Abstract
Objective:
Currently, robotic training for inexperienced, practicing surgeons is primarily done vis-à-vis industry and/or society-sponsored day or weekend courses, with limited proctorship opportunities. The objective of this study was to assess the impact of an extended-proctorship program at up to 32 months of follow-up.
Methods:
An extended-proctorship program for robotic-assisted laparoscopic radical prostatectomy was established at our institution. The curriculum consisted of 3 phases: (1) completing an Intuitive Surgical 2-day robotic training course with company representatives; (2) serving as assistant to a trained proctor on 5 to 6 cases; and (3) performing proctored cases up to 1 year until confidence was achieved. Participants were surveyed and asked to evaluate on a 5-point Likert scale their operative experience in robotics and satisfaction regarding their training
Results:
Nine of 9 participants are currently performing robotic-assisted laparoscopic radical prostatectomy (RALP) independently. Graduates of our program have performed 477 RALP cases. The mean number of cases performed within phase 3 was 20.1 (range, 5 to 40) prior to independent practice. The program received a rating of 4.2/5 for effectiveness in teaching robotic surgery skills.
Conclusion:
Our robotic program, with extended proctoring, has led to an outstanding take-rate for disseminating robotic skills in a metropolitan community.
Keywords: Prostatectomy, Robotics, Extended-proctoring, Education
INTRODUCTION
Robot-assisted laparoscopic radical prostatectomy is becoming an increasingly performed operation in the United States. In 2007, 60% of all radical prostatectomies in the United States were performed robotically.1 As the evidence for the clinical advantages of robotic surgery continues to be collected, the demand for training will continue to increase. Traditionally, robotic training has been completed at weekend courses. Fewer than 50% of participants of Intuitive Surgical's 2-day robotic training course perform robotic prostatectomies when surveyed afterwards. (Intuitive Surgical, personal communication, January 2009). The group at the University of California Irvine described a more extensive 5-day robotics mini-fellowship. With lectures, tutorials, surgical case observation, and inanimate, animate, and cadaveric robotic skill training, Gamboa et al2 report that 78% of the 47 participants of the mini-fellowship were performing robotic prostatectomies at 1-year, 78% at 2-year, and 86% at 3-year follow-up.
Training postgraduate urologists (PGUs) to perform robot-assisted laparoscopic urological procedures should be no different from training urology residents. Both require a motivated learner, a motivated trainer, a curriculum with clear learning objectives, and access to a training robot. Additionally, access to an environment that stimulates learner-centered training with a graduated sense of responsibility would be ideal, but is logistically challenging, especially for surgeons in practice. With these general principles in mind, our institution developed an extended-mentorship program for PGUs practicing in the Minneapolis and St. Paul metropolitan region. This program was designed to train PGUs robotic-assisted laparoscopic techniques with access to laparoscopic-robotic trained endourology fellows and staff.
The objectives of this study were to determine whether such a training model would1 provide basic and durable robotic skills for urologic surgeons in our community and2 influence the adoption of these skills into their practice. A secondary goal of this study was to test the viability of a partnership between a university urology program and local community urology practices.
No outside funding was required for this study. Our institution did not require a training fee to use its facilities or faculty expertise.
METHODS
Nine urologists participated in the extended mentorship program. The director of this extended mentorship program was oncology fellowship-trained and certified by Intuitive Surgical to teach robot-assisted laparoscopic surgical skills. Our institution is 1 of 21 Intuitive Surgical licensed training sites with faculty experts performing da Vinci robot-assisted procedures. Our institution is also 1 of 36 institutions in the United States offering an endourology fellowship. It also has an oncology fellowship available.
All PGUs participating in this program referred their patients to our institution's hospital for their procedures. Our hospital provided all trainees with operating privileges. The endourology and oncology fellows, in conjunction with the trainees, provided postoperative care and management to the trainees' patients. Proctors performing the cases at the console billed the surgeon's fees for the required 5 cases to 6 cases, while outside urologists billed surgeon's fees for the cases they performed as primary surgeon.
The extended-proctoring program was divided into 3 major phases. The first phase required all participants to complete the standard Intuitive Surgical training course for robot-assisted laparoscopic surgery. The training consisted of two 8-hour sessions providing presentations orienting trainees to the robot and step-by-step instructions on the use of the first-generation da Vinci robot on a porcine lab model. Four tasks were required of each trainee in the lab1: dissection of porcine renal hilar vessels followed by ligation,2 porcine laparoscopic nephrectomy on contralateral side,3 cystostomy and closure,4 urethrovesical anastomosis. The trainees were provided time to familiarize themselves with the console, practice camera, and clutching navigation, and observe the setup of the robot.
In the second phase of the program, each trainee was required to assist the proctor in 5 to 6 robotic-assisted laparoscopic prostatectomies (RALP). During this phase, the trainee referred their patients to the proctor, the director of our institution's robotics training program. Each patient consented with the understanding that the proctor was primary surgeon during these 5 to 6 cases, and that he would provide guidance to the trainee during the case both as an assistant, and when the trainee performed graduated and increasing primary console surgeon maneuvers.
In the third phase of the program, the trainees were provided progressively more autonomy to control the console until they felt confident. Fellows trained to competence eventually served as proctors during this final phase for newer trainees. The proctors assisted the trainees in these cases and provided feedback throughout the case. While performing the initial few cases, the trainee would switch from controlling the console to assisting the proctor until confidence was achieved. A “learner-centered” practical curriculum progressed from easier steps towards more technically difficult steps of the operation. It started with competence in port placement and patient positioning. Once this was demonstrated comfortably, the trainee performed the task of taking down of the bladder, followed by opening the endopelvic fascia, followed by exposure and ligation of the dorsal vein, followed by performing the urethrovesical anastomosis, followed by division of the anterior bladder neck, followed by the posterior bladder neck/seminal vesicles, and finally the pedicles and nerve-sparing techniques. As the trainees' experience and surgical volume increased, more console time was provided by the proctors.
In November 2007, all 9 trainees were contacted and completed a standardized survey evaluating their satisfaction with their training on a 5-point Likert scale (Appendix 1). A score of 1 was equivalent to “very ineffective,” while a score of 5 was “very effective.” The survey also investigated whether the trainee was performing RALP, the cumulative number of cases performed up to that time, the postresidency year of trainee, and whether the trainee was practicing in a private group or an academic center.
RESULTS
Between January 2005 and November 2007, 4 PGUs, 3 fellows (EFs), and 2 junior urology faculty (Fs) participated in the extended-proctoring experience at our institution. All 9 participants responded to a follow-up phone survey conducted in November 2007. The phone survey was conducted anywhere from 5 months to 32 months after the participants had enrolled in the extended-proctoring. Table 1 summarizes the background characteristics of the 9 participants.
Table 1.
Background Characteristics of 9 Participants Before Entry Into Robotics Training Program
| Participants* | PGU1 | PGU2 | PGU3 | PGU4 | EF1 | EF2 | EF3 | F1 | F2 |
|---|---|---|---|---|---|---|---|---|---|
| Sex | M | M | M | M | M | M | M | M | M |
| Postresidency Year | 25 | 2 | 5 | 17 | 1 | 1.4 | 1.5 | 4.5 | 4 |
| Experience With RALP | N | N | N | N | N | N | N | N | N |
| Access to a da Vinci robot? | N | N | N | N | N | N | N | N | N |
| Laparoscopic Fellowship Trained? | N | Y | N | N | N | N | N | N | Y |
PGU = postgraduate urologist; EF = endourology fellow; F = junior faculty.
All 3 of the endourology fellows had received laparoscopic training prior to beginning the robotics training. However, only 1 (F1) of the 9 participants had any prior experience with Intuitive Surgical's da Vinci robot (3 pyeloplasties). The mean time from graduation from urology residency was 6.8 years (range, 1 to 25). The mean number of cases proctored for the PGUs, endourology fellows, and junior faculty was 21, 58, and 13, respectively. The endourology fellows, by nature of their position, received the most proctoring.
To assess the significance of long-term proctoring, each participant reported the minimum number of cases required by them to achieve independence. The mean number reported during phase 3 (trainee acting as primary surgeon) was 20.1 cases (range, 5 to 40).
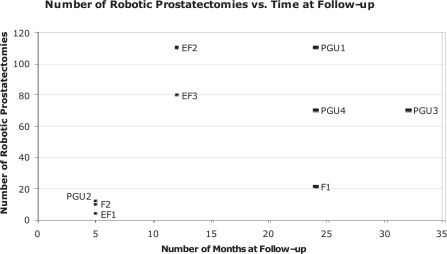
Four of 9 participants are practicing in an academic tertiary center, and 5 are practicing in private urology groups. Six of 9 participants completed the program with a partner in their practice. Currently, 100% of program participants perform RALP in their practice. At the time of the writing of this article, graduates of the program had performed 477 RALPs. Among all 9 trainees, follow-up from completion of robotic training ranged from 5 months to 32 months. Figure 1 summarizes the number of robotic prostatectomies performed by each trainee versus the number of months at follow-up.
Figure 1.
Number of prostatectomies vs. time at follow-up for all 9 trainees.
All 9 trainees have access to at least one da Vinci robot today. The range of the number of robots available to trainees was 1 to 4.
All participants of the extended-proctoring program were asked whether they believed a da Vinci virtual reality trainer would have been useful during their extended-proctoring. Eight of 9 participants believed that a virtual reality trainer would have increased their familiarity with the actual robot, improved their confidence at the console, and would have been useful during their residency training.
Overall, the program was determined to be between “effective” and “very effective” with a mean score of 4.2/5. It was 4, 4.7, and 4 for the PGUs, fellows, and junior faculty, respectively.
DISCUSSION
A primary training outcome metric reported by mini-fellowship programs focused on teaching RALP is the takerate,2 or the rate of trainees incorporating the newly learned technique into clinical practice. While our institution's robotics program included lectures, animal laboratory experience with the robotic interface, and assistance on live surgical cases, the truly unique part of the program consisted of the establishment of an environment for “extended” proctored learner-centered graduated sense of responsibility, much like one would have during a dedicated residency or fellowship. With this curriculum, our take-rate was 100% with a range of 5 months to 32 months of follow-up. Intuitive Surgical's training course is considered among the most comprehensive in the minimally invasive industry, yet even still, the standard take-rate after the da Vinci course has been estimated to be <50%. UC Irvine's mini-fellowship trainees reported by Gamboa et al2 were 78%, 78%, and 86% at 1 to 3 years of follow-up, respectively, and the take-rate of the University of Iowa's intensive 2-day laparoscopy course's trainees reported by Colegrove et al3 was 54% at 5 years.
Similar to the laparoscopic urology training curriculum described by Rane,4 our institution's training curriculum involved the same sequence and composition of phases, including1 completion of an animal laboratory course,2 assisting the mentor on cases,3 performing cases with mentor's assistance until confidence was achieved. The take-rate of Rane's trainees was 100% at up to 3-year follow-up. We agree with Rane's assertion that the main obstacle to the acquisition of laparoscopic skills for a novice laparoscopist is the lack of readily available mentors and long-term proctoring. Training PGUs naïve to laparoscopy requires substantial time commitment from both the mentor and trainee, as evidenced by the fact that some of our trainees continued to participate in the program at our institution up to 1 year after completing phase 2. Although Rane4 describe lack of concentrated surgical volume as one pitfall of such a training model, we were fortunate to train established PGUs in busy clinical practices whose training did not suffer from low caseloads.
Corica et al5 provided evidence that having 2 surgeons collaborate together to learn a new surgical technique in a supportive environment is critical to incorporating laparoscopy into a surgeon's armamentarium. Specifically, trainees who attended Corica's laparoscopic renal surgery training program with a colleague had a 100% take-rate, whereas those who did not had a 77% take-rate at 8-month follow-up. Moreover, Gamboa et al2 recommend that all trainees applying to their robotics training program attend with a colleague. Six of the 9 trainees from our institution completed the robotics training in concert with a colleague from their home institution, and these 3 pairs of trainees continued to collaborate with each other at their home institution. Our institution's take-rate of 100% may reflect these interesting educational effects reported by both Corica et al5 and Gamboa et al.2
Marguet et al6 at Duke reported the take-rates of proctored vs. unproctored trainees in their hand-assisted laparos-copy (HAL) course at 6-month follow-up. The proctored trainees had a 93% take-rate, whereas the unproctored trainees had a 44% take-rate for HAL, a statistically significant difference. In a study measuring the impact of residency training in laparoscopy on subsequent urology practice patterns, Shay et al7 reported the take rates of PGUs with laparoscopic training in residency to be 69%, whereas that of PGUs who had participated in laparoscopic courses with no prior residency training was 48%. The results reported by both Marguet et al6 and Shay et al7 demonstrate a direct relationship between proctoring trainees and the subsequent take-rate. Consistent with these results, the extended-proctoring component of our institution's robotics training likely contributed to the 100% take-rate of our trainees.
In addition to contributing to a high take-rate, at face value, extended-proctoring may help reduce the learning curve of the trainee in a manner that is more safe and effective for the patient. Further studies including an analysis of patient outcomes, however, would have to be performed to determine this conclusively. Fabrizio et al8 demonstrated that the learning-curve of a fellowship-trained laparoscopist naïve to laparoscopic radical prostatectomies was cut down by at least 50% after assisting the expert proctor for 12 cases followed by performing 18 cases while the proctor assisted. More importantly, the trainee learned laparoscopic radical prostatectomy safely as there were no statistical differences in operative time, blood loss, complications, or recovery when the proctor was primary surgeon or when the trainee was primary surgeon. Participating junior faculty had a lower number of cases to perceived competency compared with PGUs and EFs. This is likely explained by the fact that one had some robotic experience (pyeloplasties) and the other was already performing laparoscopic radical prostatectomies before becoming a trainee. Cadeddu et al9 reported that the rate of complications among trainees who had at least 12 months of training in urological laparoscopy before beginning clinical practice did not change when the initial 20, 30, and 40 cases per surgeon were compared with all subsequent cases. These results provide evidence that intensive training shortens the learning curve for laparoscopy. Our institution's trainees underwent more intensive training in robotics surgery because the extended-proctoring program provided supplemental surgical experience to the trainees. Such extended-proctoring provided ample time for trainees to master each step of the RALP, including the most challenging posterior bladder neck and nerve-sparing steps. More importantly, extended-proctoring allowed the endourology fellows an opportunity to teach advanced robotics skills to newer trainees, an important phase of advanced skill acquisition towards the development of skills mastery.
Reporting the same 100% take-rate as Shalhav et al,10 our program was designed to provide postgraduate urologists with robotic surgical techniques in a collaborative and supportive environment. The results of this study, like that of Shalhav et al,10 demonstrate that laparoscopic-trained proctors at academic centers of excellence have a duty to train their postgraduate colleagues with safe and durable robotic surgical skills. Such cooperation is essential to disseminating robotic laparoscopy to PGUs, and sets a high quality standard in the community at large.
The cumulative number of robotic prostatectomies performed by the 9 graduates, 477, reflects not only the effectiveness of our institution's training program, but also the economic pressures to perform a sufficient number of cases to justify the purchase of a da Vinci robot. Steinberg et al11 reported that 78 robotic prostatectomies per year are needed to cover the cost of a $1.5 million da Vinci robot. They also reported that profits are not possible when fewer than 25 robotic prostatectomies are performed annually. Furthermore, they suggest that surgeons converting from open to robotic prostatectomy need to increase their caseloads to cover the added costs of the robot.11
This study has several limitations. The survey is retrospective and did not directly look at the operative reports or case logs. Thus, the study was susceptible to recall bias on the part of the participating surgeon. Another study evaluating the clinical outcomes of patients treated by trainees of our institution is being performed and will also compare the rate of complications of proctor as primary surgeon versus trainee as primary surgeon. Another area of possible concern is that a follow-up of up to 32 months is not as significant as 5 years, and that this shorter follow-up may have contributed to the high take-rate we report. Although this training program was tuition-free, it is difficult to estimate the costs to an academic center in organizing such a robotic training program because many working hours, both proctor and trainee, dedicated to this program were not tracked. As such, a separate study must be performed to calculate the costs in administering such a training program.
CONCLUSIONS
The described extended-proctoring program's 100% takerate and high effectiveness reflects a successful partnership between an academic center of excellence and its local community. Such a model deserves further study in robotics and other new surgical techniques.
The demand for the acquisition of robotic skills may have contributed substantially to our positive results. We cannot ignore the budgetary influence involved with the purchase of a da Vinci robot either. The purchase of a robot is a significant financial commitment for an institution that may have stifled even the most motivated practitioner from applying his new skills, and such a program may allow them an opportunity to apply and develop their skills during the period of time between training and capital acquisition.
The high take-rate and training satisfaction reported here provide more evidence for a viable training model that focuses on the greater well-being of its local community by providing extensive robot-assisted laparoscopic training to urologists motivated to learn robotic surgery. Continued follow-up will ultimately determine the long-term effectiveness of our extended-proctoring program.
Contributor Information
Hossein Mirheydar, Department of Urologic Surgery, University of Minnesota, Minneapolis, Minnesota, USA..
Marklyn Jones, Denver, Colorado, USA..
Kenneth S. Koeneman, Department of Urologic Surgery, University of Minnesota, Minneapolis, Minnesota, USA..
Robert M. Sweet, Department of Urologic Surgery, University of Minnesota, Minneapolis, Minnesota, USA..
References:
- 1.Wexner SD, Bergamaschi R, Lacy A, et al. The current status of robotic pelvic surgery: results of a multinational interdisciplinary consensus conference. Surg Endosc. 2009;23:438–443 [DOI] [PubMed] [Google Scholar]
- 2.Gamboa AJR, Santos RT, Sargent ER, et al. Long-term impact of a robot assisted laparoscopic prostatectomy mini fellowship training program on postgraduate urological practice patterns. J Urol. 2009;181:778–782 [DOI] [PubMed] [Google Scholar]
- 3.Colegrove PM, Winfield HN, Donovan JF, Jr., et al. Laparoscopic practice patterns among North American urologists 5 years after formal training. J Urol. 1999;161:881. [PubMed] [Google Scholar]
- 4.Rane A. A training module for laparoscopic urology. JSLS. 2005;9:460–462 [PMC free article] [PubMed] [Google Scholar]
- 5.Corica FA, Boker JR, Chou DS, et al. Short-term impact of a laparoscopic “mini-residency.” Experience of postgraduate urologists' practice patterns. J Am Coll Surg. 2006;203:692–698 [DOI] [PubMed] [Google Scholar]
- 6.Marguet CG, Young MD, L'Esperance JO, et al. Hand assisted laparoscopic training for postgraduate urologists: the role of mentoring. J Urol. 2004;172:286–289 [DOI] [PubMed] [Google Scholar]
- 7.Shay BF, Thomas R, Monga M. Urology practice patterns after residency training in laparoscopy. J Endourol. 2002;16:251–256 [DOI] [PubMed] [Google Scholar]
- 8.Fabrizio MD, Tuerk I, Schellhammer PF. Laparoscopic radical prostatectomy: decreasing the learning curve using a mentor initiated approach. J Urol. 2003;169:2063–2065 [DOI] [PubMed] [Google Scholar]
- 9.Cadeddu JA, Wolfe JS, Jr., Nakada S, et al. Complications of laparoscopic procedures after concentrated training in urological laparoscopy. J Urol. 2001;166:2109–2111 [PubMed] [Google Scholar]
- 10.Shalhav AL, Dabagia MD, Wagner TT, Koch MO, Lingeman JE. Training postgraduate urologists in laparoscopic surgery: the current challenge. J Urol. 2002;167:2135–2137 [PubMed] [Google Scholar]
- 11.Steinberg PL, Merguerian PA, Bihrle W, Heaney JA, Seigne JD. A da Vinci robot system can make sense for a mature laparoscopic prostatectomy program. JSLS. 2008;12:9–12 [PMC free article] [PubMed] [Google Scholar]