Abstract
Background:
Pioneers in natural orifice transvaginal cholecystectomy are in search of an approach that uses less percutaneous assistance. The approach must be safe and affordable. The authors present a successful cholecystectomy using a technique of transvaginal operative laparoscopy with no abdominal ports.
Methods:
A 24-year-old female patient with gallbladder lithiasis underwent a natural orifice cholecystectomy with only one transvaginal 12-mm port, using a laparoscope with a working channel. We used laparoscopic instruments 5 mm in diameter by 43cm in length (including a needle holder, Maryland dissector clamp, spatula, hook, suction cannula, and clip applier) and assistance with percutaneous marionette leashes.
Results:
The patient stayed in the hospital for 24 hours and was discharged without pain and without scars.
Conclusion:
Transvaginal cholecystectomy performed using an operative laparoscope with a working channel is possible in select cases. This technique requires no abdominal ports and is an alternative to culdolaparoscopy or hybrid transvaginal procedures with flexible endoscopes.
Keywords: NOTES, Cholecystectomy, Transvaginal, Natural Orifice Surgery
INTRODUCTION
Transvaginal cholecystectomy in humans was a rarity in the medical literature prior to 2007.1 Beginning in 2007, press releases, contributions, and publications became abundant. Most of these articles are related to advances in flexible and magnetic technology. However, advanced instruments are either not currently available or not affordable for most surgeons. Meanwhile, laparoscopes with working channel and bariatric 5-mm instruments are available or customized by the industry for an affordable budget.
This case presents a cholecystectomy performed transvaginally using a laparoscope with a working channel measuring 6mm and laparoscopic instruments measuring 5mm in diameter by 43cm in length. This was done with no additional abdominal ports.
CASE REPORT
A 24-year-old female patient with multiple gallbladder stones and symptoms of cholecytitis was scheduled for surgery. Preoperative laboratory studies, including liver profile tests, were within normal limits. An abdominal ultrasound confirmed the diagnosis. The surgery was performed following the approved IRB protocol for scarless surgery and natural orifice transluminal endoscopic surgery (NOTES).
The patient underwent bimanual pelvic examinations. A Papanicolaou test was done and was negative. The examination showed no obliteration of the pouch of Douglas or vaginal narrowing. The patient received intravenous antibiotic prophylaxis with metronidazole 500mg and cephalosporin 1g within 1 hour before the time of incision. We used Allen telescopic stirrups. This provides an easy way to adjust from a lithotomy to a semi-dorsolithotomy position (which is done by changing the stirrups from 90-degree to 15-degree angles from the horizontal position). Careful positioning and separation of the legs provided enough room to operate in the European position and a Foley catheter was placed.
With the patient in the lithotomy position, a small posterior colpotomy was made for the placement of a port from the posterior vaginal fornix and into the pouch of Douglas. For the procedure, we used a weighted speculum in the posterior vaginal wall. Additional Deaver retractors were used for exposure.
A weighted speculum was placed to retract the posterior wall; we used Deaver retractors to further expose the uterine cervix. A tenaculum (Pozzi) was placed in the anterior lip of the cervix. With the cervix exposed, the cavity was measured with a probe. A dilatation of the cervix was done progressively until 6mm. We used a Kroner uterine manipulator manufactured by Cooper Surgical (Trumbull, CT, USA).
The cervix was grasped again with a tenaculum at the posterior lip. The cervix was elevated anteriorly. We identified the area in the posterior fornix where the posterior vaginal wall meets the cervix. Approximately 1cm to 2cm posterior to this junction is the area for the colpotomy. We used 2 Allis clamps to elevate the area and allow for making a transversal cut of 2cm in length with a curved Mayo scissor (Figure 1). The point of the curved scissor is oriented anteriorly.
Figure 1.
View of the colpotomy.
A vaginal port consisting of a plastic rod that was 10mm in diameter and 46cm in length (PortSaver, ConMed, Utica, NY) was mounted inside an insufflating cannula 12mm in diameter and 15cm in length (Endopath Xcel, Ethicon Endo Surgery Inc, Cincinnati, OH). The plastic rod and the cannula were placed in the pelvic cavity via a colpotomy incision. The weighted speculum was removed, and the insufflation line was attached to the vaginal port and pneumoperitoneum was developed. The patient's thighs were brought to about 15 degrees above the horizontal position while the knees were kept flexed.
The vaginal port was used for placement of a laparoscope with an operative channel (Hopkins Straight Forward Telescope 0° with 6-mm instrument channel, 26034AA, Karl Storz, Germany). The Trendelenburg position was used for the introduction of the laparoscope to the level of the umbilicus and was then changed to the Fowler position for visualization of the gallbladder. Visualization of the gallbladder from the vaginal angle was not difficult. The vaginal port was used for insufflation, visualization, operation, and extraction.
The procedure continues using the transvaginal operating laparoscope for the placement of 3 leashes by using straight needles with 2– 0 (Prolene Ethicon, Cincinnati, OH). The leashes were introduced percutaneously into the peritoneal cavity. Once in the cavity, the needle holder operating from the operative channel grasped the needle, and the leashes were placed through the fundus of the gallbladder. The needle was grasped again with the needle holder and exteriorized from the peritoneum to the skin near the initial entrance point. Both ends of the suture were held with a Kelly clamp with the necessary traction to bring the gallbladder to the anterior peritoneum.
Puncture of the gallbladder was done with a long laparoscopic needle to remove liquid contents to limit leakage during the procedure. The second leash was placed in a similar fashion at the Hartman pouch (Figure 2), and a third leash was placed at the infundibulum. The second and third leashes were used as a marionette for mobilization and exposure during dissection.
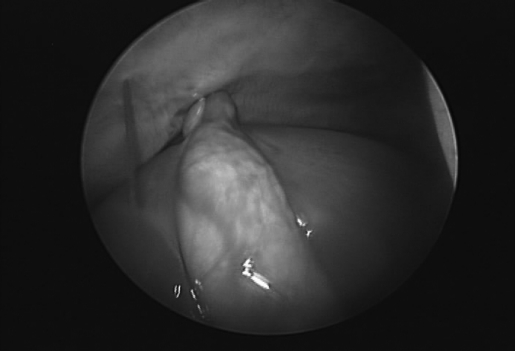
Figure 2.
The placing of the second leash.
The dissection of the cystic duct and artery was done using a Clickline Kelly Dissecting forceps (33421MD, Karl Storz, Germany). Clips were applied through the operating channel (Nonabsorbable Polymer Ligation Clips Hem-o-lok ML, Weck, Triangle Park, NC). Dissection of the gallbladder continued with an insulated hook.
Once the gallbladder was separated from the liver, the gallbladder was held with a leash to the abdominal wall. The specimen was grasped with a 5-mm claw forceps. The leashes were removed. The specimen was gently withdrawn until it reached the intraabdominal tip of the vaginal port. The cannula, laparoscope, and gallbladder were then removed together for final extraction (Figure 3).
Figure 3.
The transvaginal extraction.
The vaginal port was reinserted. Pneumoperitoneum was established and operative laparoscope placed for inspection. Irrigation and suction were carried out through the operating channel. For suction-irrigation, we used 5-mm probes. The incision in the posterior fornix was closed with a 2– 0 chromic suture placed inside the vagina.
The patient tolerated the procedure well and was discharged 24 hours after surgery, as is customary at this hospital for laparoscopic cholecystectomies. The patient had no scars because no abdominal ports were used.
DISCUSSION
Major concerns following the use of the vaginal route are risks of pelvic infection, trauma to adjacent structures, dyspareunia, and cul-de-sac adhesion.2–5 Dr. Tsin et al2 have 10 years of experience (1998 –2008) with culdolaparoscopy; we have not seen any of these complications.
This is consistent with earlier reports demonstrating an extremely low incidence of complications with colpotomy and culdoscopy.
The use of modern, flexible, multifunctional endoscopes with 2 or 3 working channels, as developed for NOTES, has some disadvantages. The devices are not stable enough to allow precise dissection, and, therefore, must be incorporated with a rigid platform. Retraction is also limited, because reliable instruments permitting triangulation are not yet available. Insufflation of the peritoneal cavity through the endoscope is unstable. Vision cannot be guaranteed in the presence of bleeding, and hemostasis is likely to be insecure and slow in execution.
These disadvantages can be overcome with the use of a laparoscope with a working channel through a vaginal port that allows suitable insufflation, precise dissection with strong laparoscopic instruments, and appropriate hemostasis (suture, clips, Harmonic scalpel, LigaSure). Retraction and exposure could be done with marionette leashes.
Dr. Davila et al have performed laparoscopic surgery (cholecystectomy, appendectomy, ovarian cystectomy, hysterectomy) with only one umbilical port since 1997. This experience is an important factor that allows changing the transumbilical to a transvaginal access.
The introduction of this new approach required an IRB that was obtained by Dr. Fausto Davila, the principal investigator. The protocol includes the use of rigid, flexible, and magnetic technology for transvaginal surgeries.
Preparation for the junction of the concepts of culdolaparoscopy with single puncture techniques began in 2005, and the first operations were done in Poza Rica, Veracruz, Mexico in April 2008. The result was transvaginal surgery that used only one vaginal port.
CONCLUSION
The innovations in flexible technology, robotics, and magnets will change the way endoscopy will be performed in the future, and allow for more indications and improvement in the current artisan, labor-intensive natural orifice peritoneoscopies. Minilaparoscopy assisted natural orifice surgery (MANOS) and transvaginal NOTES cholecystectomies will benefit from such advances. Today, such technology is in the early developmental stage; it is not universally available and may not be affordable for most surgeons.7,8 This article presents a case of transvaginal cholecystectomy performed by a skilled team with currently available technology and with no abdominal port.
Contributor Information
Fausto Davila, Hospital Regional, Poza Rica, SESVER, Veracruz, México..
Daniel A. Tsin, The Mount Sinai Hospital of Queens, Long Island City, New York, USA..
Guillermo Dominguez, Sanatorio Mitre, Buenos Aires, Argentina..
Ulises Davila, Hospital Regional, Poza Rica, SESVER, Veracruz, México..
Ramiro Jesús, Hospital Regional, Poza Rica, SESVER, Veracruz, México..
Adriana Gomez de Arteche, Hospital Regional, Poza Rica, SESVER, Veracruz, México..
References:
- 1.Hugness E. The best surgical thinking. Natural orifice surgery: Is it here to stay? ACS Surgery—Principle & Practice. November 2007;1–3 [Google Scholar]
- 2.Tsin DA, Colombero L, Lambeck, Manolas P. Minilaparoscopy-assisted natural orifice surgery. JSLS. 2007;11:24–29 [PMC free article] [PubMed] [Google Scholar]
- 3.Tsin DA, Colombero LT, Mahmood D, Padouvas J, Manolas P. Operative culdolaparoscopy: a new approach combining operative culdoscopy and minilaparoscopy. J Am Assoc Gynecol Laparosc. 2001;8:438–441 [DOI] [PubMed] [Google Scholar]
- 4.Ghezzi F, Raio L, Mueller MD, Gyr T, Buttarelli M, Franchi M. Vaginal extraction of pelvic masses following operative laparos-copy. Surg Endosc. 2002;16:1691–1696 [DOI] [PubMed] [Google Scholar]
- 5.Tsin DA. Culdolaparoscopy: a preliminary report. JSLS. 2001;5:69–71 [PMC free article] [PubMed] [Google Scholar]
- 6.Buess G, Cushieri A. Raising our heads above the parapet: ES not NOTES. Surg Endosc. 2007;21:835–837 [DOI] [PubMed] [Google Scholar]
- 7.Fo Wagh M, Thompson C. Surgery insight; natural orifice transluminal endoscopic surgery. An analysis of work to date. Nat Clin Pract Gastroenterol Hepatol. 2007;4(7):386–392 [DOI] [PubMed] [Google Scholar]
- 8.Christian J, Barrier BF, Miedema BW, Thaler K. Culdoscopy: a foundation for natural orifice surgery past, present and future. J Am Coll Surg. 2008;207:417–422 [DOI] [PubMed] [Google Scholar]