimal, and dual-sided polytetrafluoroethylene (ePTFE, Gortex) mesh was used for the repair. The patient was tolerating a liquid diet on postoperative day one (POD 1). The patient had some nausea that was controlled with medication, tolerated a regular diet on POD 2 and was discharged home on POD 3. One week after surgery, the patient was noted to have an asymptomatic seroma, approximately 4 × 3 cm in size. The seroma was observed and resolved within 4 weeks without treatment.
Figure 1.
Abdominal computed tomography of a right-sided incarcerated spigelian hernia. White arrow depicts the right-sided hernia sac that has protruded through the transverses abdominus, internal oblique, and external oblique muscles.
CASE REPORT TWO
The second patient is a 39-year-old woman who presented with constipation and intermittent abdominal pain of several months duration. Her past surgical history was significant for a kidney transplant in 2003, cholecystectomy in 2004, and an appendectomy in 1980. She had a past medical history of systemic lupus erythematosus and was taking maintenance immunosuppression medications. On physical examination, she had a mass on the right side of the abdomen that was tender to palpation. This mass did not appear to be an incisional hernia from previous surgeries. As in the first case, the mass was most prominent when the patient was standing. An abdominal computed tomography scan demonstrated an incarcerated right-sided spigelian hernia. The patient also underwent a laparoscopic repair of the spigelian hernia. The same method was used as in the first case except that most of the hernia sac was resected. The operation was performed with the patient under general endotracheal intubation, 4 trocar sites were used, duration was approximately 1.5 hours, EBL was minimal, dual-sided polytetrafluoroethylene (ePTFE, Gortex) mesh was used for the repair. The patient was tolerating a liquid diet on POD 1, a regular diet on POD 2, and was discharged home on POD 2.
OPERATIVE PROCEDURE
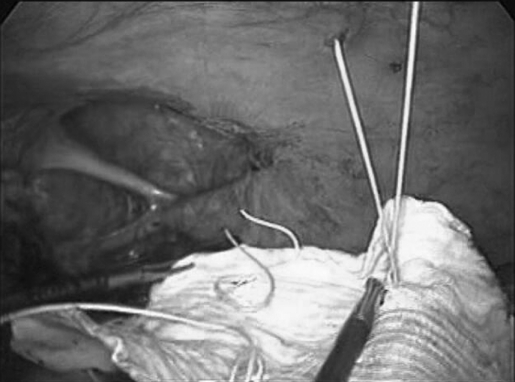
Both patients had laparoscopic reduction of their incarcerated spigelian hernias and repair using dual-sided 2-mm Gortex, ePTFE mesh. Four laparoscopic ports were used with a 30-degree scope placed in the supraumbilical location. Following pneumoperitoneum, the abdomen was inspected, and adhesions were taken down with the LigaSure system (ValleyLab, Colorado). Both incarcerated spigelian hernias contained bowel and omentum (Figure 2). No physical evidence was found of any necrotic bowel.
Figure 2.
Intraoperative image of the right-sided incarcerated spigelian hernia. The hernia sac contained omentum and bowel.
Both hernia defects measured approximately 8 × 6 cm. A 2 mm × 15 cm × 10 cm dual-sided Gortex ePTFE mesh was used to repair both fascial defects. Using a 0-Gortex suture, stay sutures were placed extraperitoneally in the 4 corners of the Gortex mesh. The mesh was then rolled up and inserted into the abdomen. Atraumatic graspers were used to unroll the mesh with the smooth side of the mesh towards the intestines. The appropriate locations of the 4 corners of the fascia surrounding the hernia defect were identified. Beginning laterally, a suture passer was inserted in the upper outer margin of normal fascia (to the right of the superior most border of the fascial defect). The corresponding stay suture was secured in the needle passer and withdrawn through the insertion side and secured outside of the abdomen with a hemostat (Figure 3).
Figure 3.
Intraabdominal photograph depicting the dual-sided Gortex mesh with all 4 Gortex stay sutures.
The remaining corner stay sutures were similarly secured outside the abdomen and then all 4 sutures were tied securely with the knots carefully pushed down through the single corresponding stab incision. This maneuver allowed the mesh to be flush against the anterior abdominal wall, completely covering the hernia defect with a minimum 3-cm margin (Figure 3). The mesh was further secured to the anterior abdominal wall by metallic spiral tacks. The tacks were placed approximately 1 cm to 1.5 cm apart around the entire edge of the mesh. Care was taken to provide counterpressure while securing the spiral tacks (Figure 4).
Figure 4.
Intraabdominal photograph depicting the dual-sided Gortex mesh flush against the anterior abdominal wall with the metallic spiral tacks.
LITERATURE REVIEW
Spigelian hernias have traditionally been repaired with an open surgical technique; however, minimally invasive repair has become a promising alternative for surgical repair. One of the limitations of doing a literature review to compare various laparoscopic techniques is that spigelian hernias constitute only 1% to 2% of all ventral hernias and the majority of studies are single case reports. Therefore, few randomized controlled trails directly compare the open surgical technique with the laparoscopic technique for repairing spigelian hernias.
Mareno-Egea and colleagues7 completed one of the few randomized controlled trials comparing the open versus the laparoscopic surgical repair in nonincarcerated spigelian hernias as shown in Table 1. They reported on 22 patients, with 11 having an open repair and 11 having a laparoscopic repair. No significant difference occurred in hernia recurrence between the 2 groups after a 3.5-year follow-up. There were, however, significant differences in morbidity and hospital stay between the open and laparoscopic groups. Length of stay for patients having open surgical repair averaged 5 days, while the patients with the laparoscopic repair averaged 1 day in the hospital. One of the limitations of this study was that the laparoscopic repair included both an extraperitoneal on-lay technique using polypropylene and an intraperitoneal underlay technique using Parietex composite double-layer mesh. Eight patients were in the extraperitoneal group, and 3 were in the intraperitoneal group. One of the disadvantages of this study was that it did not directly compare laparoscopic intraperitoneal repair with an open surgical technique.
Table 1.
List of the Recent Studies Regarding Laparoscopic Repair of Spigelian Hernias
| Study Type* | Author | No. Patients* | Repair* | Mesh | Complication* |
|---|---|---|---|---|---|
| RCT | Moreno-Egea et al 2002 | 11 open | 8 TEP | Prolene | None |
| 11 lap | 3 IA | Parietex | |||
| Case Series | Felix et al 1994 | 4 | IA | Prolene | None |
| Case Series | Palanivelu et al 2006 | 8 | IA | Prolene | None |
| Case Report | Amendolara et al 1998 | 2 | IA | Prolene | None |
| Case Reports | Martell et al 2004 | 1 | IA | Prolene | None |
| Case Reports | Fisher et al, 1994 | 1 | IA | Prolene | Hematoma LIH |
| Case Reports | Lopez-Tomassetti et al, 2006 | 1 | IA | PTFE Gortex Dual Mesh | None |
RCT = randomized controlled trial; open = open surgical repair, lap = laparoscopic repair; TEP = total extraperitoneal repair; IA = intraabdominal (intraperitoneal) repair, LIH = left inguinal hernia; PTFE = Polytetrafluoroethylene.
Several prospective case series have used polypropylene mesh for laparoscopic repair of spigelian hernias. In 2006, Palanivelu and colleagues8 repaired 8 spigelian hernias with a primary fascial repair followed by placement of a polypropylene mesh for reinforcement. The polypropylene mesh was secured by several interrupted polypropylene sutures. Three of the patients had incarcerated hernias containing bowel or omentum. There were no postoperative complications or recurrences after a 3.5-year follow-up.8 Felix and colleagues9 reported successful laparoscopic repair of 4 spigelian hernias with intraperitoneal underlay of polypropylene mesh. No immediate postoperative complications occurred; however, long-term follow-up was not addressed in the article. One of the disadvantages of the case series was that the mesh was made of polypropylene and closure varied from primary fascial closure to intraperitoneal overlay.
In addition to the case series, there have been several case reports of successful laparoscopic repair of spigelian hernias. In the majority of reported cases polypropylene mesh has been used and both incarcerated and nonincarcerated hernias have been repaired. Amendolara et al10 repaired 2 incarcerated spigelian hernias with polypropylene mesh securing the mesh edges with titanium clips. Martell et al11 repaired a single incarcerated spigelian hernia using polypropylene mesh, but secured the mesh using spiral tacks. Similarly, Fisher12 in 1994 published a case report on successfully repairing an incarcerated spigelian hernia in a 71-year-old man by using polypropylene mesh. In general, the patients in these case series had a benign postoperative course and were discharged 24 hours to 49 hours postoperatively.
While polypropylene mesh was used in the majority of case reports, the report by Lopez-Tomassetti et al13 is one of the few where polytetrafluoroethylene (PTFE, Gortex) mesh was used to repair an incarcerated spigelian hernia. The fascial defect measured approximately 7 cm × 6 cm, and a 10 cm × 15 cm Gortex mesh was used for an underlay intraperitoneal repair. No evidence was found of necrotic bowel. The mesh was secured by using 2 rows of spiral tacks with one row of tacks about 3 cm and the other row of tacks about 0.5 cm from the fascial defect. The patient had a benign postoperative course and was discharged within 72 hours of surgery. At the 10-month follow-up, the patient remained asymptomatic. One of the advantages of this case report is that dual-sided Gortex mesh was successfully used for an incarcerated spigelian hernia.
DISCUSSION
Due to the location of spigelian hernias, diagnosis of this type of hernia by physical examination is unreliable. Such findings can include a bulge made worse by lumbar flexion located on the lateral aspect of the abdominal wall. In the initial stages of development, spigelian hernias are often difficult to diagnose by physical examination because the hernia originates inferior to an intact external oblique aponeurosis.6 Symptoms can include abdominal pain or discomfort with or without obstructive symptoms, often made worse with straining or other increases in intraabdominal pressure. Today, the majority of spigelian hernias are diagnosed with either ultrasound or computed tomography, but traditionally they were diagnosed during operative exploration.
Previous authors14,15 have speculated that spigelian hernias can be both acquired and inherited. While the exact cause is unknown, the development of a spigelian hernia is likely multifactorial involving one or more factors: collagen disorders, aging, obesity, rapid weight loss, multiple pregnancies, chronic pulmonary diseases, trauma, iatrogenic, and congenital.4,16,17 Although multiple conditions predispose people to acquire spigelian hernias, recent reports have found that at least 50% of all patients with spigelian hernias had previous abdominal surgeries including both open and laparoscopic surgeries.17,18
The spigelian aponeurosis is formed by the fusion of the internal oblique and the transverses abdominis aponeurosis. The spigelian aponeurosis is limited laterally by the linea semilunaris, and medially by the lateral edge of the rectus muscle. The spigelian aponeurosis extends from the costal cartilage of the eighth rib to the symphysis pubis.1,5,17 In the upper abdominal wall, the spigelian aponeurosis is posterior to the rectus muscle making it difficult to locate a fascial defect on physical examination. Superior to the umbilical region, the aponeurosis of the internal oblique crosses over the transverses in a perpendicular fashion creating a strong abdominal wall barrier. Inferior to the umbilical region, these aponeuroses run parallel to each other. These parallel fibers form a weak barrier that is susceptible to protruding peritoneal sacs or extraperitoneal fat.1,2,17,19 More than half of all spigelian hernias are located in a 6-cm wide region inferior to the umbilicus and superior to the inferior epigastric vessels. This region is referred to as “the spigelian hernia belt.”1
The spigelian hernia sac often contains extraperitoneal fat, peritoneum, small bowel, or omentum.3 In addition, previous studies have reported various abdominal contents including stomach, gallbladder, Meckel's diverticulum, ovary, testis, and bladder.1,20 Spigelian hernias often have a narrow fascial defect and therefore have an increased risk of incarceration and strangulation. The incarceration rate has been reported to be as high as 24%.4
CONCLUSION
Spigelian hernias are an uncommon type of ventral hernia. To date, most surgical repairs have used an open technique. However, minimally invasive repair of spigelian hernia has become a promising alternative to open surgery. Due to the rarity of this hernia, the majority of the literature contains case reports, and the majority of laparoscopic repairs have been done with polypropylene mesh. Further studies are needed to directly compare recurrence rates of the minimally invasive repair with that of the open surgical repair. This paper demonstrates that an incarcerated spigelian hernia can be successfully repaired by using dual-sided polytetrafluoroethylene (ePTFE, Gortex) mesh.
Based on available evidence published on laparoscopic ventral hernia repair, especially the more common incisional hernia, we conclude that laparoscopic repair is becoming the preferred method where expertise exists. However, the optimal laparoscopic technique remains debatable.20 Advancements in mesh technology and fixation devices (tackers) or potentially the application of energy-based tissue fusion will likely allow for further improvements in the outcomes of spigelian hernia repair.
References:
- 1.Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Spigelian hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2006;72:42–48 [PubMed] [Google Scholar]
- 2.Olson RO, Davis WC. Spigelian hernia: rare or obscure? Am J Surg. 1968;116:842–846 [DOI] [PubMed] [Google Scholar]
- 3.Houlihan TJ. A review of spigelian hernia. Am J Surg. 1976;131:734–735 [DOI] [PubMed] [Google Scholar]
- 4.Spangen L. Spigelian hernia. In: Prostheses and Abdominal Wall Hernias. Bendavid R. ed. Austin: RG Landes; 1994;563 [Google Scholar]
- 5.Spangen L. Spigelian hernia. World J Surg. 1989;13:573–580 [DOI] [PubMed] [Google Scholar]
- 6.Kavic MS. Abdominal wall hernia: the procedure. In: Laparoscopic Hernia Repair. Kavic MS. ed. Amsterdam: Harwood Academic Publishers; 1997;83–94 [Google Scholar]
- 7.Moreno-Egea A, Carrasco L, Girela E, Martin JG, Aguayo JL, Canteras M. Open vs. laparoscopic repair of spigelian hernia. Arch Surg. 2002;137:1266–1268 [DOI] [PubMed] [Google Scholar]
- 8.Palanivelu C, Vijaykumar M, Jani KV, Rajan PS, Maheshkumaar GS, Rajapandian S. Laparoscopic transabdominal preperitoneal repair of spigelian hernia. JSLS. 2006;10:193–198 [PMC free article] [PubMed] [Google Scholar]
- 9.Felix E, Michas C. Laparoscopic repair of spigelian hernias. Surg Laparosc Endosc. 1994;4:308–310 [PubMed] [Google Scholar]
- 10.Amendolara M. Videolaparoscopic treatment of spigelian hernia. Surg Laparosc Endosc. 1998;8(2):136–139 [PubMed] [Google Scholar]
- 11.Martell EG, Singh NN, Zagorski SM, Sawyer MA. Laparoscopic repair of spigelian hernia: a case report and literature review. JSLS. 2004;8:269–274 [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher BL. Video-assisted spigelian hernia repair. Surg Laparosc Endosc. 1994;4(3):238–240 [PubMed] [Google Scholar]
- 13.Lopez-Tomassetti Fernandez EM, Martin Malagón A, Delgado Plasencia L, Arteaga González I. Laparoscopic repair of incarcerated low spigelian hernia with transperitoneal PTFE DualMesh. Surg Laparosco Endosc Percutan Tech. 2006;16(6):427–431 [DOI] [PubMed] [Google Scholar]
- 14.Scopinaro AJ. Hernia on spigels semilunar line in a new born. Semana Med. 1935;1:284 [Google Scholar]
- 15.Bennett D. Incidence and management of primary abdominal wall hernias: umbilical, epigastric, and spigelian. In Nyhus and Condon's Hernia. 5th ed Fitzgibbons RJ, Green-burg AG. eds. Philadephia: Lippincott Williams & Wilkins; 2002;339 [Google Scholar]
- 16.Montes IS, Deysine M. Spigelian and other uncommon hernia repairs. Surg Clin North Am. 2003;83:1235–1253 [DOI] [PubMed] [Google Scholar]
- 17.Sanchez-Montes I, Deysine M. Spigelian hernias. Arch Surg. 1998;133:670–672 [DOI] [PubMed] [Google Scholar]
- 18.Slakey DP, Teplitsky S, Cheng SS. Incarcerated spigelian hernia following laparoscopic living-donor nephrectomy. JSLS. 2002;6(3):217–219 [PMC free article] [PubMed] [Google Scholar]
- 19.Read RC. Observations on the etiology of spigelian hernia. Ann Surg. 1960;152:1004–1009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silberstein PA, Kern IB, Shi EC. Congenital spigelian hernia with cryptorchidism. J Pediatr Surg. 1996;31:1208–1210 [DOI] [PubMed] [Google Scholar]