Abstract
Objective:
In the past, knot-tying techniques have been evaluated and compared, but there has been a scarcity of objective scoring systems in these comparison studies. Using an objective scoring system, we aimed to compare 3 types of knots: intracorporeal flat-square knots, intracorporeal slip-square knots, and extracorporeal square-knots for their Knot Quality Scores (KQS) and their rates of slippage.
Materials and Methods:
Three surgeons tied 100 knots in the 3 knot categories. The knots tied were evenly distributed amongst the 3 surgeons with each surgeon contributing at least 30 knots. These knots were tied in a nonrandomized fashion. Forces were measured using a tensiometer and an objective scoring system, the Knot Quality Score (KQS), which is used to compare the knot's strength and rates of slippage.
Results:
Median KQS scores of the 3 groups were not all the same. The median KQS and variance for the extracorporeal square knot group was 0.32 and 0.0079, respectively. For the intracorporeal slip-square knot group, the median KQS and variance was 0.28 and 0.00017, respectively. Lastly, for the intracorporeal flat-square knot group, the median KQS and variance was 0.33 and 0.0075, respectively. Follow-up analysis revealed that the KQS medians (0.32 versus 0.28) of the extracorporeal square-knots and intracorporeal slip-square knot groups were significantly different (P<0.0001). The medians of the intracorporeal slip-knot and intracorporeal flat-square knot groups (0.28 versus 0.33) were also statistically significantly different (P<0.0001). There was no statistically significant difference in KQS scores between extracorporeal square-knots and intracorporeal flat-square knots.
Conclusion:
Extracorporeal square-knots and intracorporeal flat-square knots can tolerate better distraction forces and thus have higher median KQS scores compared with intracorporeal slip-square knots.
Keywords: Laparoscopic knots, Square knots, Flat-square knots
INTRODUCTION
The goal in tying a surgical knot is simple: reliably secure in a firm manner. This goal is preserved in any area of medicine where tissue is approximated and secured. Many laparoscopic operations require a surgeon to be skilled in suturing technique if the surgery is to be successful. For example, in laparoscopic Roux-en-Y gastric bypass and Nissen fundoplication, the need to suture and knot laparoscopically is critical. Essentially, no effective substitute for the surgical knot currently exists.1
Several methods of creating laparoscopic knots have been developed, and they include the 2 broad categories of those knots created extracorporeally and those created intracorporeally. Extracorporeal knots are created by removing both ends of suture outside the laparoscopic ports forming the knot outside of the abdominal cavity and using a laparoscopic knot pusher to cinch down and secure each throw of the knot. Intracorporeal knots are formed entirely within the abdomen by using an instrument tie technique. Each of these methods can be subdivided into either flat knots (such as the square, or surgeon's knot) or sliding knots (such as the Roeder knot or the intracorporeal slip-square).
Several studies have compared the breaking strength of each of these laparoscopic knots. Unfortunately, many of these are underpowered and often have just one surgeon tying the knots.2–4 Moreover, none have used an objective scoring system to compare different techniques of tying knots. The Knot Quality Score (KQS) devised by Hanna, Frank, and Cuschieri5 provides an objective formula to reliably assess knot security and reflects the degree of tightening of the knot. In this system, a precision, computer-based knot distracting tensiometer provides a force extension curve from which knot tightening or slippage can be deduced. An equation using the amount of distraction force needed to break the knots then calculates a Knot Quality Score (KQS):
KQS=[(knot breaking or slipping force * integrated for the knot)/(thread breaking force * integrated force for the thread)] *100
In this study, we compared 3 types of knots: intracorporeal flat-square knots, intracorporeal slip-square knots, and extracorporeal square-knots for their knot quality scores and their rates of slippage.
MATERIALS AND METHODS
Three surgeons contributed over 100 knots tied in each of 3 categories. All 3 surgeons were tested using a PicSOR model that identifies spatial abilities and reasoning, and the results suggested similar skill levels. The knots tied were evenly distributed amongst the 3 surgeons with each surgeon contributing at least 30 knots. These knots were tied in a nonrandomized fashion. PicSOR testing is a well-validated test used to predict a surgeon's innate visiospatial abilities.6 Each of the knots was tied in a laparoscopic box trainer on a specially created foam jig. The knot was formed in a ligature that had been previously passed around a foam tube placed inside of a foam block. A 2– 0 silk of a varying length (Tyco Healthcare, Norwalk CT) was used on all of the knots tied by all of the surgeons). The jig was created to ensure a minimum length of 32mm that provides the suture length necessary for the tensiometer (In-Spec 2200, Instron, Canton, MA). The video system consisted of a Sony PVM-20M2MDU (Sony Corp, Tokyo, Japan) Hi-resolution monitor, a Karl Storz Tricam SL NTSC 202221 camera, and Xenon Nova light source along with a Hopkins II zero-degree lens (Karl Storz, Tuttlington, Germany).
Each of the knots was tied using a standardized technique1 with a Jarit needle holder and Hunter graspers (Jarit, Tuttlingen, Germany). The laparoscopic flat square knot was tied by making 4 alternating “squared” throws in an instrument tie fashion.
Although the square knot and surgeons' knot are useful in most situations, they are sometimes insufficient in tissue approximation. Specifically, while the second throw is being looped, the first knot will unravel leaving the first throw to be repeated. The slip-square knot has the advantage of allowing the square knot to be formed before it is cinched down and then converted back into a square knot.
Extracorporeal knots were performed using alternating flat-square throws pushed to the target tissue by an Ethicon ESS 15 knot pusher (Ethicon Endosurgery, Cincinnati, Ohio).
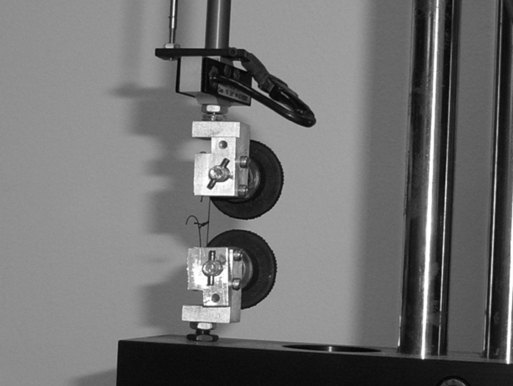
The system for measuring the quality of each of the knots used an Instron In-Spec 2200 Benchtop Tensiometer (Figure 1) and Instron series IX software (Instron, Canton, MA). Load cell signals were filtered to remove high-frequency noise, and distraction was set at 50mm/min. The Instron series IX software was used to calculate Knot Quality Scores (KQS) based on the data retrieved from the resistance generated by the force of distraction.
Figure 1.
The tensiometer with suture placed.
Each of the knots tied around the jig was cut. These knotted sutures were then placed into the In-Spec 2200 tensiometer (Figure 1), and each of the knots was distracted and their KQS, force used for distraction (in Newtons), and slip or break were logged into the database. A knot was defined as a slip if the maximum force caused the knot to fail at the level of the knot. A break was defined if the maximum force caused the knot to rupture at the level of the untied (unknotted) portion of the suture material. Only knots that were broken and did not slip had their KQS recorded.
RESULTS
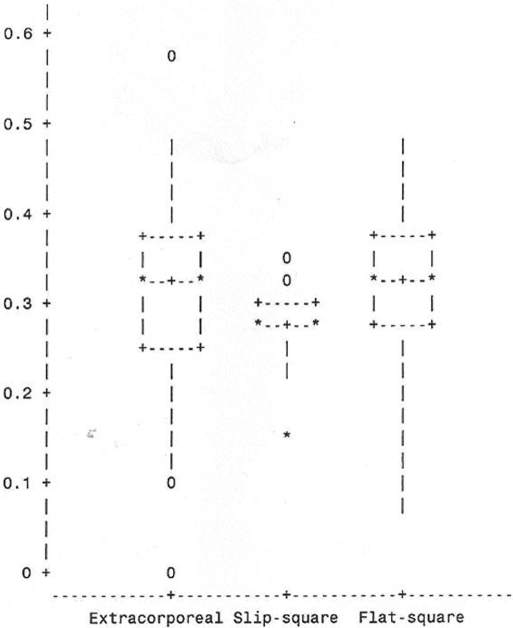
To determine whether there was a significant difference in KQS among the intracorporeal flat-square knots, intracorporeal slip-square knots, and extracorporeal square-knots, the nonparametric analogue of ANOVA, which is called a Kruskal-Wallis test, was used. As Figure 2 shows, there are outliers in the data, and the 3 groups do not appear to have the same KQS variance with the intracorporeal slip-square knots being the least variable. The median KQS and variance for the extracorporeal square knot group were 0.32 and 0.0079, respectively. For the intracorporeal slip-square knot group, the median KQS and variance were 0.28 and 0.00017, respectively. Lastly, for the intracorporeal flat-square knot group, the median KQS and variance were 0.33 and 0.0075, respectively, as described in Table 1.
Figure 2.
A graphical representation of the Knot Quality Score (KQS). It is based on the quartiles of the variable. The rectangular box corresponds to the lower quartile and the upper quartile. The line in the middle is the median.
Table 1.
Comparison of Knot Quality Scores (KQS)
| Extracorporeal Square Knot | Intracorporeal Slip-square Knot | Intracorporeal Flat-square Knot | |||
|---|---|---|---|---|---|
| Quantile | KQS Estimate | Quantile | KQS Estimate | Quantile | KQS Estimate |
| 100% Max | 0.59 | 100% Max | 0.24 | 100% Max | 0.48 |
| 75% Q3 | 0.37 | 75%Q3 | 0.29 | 75% Q3 | 0.39 |
| 50% Median | 0.32 | 50% Median | 0.28 | 50% Median | 0.33 |
| 25% Q1 | 0.26 | 25% Q1 | 0.27 | 25% Q1 | 0.26 |
| 0% Min | 0.00 | 0% Min | 0.14 | 0% Min | 0.09 |
| N | 101 | N | 100 | N | 105 |
| Variance (+/-) | 0.0079 | Variance (+/-) | 0.00017 | Variance (+/-) | 0.0075 |
The Kruskal-Wallis test statistic is 25.76 (P<0.0001). This suggests that the median KQS of the 3 groups are not all the same. Follow-up analysis reveals that the medians (0.32 versus 0.28) of the extracorporeal square-knots and intracorporeal slip-square knot groups are significantly different (P<0.0001) (Table 1). The medians of the intracorporeal slip-knot and intracorporeal flat-square knot groups (0.28 versus 0.33) are also statistically significantly different (P<0.0001) (Table 1). However, the sample medians (0.32 versus 0.33) of the extracorporeal square-knots and flat-square knots are not statistically significantly different (P=0.47) (Table 1).
In comparing the medians of the 3 groups, we applied the Bonferroni adjustment and test at α/3 = 0.05/3 = 0.016 significance level.
DISCUSSION
Most surgical procedures comprise several simple tasks that when sequenced together form a larger, more complex procedure. Although we often focus on quality outcomes of the complete procedure, simpler components are more readily and rigorously testable. The quality of a tied knot is easily taken for granted. In this study, we sought to assess the quality of the tied knot by using each of the 3 techniques. Previous studies1,3,4 have compared results of different techniques of laparoscopic knot tying. Unfortunately, most of these studies use either too few knots ranging from 5 to 30 or too many different sutures.
In this study, our scope was limited: 100 of each of 3 different knots were tied by a pool of 3 different but equally qualified surgeons using the same brand and type of suture and the same tying instruments. The difference of the KQS between both intra- and extracorporeal square knots was negligible. The difference, however, between either of these knots compared with a slip-square was significant. We attribute this difference to the following reasons. The first is that a slip-to-square knot requires more manipulation upon the suture material creating weaknesses in the fiber of the 2– 0 silk ties. Additionally, the process of cinching down and tightening and retightening can lead to increased weakness.
Unfortunately, the results do not accurately account for the variability between surgeons. Because the knots were done in a nonrandomized fashion by the 3 surgeons, a potential for bias occurs, given potential variations in skill and fatigue. However, the potential fatigue of tying the knots was offset, given that these knots were done on a machine in a low stress, relaxed atmosphere without time pressures. Additionally, when the knots were pooled, the surgeon tying a knot was not recorded. Admittedly, patients who were treated by one surgeon may yield more similar responses than those who were treated by another surgeon. A study that properly takes into account the correlated nature of the data might report different results. While some can argue that each surgeon should be assessed for variability within each of the 100-knot pools, it should be noted that the one technique that the test deemed inferior to the other 2 is the technique with the least variability. We also believe that the surgeons' abilities measured by PicSOR and the number of trials (100 in each group) may make variability less of an issue.
The other question that needs to be raised is in regard to clinical significance. Although it may be possible to say that an intracorporeal square is of a better quality than a slip-square knot; it is possible that the quality of a slip-square knot is still good enough to do the job it was intended to do, thus making the difference found here academic. What is needed then is the creation of a model that will allow surgeons to determine the minimum KQS needed to appose 2 edges of tissue and maintain this apposition under physiologic conditions. This would give any data about the relevance of knot strength a robust clinical direction and set a benchmark for all surgeons who wish to incorporate techniques of laparoscopic suturing into their practice.
Nonetheless, out results using KQS measurements underline the fact that it takes more force and distraction to break knots tied using the extracorporeal square knot and intracorporeal flat-square techniques compared with the intracorporeal slip-square knot technique. While these knots were tied in a laboratory versus in the in-vivo setting, the risk of knots breaking in the operating room likely increases with time and operating setting pressures. This may logically favor using knot techniques that have higher knot quality scores in the lab in an effort to hedge the likelihood against knot breakage in the patient.
CONCLUSION
Given our results, intracorporeal flat-square knots and extracorporeal square-knots can tolerate greater distraction forces than intracorporeal slip-square knots when tested in laboratory settings. Further clinical studies with patients postsurgical follow-up are needed to determine true outcome differences between the suture tying techniques.
Contributor Information
Elie A. Goldenberg, Concord Hospital, Dartmouth Clinic, Concord, New Hampshire, USA..
Abhishek Chatterjee, Dartmouth Hitchcock Medical Centre, Lebanon, New Hampshire, USA..
References:
- 1.Amortegui JD, Restrepo H. Knot security in laparoscopic surgery. A comparative study with conventional knots. Surg Endosc. 2002;16(11):1598–1602 [DOI] [PubMed] [Google Scholar]
- 2.Menenakos E, Nassiopoulos K, Pavlidis T, Petropoulos P. Endokomvos: a simple and secure intracorporeal laparoscopic knot. JSLS. 2004;8(2):207–209 [PMC free article] [PubMed] [Google Scholar]
- 3.Moreno M, Magos FJ, Arcovedo R, et al. Comparison of the performance of the Gea extracorporeal knot with the Roeder extracorporeal knot and the classical knot. Surg Endosc. 2004;18(1):157–160 [DOI] [PubMed] [Google Scholar]
- 4.Patsalos C, Karavias D, Stavropoulos M, et al. The relationship between five kinds of laparoscopic knots and five types of suture materials and histological findings in tissues: an experimental study on rabbits. Surg Laparosc Endosc Percutan Tech. 2003;13(3):202–207 [DOI] [PubMed] [Google Scholar]
- 5.Hanna GB, Frank TG, Cuschieri A. Objective assessment of endoscopic knot quality. Am J Surg. 1997;174(4):410–413 [DOI] [PubMed] [Google Scholar]
- 6.Gallagher AG, Cowie R, Crothers I, Jordan-Black JA, Satava RM. PicSOr: an objective test of perceptual skill that predicts laparoscopic technical skill in three initial studies of laparoscopic performance. Surg Endosc. 2003;17(9):1468–1471 [DOI] [PubMed] [Google Scholar]