Abstract
Nonparasitic splenic cysts require a totally different type of surgical management than that of parasitic cysts. Three cases of nonparasitic splenic cysts and their surgical management by the open and laparoscopic approaches are presented. The surgical technique and review of the recent literature are discussed to demonstrate the current trends in the operative management of nonparasitic splenic cysts.
Keywords: Laparoscopy, Laparoscopic splenectomy, Laparoscopic deroofing, Partial splenectomy, Splenectomy
INTRODUCTION
Splenic cysts are a relatively rare condition. In 1974, Robbins et al1 reported only 32 cases of splenic cysts in 42 327 splenic autopsies during a period of 24 years. These splenic cysts were incidental postmortem findings.
A splenic cyst can be either primary (true) or secondary (false).2 The main characteristic of primary cysts is their cellular epithelial lining, which is absent in secondary cysts.
Primary splenic cysts are divided into 2 major categories: parasitic and nonparasitic. Although the parasitic cysts are the most common type worldwide accounting for about 60%, in Central Europe and North America nonparasitic cysts are more frequent.1,3 Echinococcus granulosus is the most common cause of a parasitic cyst. On the other hand, nonparasitic splenic cysts are congenital or neoplastic.4 Congenital cysts are divided into epidermoid, dermoid, and endodermoid (simple) cysts. The epidermoid type accounts for 90% of primary nonparasitic cysts.5 Historically, Andral, in 1829, first described a case of splenic dermoid cyst at an autopsy.6
Secondary splenic cysts usually develop after an abdominal trauma (posttraumatic) and less frequently as a result of mononucleosis, tuberculosis, or malaria.7
Parasitic and nonparasitic cysts require an absolutely different management approach because of their dissimilar pathogenesis.
In this report, we describe 3 cases of benign nonparasitic splenic cystic structures and their surgical treatment. Additionally, we discuss the current trends in approach and surgical management of nonparasitic splenic cysts.
MATERIALS AND METHODS
Case Report One
A 55-year-old female complained of chronic intermittent pain in the left upper abdominal quadrant. She had no history of trauma or infection, and her remaining history was unexceptional. The physical examination revealed only normal findings. An abdominal ultrasound study revealed multiple anechoic patterns of a cystic mass (9 × 8 × 5cm) at the lower pole of the spleen. The same findings were confirmed on an abdominal CT scan. Routine blood tests were within normal limits. The Echinococcus-anti-body titer test was negative. We performed an open procedure because of the presence of multiple spaces in the cyst. With the patient under general anesthesia and endotracheal intubation, the abdomen was entered through a left subcostal incision, and a giant splenic cyst containing serous fluid was revealed at the lower pole of the spleen. We performed a total splenectomy, avoiding rupture or aspiration of the cyst. The histology report demonstrated a multicystic structure at the lower pole of the spleen. The definite histological diagnosis was cystic splenic lymphangioma. Pneumococcal vaccine and penicillin were administered postoperatively. The patient had an uneventful postoperative course, and she was discharged on the seventh postoperative day. The patient is in good health 12 years after the initial surgery.
Case Report Two
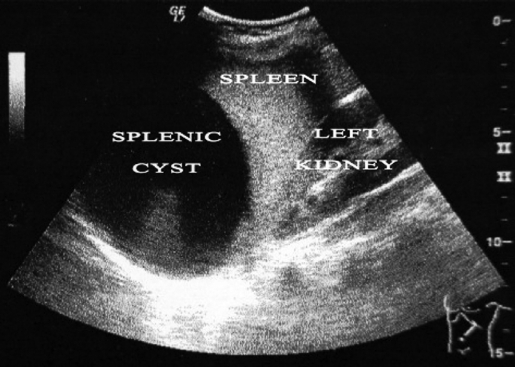
A 12-year-old girl was examined at our department for intermittent dull abdominal pain located mainly in the left upper quadrant. The pain started 1 year prior to the examination. The patient had no history of trauma or infection, and her remaining history was unexceptional. The physical examination revealed only normal findings. There was only the suspicion of a palpable mass in the left upper abdominal quadrant. An ultrasonography of the upper abdomen revealed a cystic mass of the spleen located in the upper pole of the organ. The sonographic characteristics of the cyst were a size of 9 × 8 × 9 cm, with a smooth wall and an anechoic central area (Figure 1). There was no dislocation of the surrounding organs and no abnormal findings from the other abdominal viscera. The routine blood tests were within normal limits. The Echinococcus-antibody titer test was negative.
Figure 1.
Abdominal sonography showing the splenic cyst, the splenic parenchyma, and the left kidney.
Laparoscopic resection of the splenic cyst was considered. Standard preoperative care included prophylactic dosage of antibiotics. The patient was placed in a supine position with her lower extremities in abduction. With the patient under general anaesthesia and endotracheal intubation, a 10-mm laparoscopic trocar was placed in the area below the umbilicus by using the open cut-down technique. A 10-mm Hg to 12-mm Hg pneumoperitoneum was created. Before starting, a thorough video-guided inspection of the peritoneal cavity revealed a large cyst clearly visible on the upper pole of the spleen. A second 5-mm trocar was placed in the midline, approximately 8cm superiorly to the umbilical port. A 5-mm port was placed to the right midclavicular line within the upper quadrant. A pneumatic arm was inserted via this port below the inferior surface of the liver to expand the operating field. A fourth 10-mm trocar was placed parallel to the umbilical port along the left anterior axillary line. A 30o laparoscope was used for better visualization of the upper surface of the spleen. The greater omentum was pulled down, and the cyst was revealed. After the cyst was opened with ultrasonically activated coagulated shears (Ultracision, Ethicon Endo-Surgery, Cincinnati, OH), 1,200mL of yellowish serous fluid was drained (Figure 2). An Endo-grasp forceps and the Ultracision were used to remove the whole extrasplenic wall of the cyst (deroofing), paying attention to protect the splenic parenchyma (Figure 3). The specimen was extracted through the 10-mm umbilical trocar, and a closed drain was placed inside the remaining splenic cyst cavity (Figure 4). The histology report of the cystic specimen shows only the presence of fibrin deposition in the wall without epithelium. For this reason, it was impossible to define the histologic type of cyst. We hypothesized that the cyst was a posttraumatic event despite the absence of a history of trauma. The patient was discharged on the second postoperative day, after an uneventful course. The follow-up ultrasonography of the spleen revealed no recurrence of the cyst 3 years after the resection.
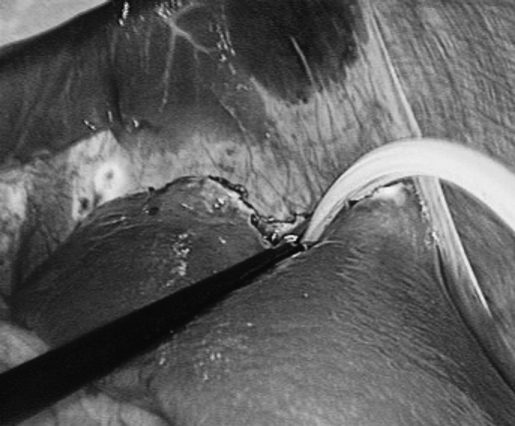
Figure 2.
Yellowish serous fluid was drained after the cyst was opened.
Figure 3.
Removing (deroofing) of the extrasplenic wall of the splenic cyst.
Figure 4.
The drain is placed inside the remaining splenic cyst cavity.
Case Report Three
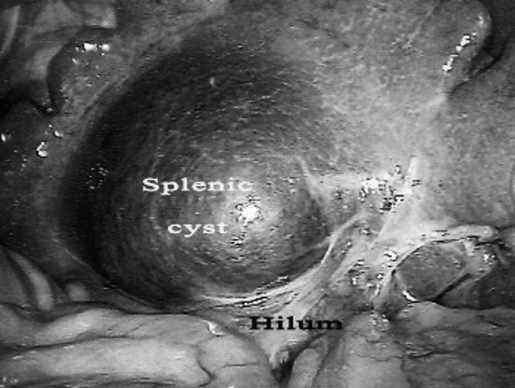
A 44-year-old woman was admitted to our department because of an incidental finding of a splenic mass after a routine abdominal sonogram was performed. The ultrasound demonstrated a splenic cystic mass on the visceral surface of the spleen near to the hilum. The sonographic characteristics of the cyst were a size of 6 × 4 × 3cm, with smooth wall and anechoic central areas. The patient had no history of trauma or infection, and the remaining history was unexceptional. A physical examination revealed only normal findings. Routine blood tests were within normal limits. The Echinococcus-antibody titer test was negative. The strong suspicion of a splenic nonparasitic cyst, the superficial location of the cyst, and the need for spleen preservation led us to perform laparoscopic resection of the cyst (Figure 5). The laparoscopic technique used was the same as that in case report 2. Damage to the splenic parenchyma, near the hilum, during the deroofing of the cyst, resulted in massive bleeding from the spleen. The unsuccessful control of bleeding required conversion of the laparoscopic procedure to an emergent open approach. A total splenectomy was performed through a left subcostal incision, to successfully control the bleeding. The diagnosis of a primary epidermoid splenic cyst was based on the histology report. Pneumococcal vaccine and penicillin were administered postoperatively. The patient was hemodynamically stable during the entire postoperative period, and she was discharged on the ninth postoperative day. She is in excellent health 2 years after the operation.
Figure 5.
Splenic cyst near to the hilum.
DISCUSSION
The rarity of nonparasitic splenic cysts has limited the definition of clear criteria for their treatment. However, a recent review by Hansen and Moller2 was the first that adequately organized and suggested the appropriate options for the treatment of this clinical entity.
Although there is no evidence-based cut-off limit for the selection of treatment, it is well known that asymptomatic nonparasitic splenic cysts <5cm in diameter must be managed conservatively.2,3,8,9 Cysts >5cm must be treated surgically because of the increased risk of complications, such as rupture and infection followed by hemoperitoneum, chemical peritonitis, or abscess formation.2,3,10,11
Especially in the case of posttraumatic splenic cysts, according to Balzan et al,12 cysts should be managed surgically when complications develop or when their diameter is >4cm. At that size, complications are more likely to occur.
Control of the cyst size, prevention of complications, and avoidance of recurrence must be the basic principles of management of splenic cysts. Different types of operative management of nonparasitic splenic cysts are available, including percutaneous drainage, complete splenectomy, partial splenectomy, marsupialization of the cyst, and partial cystectomy (fenestration, unroofing, deroofing). Factors like patient age and the size, location, and nature of the cyst influence the selection of the applied surgical procedure.13
Percutaneous Drainage
Because of the limited number of reports, the application of percutaneous drainage in the treatment of splenic cysts is controversial. In a recent study of 2 cases, Thanos and coworkers14 support the idea that percutaneous drainage along with supplementary alcohol ingestion is a safe, cost-effective, and efficacious modality of treatment that ensures early convalescence and a superior aesthetic result. Conversely, other researchers believe that this method of treatment has the major disadvantage of recurrence, the incidence of which is high.5,10 Additionally, the development of adhesions and the possibility of inflammation around the spleen are important limitations for the physician, especially if a subsequent surgical intervention is required.2 Percutaneous drainage, with or without chemical sclerotherapy, can be used as a preoperative method to decrease the size of large cysts.12
Total Splenectomy
For many years open total splenectomy was the preferred method of treatment for the majority of splenic cysts, as described by Péan in 1867. Nowadays, because of the increased risk of immunodeficiency following the complete removal of splenic tissue, minimally invasive techniques must be used.2,3 Additionally, the greater the preservation of splenic tissue, the greater the benefit for the adult patient, as long as the risk of hemorrhage is not increased. Only under special conditions is it necessary to perform total splenectomy. These indications include the presence of multiple cysts (polycystic cases), very large-sized cyst, the location of the cyst in the hilum of the spleen, the intrasplenic cyst (covered completely by the parenchyma), uncontrollable intraoperative bleeding, and cysts that are inaccessible for fenestration or marsupialization.2,3,13
Laparoscopic total splenectomy is now the preferred operative technique if splenic removal is required.15–17 Since Kum et al18 in 1993 reported the laparoscopically assisted splenectomy, this method has gained the acceptance of surgeons because of its safety.
The simultaneous autotransplantation of splenic tissue has offered optimistic results. The implantation of splenic fragments into areas within portal circulation (usually into greater omentum) results in a relatively adequate functioning of the transplanted tissue.12
Partial Splenectomy
The basic advantage of partial splenectomy is that it has a better outcome than splenic autotransplantation, achieving the conservation of more than 25% of splenic parenchyma.12 This proportion is the minimum sufficient amount for regular immunologic function of the spleen.2 Although partial splenectomy requires great technical skill and full anatomical knowledge of the splenic vascularization, it offers a definite solution in case of splenic cysts of both nonparasitic and secondary causes.3 This kind of operation can be performed when one of the splenic poles is not affected and therefore can remain with preserved parenchyma.19 The main indication is the deep location of the cyst cavity in the splenic parenchyma, which is associated with a high risk of recurrence.10
Laparoscopic partial splenectomy can be safely performed. Although partial splenectomy is usually performed using the open procedure, laparoscopic partial splenectomy has been done successfully.8,20–23 This procedure is mainly recommended if the cyst is located in the poles of the spleen even though deep in the cystic parenchyma10,13,21 and is preferable in recurrent splenic cysts.24 Currently, this procedure is the treatment of choice for these cases, and it would be beneficial if attempted after previous angiography, which offers a full evaluation of splenic vasculature.2
Marsupialization
This technique, first described by Millar in 1982,25 separates the cystic wall from the splenic parenchyma. This separation causes some degree of bleeding that can be safely controlled by diathermia or suture instruments. Marsupialization is recommended for superficial splenic cysts, and it is characterized by a shorter duration of surgery and no risk of recurrence.2,13
Very recent studies support the use of laparoscopic marsupialization, because it is a safe and effective method for nonparasitic cysts (including giant splenic cysts) and should be considered the treatment of choice.13,26,27 Lining of the cyst cavity with Surgicel and omentopexy is a feasible, efficacious method with excellent early and long-term outcomes.28
“Needlescopic” techniques are the newest laparoscopic marsupialization procedures, which remain controversial but may have some application.
Fenestration (Partial Cystectomy, Unroofing, Deroofing)
In this surgical approach, only a segment of the cystic wall is resected, creating an opening for communication between the peritoneal and cyst cavities. The main disadvantage of this procedure is the remaining risk of recurrence. Even if previous reports support the attachment of the omentum over the parenchyma defect as a way of reducing the risk of recurrence, it has not yet been determined how much of the cyst wall should be resected and whether deroofing should be partial or radical. It is believed, however, that removing a large amount of the cyst wall will prevent cyst reclosure (recurrence).2,13,23
With laparoscopic and open fenestration, the risk of recurrence is the same.2 The laparoscopic technique enables the surgeon to determine the precise size and shape of the splenic cyst and to successfully and thoroughly remove the cystic wall, as we did with our patient. Since Salky first introduced laparoscopic fenestration of a nonparasitic splenic cyst in 1985, much experience has been gained, as we can see from the literature.3 Because of the existing risk of recurrence associated with this procedure, more knowledge is needed to establish this technique as the treatment of choice for nonparasitic superficially located splenic cysts.29
CONCLUSIONS
Based on a review of the literature and our limited experience with nonparasitic splenic cysts, we suggest the following principles for optimal surgical treatment:
Surgeons should be familiar with both open and laparoscopic spleen-preserving operative procedures.
Superficially located cysts should be treated by laparoscopic marsupialization or fenestration.
Cysts located deep in the poles of the spleen should be managed by partial splenectomy, which is the treatment of choice. Laparoscopic partial splenectomy should be performed by experienced surgeons.
Cysts located on the posterior surface of the spleen are more difficult to treat laparoscopically and require wide mobilization of the organ.2
Total splenectomy (open or laparoscopic) must be performed only when minimally invasive surgical techniques or operations like partial splenectomy jeopardize the outcome of the procedure.
Generally, laparoscopic spleen-preserving surgery must be the first goal of management of nonparasitic splenic cysts, because it provides all the benefits of minimally invasive surgery and offers adequate safety and acceptable results, especially in experienced hands.
References:
- 1.Robbins FG, Yellin AE, Lingua RW, et al. Splenic epidermoid cysts. Ann Surg. 1978;187(3):231–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hansen MB, Moller AC. Splenic Cysts. Surg Laparosc Endosc Percutan Tech. 2004;14:316–322 [DOI] [PubMed] [Google Scholar]
- 3.Gianoma D, Wildisenb A, Hotza T, et al. Open and laparoscopic treatment of nonparasitic splenic cysts. Dig Surg. 2003;20:74–78 [DOI] [PubMed] [Google Scholar]
- 4.Robertson F, Leander P, Ekberg O. Radiology of the spleen. Eur Radiol. 2001;11:80–95 [DOI] [PubMed] [Google Scholar]
- 5.Cowles RA, Yahanda AM. Epidermoid cyst of the spleen. Am J Surg. 2000;180:227. [DOI] [PubMed] [Google Scholar]
- 6.Andral G. Precis d'Anatomie Pathologique. Paris: Gabon, 1829:432 [Google Scholar]
- 7.Thorvaldson J, Birkeland S. Splenic cysts. Tidsskr Nor Laegeforen. 1981;101:1641–1643 [PubMed] [Google Scholar]
- 8.Tagaya N, Oda N, Furihata M, et al. Experience with laparoscopic management of solitary symptomatic splenic cysts. Surg Laparosc Endosc Percutan Tech. 2002;12:279–282 [DOI] [PubMed] [Google Scholar]
- 9.Pachter HL, Hofstetter SR, Elkowitz A, et al. Traumatic cysts of the spleen–the role of cystectomy and splenic preservation: Experience with seven consecutive patients. J Trauma. 1993;35:430–436 [PubMed] [Google Scholar]
- 10.Smith ST, Scott DJ, Burdick JS, et al. Laparoscopic marsupialization and hemisplenectomy for splenic cysts. J Laparoendosc Adv Surg Tech A. 2001;11:243–249 [DOI] [PubMed] [Google Scholar]
- 11.Boesby S. Spontaneous rupture of benign nonparasitic cyst of the spleen. Ugeskr Laeger. 1972;134:2596–2597 [PubMed] [Google Scholar]
- 12.Balzan SM, Riedner CE, Santos LM, et al. Posttraumatic splenic cysts and partial splenectomy: report of a case. Surg Today. 2001;31(3):262–265 [DOI] [PubMed] [Google Scholar]
- 13.Macheras A, Misiakos EP, Liakakos T, et al. Non-parasitic splenic cysts: a report of three cases. World J Gastroenterol. 2005;11(43):6884–6887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thanos L, Mylona S, Ntai S, et al. Percutaneous treatment of true splenic cysts: report of two cases. Abdom Imaging. 2005;30:773–776 [DOI] [PubMed] [Google Scholar]
- 15.Rosin D, Brasesco O, Rosenthal RJ. Laparoscopic splenectomy: new techniques and indications. Chirurg. 2001;72:368–377 [DOI] [PubMed] [Google Scholar]
- 16.Uccheddu A, Pisanu A, Cois A, et al. Laparoscopic management of non-parasitic splenic cysts. Chir Ital. 2003;55(1):55–60 [PubMed] [Google Scholar]
- 17.Yagi S, Isaji S, Iida T, et al. Laparoscopic splenectomy for a huge splenic cyst without preoperative drainage: report of a case. Surg Laparosc Endosc Percutan Tech. 2003;13:397–400 [DOI] [PubMed] [Google Scholar]
- 18.Kum CK, Ngoi SS, Goh P, et al. A rare wandering splenic cyst removed with laparoscopic assistance. Singapore Med J. 1993;34:179–180 [PubMed] [Google Scholar]
- 19.Sagar PM, McMahon MJ. Partial splenectomy for splenic cysts. Br J Surg. 1998;75:488. [DOI] [PubMed] [Google Scholar]
- 20.Poulin EC, Thibault C, DesCoteaux JG, et al. Partial laparoscopic splenectomy for trauma: Technique and case report. Surg Laparosc Endosc. 1995;5:306–310 [PubMed] [Google Scholar]
- 21.Kaiwa Y, Kurokawa Y, Namiki K, et al. Laparoscopic partial splenectomies for true splenic cysts. A report of two cases. Surg Endosc. 2000;14:865. [DOI] [PubMed] [Google Scholar]
- 22.Seshadri PA, Poulin EC, Mamazza J, et al. Technique for laparoscopic partial splenectomy. Surg Laparosc Endosc Percutan Tech. 2000;10:106–109 [PubMed] [Google Scholar]
- 23.Till H, Schaarschmidt K. Partial laparoscopic decapsulation of congenital splenic cysts. Surg Endosc. 2004;18:626–628 [DOI] [PubMed] [Google Scholar]
- 24.Mertens J, Penninckx F, DeWever I, et al. Long-term outcome after surgical treatment of nonparasitic splenic cysts. Surg Endosc. 2007;21:206–208 [DOI] [PubMed] [Google Scholar]
- 25.Millar JS. Partial excision and drainage of post-traumatic splenic cysts. Br J Surg. 1982;69:477–478 [DOI] [PubMed] [Google Scholar]
- 26.Sierra R, Brunner WC, Murphy JT, et al. Laparoscopic marsupialization of a giant posttraumatic splenic cyst. JSLS. 2004;8(4):384–388 [PMC free article] [PubMed] [Google Scholar]
- 27.Palanivelu C, Rangarajan M, Madankumar MV, et al. Laparoscopic internal marsupialization for large nonparasitic splenic cysts: effective organ-preserving technique. World J Surg. 2008;32(1):20–25 [DOI] [PubMed] [Google Scholar]
- 28.McColl RJ, Hochman DJ, Sample C. Laparoscopic management of splenic cysts: marsupialization, cavity lining with surgicel and omentopexy to prevent recurrence. Surg Laparosc Endosc Percutan Tech. 2007;17:455–458 [DOI] [PubMed] [Google Scholar]
- 29.Mezquita S, Rosado R, Gallardo A, et al. Partial laparoscopic decapsulation of splenic cysts: long-term results. Surg Laparosc Endosc Percutan Tech. 2007;17:49–51 [DOI] [PubMed] [Google Scholar]