Abstract
Introduction:
Acute inguinal hernias are a common presentation as surgical emergencies, which have been routinely managed with open surgery. In recent years, the laparoscopic approach has been described by several authors but has been controversial amongst surgeons. We describe the laparoscopic approach to incarcerated/strangulated inguinal hernias based on a review of the literature with regards to its feasibility in laparoscopically managing the acute hernia presentation.
Methods:
A systematic literature search was carried out including Medline with PubMed as the search engine, and Ovid, Embase, Cochrane Collaboration, and Google Scholar databases to identify articles reporting on laparoscopic treatment, reduction, and repair of incarcerated or strangulated inguinal hernias from 1989 to 2008.
Results:
Forty-three articles were found, and 7 were included according to the inclusion criteria set. Articles reporting on the use of laparoscopy for the evaluation of the hernia but not reducing and repairing it, the use of the open technique, elective hernia repairs, pediatric series, review articles, and other kinds of hernias were excluded after title and abstract review. This resulted in 16 articles that were reviewed in full. Of these 16 articles, 7 reported on the use of the laparoscopic approach exclusively. From these 7 studies, there were 328 cases reported, 6 conversions, average operating time of 61.3 minutes (SD±12.3), average hospital stay of 3.8 days (SD±1.2), 34 complications (25 of which were reported as minor), and 17 bowel resections performed either laparoscopically or through a minilaparotomy incision guided laparoscopically.
Conclusion:
The laparoscopic repair is a feasible procedure with acceptable results; however, its efficacy needs to be studied further, ideally with larger multicenter randomized controlled trials.
INTRODUCION
Inguinal hernias are common presentations to general surgery clinics when they are reducible and to the emergency unit when they incarcerate or strangulate. Elective surgery for inguinal hernia has a very low mortality (<1 death per 10000 operations).1 In contrast, the risks of postoperative complications following emergency surgery are high, and in elderly patients, mortality can be as high as 5%.1,2 The probability of the hernia getting incarcerated varies in the literature from 0.29% up to 2.9%.3 The classical approach to such presentations is open surgery where the hernia is reduced after induction of anesthesia and muscle relaxation, or during the surgery where the sac is dissected or the hernia defect is widened. The laparoscopic approach remains contentious and even controversial, but few studies in the literature outline the pioneers in reporting this approach with Watson et al4 being the first to report a reduction of the hernia and bowel resection laparoscopically in 1993. After that, several authors explored the feasibility of using this approach for incarcerated and strangulated groin hernias.
This study carries out a systematic review of the literature to assess the use of a laparoscopic approach in managing such cases and to assess its safety and feasibility.
METHODS
A literature search included Medline with PubMed as the search engine, and Ovid, Embase, Cochrane Collaboration, and Google Scholar databases to identify articles reporting on laparoscopic treatment, reduction, and repair of incarcerated or strangulated inguinal hernias from 1989 to 2008. The following Mesh search headings were used: laparoscopy hernia, strangulated hernia, incarcerated hernia, irreducible hernia, groin hernia, inguinal hernia, emergency hernia, and acute hernia. The “related articles” function was used in PubMed to broaden the search, and all titles, abstracts, studies, and citations scanned were reviewed. Then the references of the articles that the search yielded were also reviewed; the latest search was April 23, 2008.
Inclusion criteria were that the English-language manuscript should report on a series of patients who had presented with acute, strangulated, incarcerated, or irreducible inguinal hernias and were managed on an emergency basis using a laparoscopic approach irrespective of whether totally extraperitoneal (TEP) or transabdominal preperitoneal (TAPP). Manuscripts reporting on the open approach, laparoscopy for evaluation of bowel viability only, pediatric, laparoscopic approach for nonacute elective presentations, laparoscopic approach for other types of hernias, and joint approaches (laparoscopy with others) as pooled data were all excluded.
Data extraction of the following variables was performed: author, year, country where study was performed, type of laparoscopic approach, number of cases, conversion rate, operative time, hospital stay, complications, recurrences, manual reduction versus laparoscopic reduction, and the necessity for bowel resection (laparoscopic vs open).
RESULTS
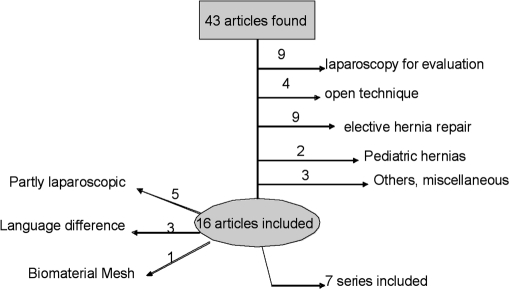
A total of 43 articles were found that sited the use of the laparoscopic approach for the management of acute hernias (Figure 1). Nine articles reported on the use of laparoscopy for the evaluation of the hernia and its contents but not reducing and repairing the hernia, 4 articles reported on the open technique for the repair, 9 articles were reports of laparoscopic elective hernia repairs, 2 were reports of pediatric series, 1 was a review article, and 2 were reports of other kinds of hernias and therefore were excluded after title and abstract review. This resulted in 16 articles that were reviewed in full.
Figure 1.
Flow chart of the articles identified and included.
Out of these 16 articles, 7 reported on the use of the laparoscopic approach exclusively. Five of the 16 were reports of laparoscopic repairs with a few numbers in the cohort being acute hernias, 3 were in languages other than English, and 1 reported on the use of biomaterial as mesh reinforcement and not the usual synthetic meshes available on the market. Therefore, 7 studies reported on the use of laparoscopy exclusively for the management of the acute hernias. Table 1 outlines the details of the studies included. Table 2 outlines the complications extracted in more detail.
Table 1.
Included Studies With Their Respective Data
| Country | Author | Publication Year | Approach | No. of Patients | Conversion Rate (%) | Operative Time (min) | Length of Stay | Complications | Intraoperative Resection* |
|---|---|---|---|---|---|---|---|---|---|
| USA | Ferzli | 2004 | TEP | 11 | 27.2 | 50 | 5.4 | 2 | 1 |
| Germany | Leibl | 2001 | TAPP | 194 | 0 | 55 | NA | 7 | 6 |
| India | Saggar | 2005 | TEP | 34 | 0 | 84.4 | 30 < 2 days | 23 minor | NA |
| Japan | Ishihara | 1996 | TAPP | 6 | 0 | 88 | NA | 1 | NA |
| Italy | Legnani | 2007 | TAPP | 9 | 0 | 72 | 2.7 | 0 | 1 |
| Italy | Rebuffat | 2006 | TAPP | 28 | 10.7 | 72 | 3.9 | 1 | 9 |
| Germany | Mainik | 2005 | TEP | 46 | NA | NA | 4.7 | NA | NA |
| Total | 7 | — | — | 328 | 6 | — | — | 34 | 17 |
Table 2.
Complications Stratified by Author
| Complication | Ferzli | Leibl | Saggar | Ishihara | Rebuffat | Total |
|---|---|---|---|---|---|---|
| Infected Mesh | 1* | 1 | — | — | — | 2 |
| Wound Infection | 1 | — | — | — | — | 1 |
| Intraoperative injury | 1* | 2 | — | — | — | 3 |
| Reoperation | 1* | 1 | — | 1 | — | 3 |
| Thrombosis | — | 1 | — | — | — | 1 |
| Cord induration | — | — | 11 | — | — | 11 |
| Scrotal hematoma | — | — | 6 | — | — | 6 |
| Cord seroma/hematoma | — | — | 4 | — | 1 | 5 |
| Urinary retention | — | — | 2 | — | — | 2 |
| Others | — | 2 | — | — | — | 2 |
| Total | 2 | 7 | 23 | 1 | 1 | 34 |
Same complication with different consequences.
From these studies, 328 cases were reported, 6 conversions, average operating time of 61.3 minutes (SD±12.3), average hospital stay of 3.8 days (SD±1.2), 34 complications (25 of which were reported as minor, Table 2), and 17 bowel resections either laparoscopically or through a minilaparotomy incision guided laparoscopically. Table 2 shows the studies with their respective reported complications be it minor or major. The 6 conversions were due to encountering an obturator hernia, iatrogenic bowel injury to assess viability, and for an omentectomy as reported by Ferzli et al,5 along with bowel distention in 2 cases and a case of extensive intraabdominal adhesions as reported by Rebuffat et al.6
Laparoscopic manipulation and reduction was reported in 6 of the 7 manuscripts described above, while the seventh reports on the majority of cases being laparoscopically reduced (153/194), while the remaining were manually reduced after induction of anesthesia.7
Intraoperative injuries were reported to be one left colon injury by the Veress needle repaired with no consequence,7 one cecal injury repaired but with a mesh infection postoperatively that was salvaged by continuous irrigation,5 and one vas deferens injury with no comment on treatment.7 Two reoperations were reported by Ferzli et al5 and Leibl et al7 for insertion of sump drains for irrigation and salvage of infected mesh that were successful in both cases; the third reoperation was reported by Ishihara et al8 for exploration of a distended abdomen that turned out negative.
DISCUSSION
The laparoscopic approach for the elective repair of inguinal hernias has been well documented in the literature and widely accepted throughout surgical practice9–15; however, the use of this approach for the management of incarcerated/strangulated hernias has been a controversial issue with some surgeons being cautious in using this technique. This may be attributed to the technical difficulties encountered in reducing the hernia sac and contents and the increased risk for iatrogenic injuries.
The literature comparing the laparoscopic approach with open surgery suggests a clear superiority of the former,16–18 and there is also evidence comparing the 2 laparoscopic procedures together19–22; however, these studies report on reducible hernias only. The laparoscopic approach to chronic incarcerated or strangulated inguinal hernias remains scarce. The first successful treatment of an incarcerated hernia with a laparoscopic-guided intestinal resection was reported in 1993 by Watson et al.4 In 1996, Ishihara et al8 reported on a series using the TAPP approach for the reduction of incarcerated hernias and then to assess for bowel viability with an average operative time of 88 minutes with one complication that necessitated a laparotomy. This was followed by Leibl et al7 in 2001 reporting on a series of 194 patients all undergoing TAPP, some chronically incarcerated some acutely; average operative time was 55 minutes, with 7 complications and one recurrence. Other series reporting the TAPP approach include Rebuffat et al6 in 2006 reporting on a series of 28 with 72 minutes of average operating time, 3 conversions, a mean of 3.9 days of hospital stay, one complication (inguinal hematoma), and 9 bowel resections, all carried out laparoscopically. This was followed by Legnani et al23 in 2007 with a series of 9 TAPP repairs with an average operative time of 72 minutes and a hospital stay of 2.7 days and one bowel resection.
The TEP approach has more of a share of the published literature in cases with incarcerated or strangulated inguinal hernias. An exclusive TEP series was published by Ferzli et al5 in 2004 reporting on 11 patients with acute hernias, with results including 3 conversions, a mean operative time of 50 minutes, a mean hospital stay of 5.4 days, 2 complications, and 1 bowel resection for a strangulated hernia. However, they did highlight techniques that would ease the reduction of the sac in a TEP approach and would minimize the risk of injury to the bowel and/or the inferior epigastric vessels. In case of a direct hernia, a releasing incision is made in the anteromedial aspect of the defect to avoid the vessels. In indirect hernias, the vessels are controlled, clipped, and transected to facilitate the way for the releasing incision performed anteriorly in the deep (internal) ring at the 12 o'clock position toward the superficial (external) ring facilitating reduction of the incarcerated sac and its contents.5 Furthermore, in 2005 Mainik et al24 reported a series of 79 patients out of which 46 were treated with TEP with an average stay of 4.7 days. Saggar et al25 followed in the same year reporting on a series of 34 TEP repairs of incarcerated hernias all of which were chronic cases. Thier results show a mean operative time of 84.4 minutes, 2 recurrences, and no resections. Furthermore, hospital stay was less than 2 days in 90% of the cases (n=30) with a minor complication rate of 76.3%, all complications being treated conservatively.25
Bowel resection can be undertaken totally laparoscopically as per Rebuffat et al6 and Legnani et al,23 or it can be laparoscopically guided by a minilaparotomy on top of the area where the nonviable bowel has been laparoscopically located. Bowel or omentum needing resection can be found in both incarcerated and strangulated, moreso in the latter as Leibl et al show. They reported on 2 cases in the incarcerated group needing resection of necrotic omentum; on the other hand in the strangulated group, 2 patients needed omentectomy, one needing small bowel resection, and one needing an appendiceal resection.7 The length of stay as expected does become longer in the series that stratify the length of stay as per resections due to the time needed by patients to resume normal bowel function and tolerate a diet prior to discharge. Rebuffat et al6 show in their series that the length of stay increases from a mean of 2.6 days in the group with no resection to 6 days in the group with resections.
The issue of manual reduction of the bowel while the patient is under anesthesia is still controversial; however, using the laparoscopic approach solves this controversy for the bowel is examined in the peritoneal cavity without the need to manipulate outside through the internal ring as happens with the open technique. Instead, we can run the bowel inside the abdomen and assess its viability.26
A large series of 194 patients was reported by Leibl et al7 repairing incarcerated inguinal hernias using a TAPP approach. The reduction in this series was carried out partly manually in 47 cases, and laparoscopically in 153 cases or a combination of both in the remaining cases; however, the 6 bowel resections done were not alluded to as laparoscopically or otherwise. The morbidity in that series was 3.8% similar to rates in reducible hernias.7 Ferzli et al5 supported these findings in their series reporting no recurrences and 2 complications treated conservatively in their 11 case series of TEP repairs of strangulated hernias. Previously published data comparing laparoscopic with open hernia repair does confirm that the laparoscopic approach is superior to the open approach in minimizing persisting pain and numbness with a quicker return to usual activities. However, operation times are longer, the risk of serious complication rate with respect to visceral (especially bladder) and vascular injuries is higher,16 not to mention the higher cost which is in the order of an increment of 75%27 mostly contributed to the high cost of the disposable laparoscopic instruments.28 The complications that are of a higher risk with the laparoscopic approach are blind Veress needle insertion into a viscus or a vessel. That can be reduced by using an open Hasson port insertion and pneumoperitoneum insufflation, keeping in mind the relative contraindications for laparoscopy like previous surgery, extensive adhesions, and bowel distention due to obstruction that increases the likelihood of bowel injuries and iatrogenic serosal tears.
CONCLUSION
From this systematic review, we can conclude that the laparoscopic approach, irrespective of whether TEP or TAPP is used is feasible in tackling the problem, exposing the sac and its contents, reducing it, and eventually repairing the hernia with a mesh. It can also be used for bowel resection if the segment is deemed nonviable after the repair has been completed and gives ample time to the bowel to manifest as viable or nonviable to the surgeon. The overall rate of complication, recurrence, and hospital stay are very close to the rates documented in open repair for strangulated/incarcerated hernias; henceforth, this approach is a feasible and safe one in managing acute inguinal hernia presentations taking into consideration the knowledge of anatomy and expertise needed in dissecting and reducing the sac. Further randomized controlled trials are needed to confirm the superiority of the laparoscopic approach over the open approach in managing these presentations.
References:
- 1.Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol. 1996;25:835–839 [DOI] [PubMed] [Google Scholar]
- 2.Nilsson H, Stylianidis G, Haapamaki M, et al. Mortality after groin hernia surgery. Ann Surg. 2007;245:656–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallegos NC, Dawson J, Jarvis M, et al. Risk of strangulation in groin hernias. Br J Surg. 1991;78:1171–1173 [DOI] [PubMed] [Google Scholar]
- 4.Watson SD, Saye W, Hollier PA. Combined laparoscopic incarcerated herniorrhaphy and small bowel resection. Surg Laparosc Endosc. 1993;3:106–108 [PubMed] [Google Scholar]
- 5.Ferzli G, Shapiro K, Chaudry G, et al. Laparoscopic extra-peritoneal approach to acutely incarcerated inguinal hernia. Surg Endosc. 2004;18:228–231 [DOI] [PubMed] [Google Scholar]
- 6.Rebuffat C, Galli A, Scalambra MS, et al. Laparoscopic repair of strangulated hernias. Surg Endosc. 2006;20:13113–13114 [DOI] [PubMed] [Google Scholar]
- 7.Leibl BJ, Schmedt CG, Kraft K, et al. Laparoscopic transperitoneal hernia repair of incarcerated hernias: Is it feasible? Results of a prospective study. Surg Endosc. 2001;15:1179–1183 [DOI] [PubMed] [Google Scholar]
- 8.Ishihara T, Kubota K, Eda N, et al. Laparoscopic approach to incarcerated inguinal hernia. Surg Endosc. 1996;10:1111–1113 [DOI] [PubMed] [Google Scholar]
- 9.Ramshaw BJ, Tucker JG, Conner T, et al. A comparison of the approaches to laparoscopic herniorrhaphy. Surg Endosc. 1996;10:29–32 [DOI] [PubMed] [Google Scholar]
- 10.Stoker DL, Spiegelhalter DJ, Singh R, et al. Laparoscopic versus open inguinal hernia repair: randomised prospective trial. Lancet. 1994;343:1243–1245 [DOI] [PubMed] [Google Scholar]
- 11.Tschudi J, Wagner M, Klaiber C, et al. Controlled multicenter trial of laparoscopic transabdominal preperitoneal hernioplasty vs Shouldice herniorrhaphy. Early results. Surg Endosc. 1996;10:845–847 [DOI] [PubMed] [Google Scholar]
- 12.Vogt DM, Curet MJ, Pitcher DE, et al. Preliminary results of a prospective randomized trial of laparoscopic onlay versus conventional inguinal herniorrhaphy. Am J Surg. 169:84–89, 1995; discussion 9 –90 [DOI] [PubMed] [Google Scholar]
- 13.Hallen M, Bergenfelz A, Westerdahl J. Laparoscopic extra-peritoneal inguinal hernia repair versus open mesh repair: long-term follow-up of a randomized controlled trial. Surgery. 2008;143:313–317 [DOI] [PubMed] [Google Scholar]
- 14.Pokorny H, Klingler A, Schmid T, et al. Recurrence and complications after laparoscopic versus open inguinal hernia repair: results of a prospective randomized multicenter trial. Hernia. DOI 10.1007/s10029–008-0357–1 [DOI] [PubMed] [Google Scholar]
- 15.Takata MC, Duh QY. Laparoscopic inguinal hernia repair. Surg Clin North Am. 2008;88:157–178 [DOI] [PubMed] [Google Scholar]
- 16.McCormack K, Scott NW, Go PM, et al. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003:CD001785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kapischke M, Schulz T, Schipper T, et al. Open versus laparoscopic incisional hernia repair: something different from a meta-analysis. Surg Endosc. 2008;22(10):2251–2260 Epug 2008 Mar 5 [DOI] [PubMed] [Google Scholar]
- 18.Lal P, Kajla RK, Chander J, et al. Randomized controlled study of laparoscopic total extraperitoneal versus open Lichtenstein inguinal hernia repair. Surg Endosc. 2003;17:850–856 [DOI] [PubMed] [Google Scholar]
- 19.Wake BL, McCormack K, Fraser C, et al. Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2005:CD004703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen RV, Alvarez G, Roll S, et al. Transabdominal or totally extraperitoneal laparoscopic hernia repair? Surg Laparosc Endosc. 1998;8:264–268 [PubMed] [Google Scholar]
- 21.Kald A, Anderberg B, Smedh K, et al. Transperitoneal or totally extraperitoneal approach in laparoscopic hernia repair: results of 491 consecutive herniorrhaphies. Surg Laparosc Endosc. 1997;7:86–89 [PubMed] [Google Scholar]
- 22.Felix EL, Michas CA, Gonzalez MH., Jr Laparoscopic hernioplasty. TAPP vs TEP. Surg Endosc. 1995;9:984–989 [DOI] [PubMed] [Google Scholar]
- 23.Legnani GL, Rasini M, Pastori S, et al. Laparoscopic transperitoneal hernioplasty (TAPP) for the acute management of strangulated inguino-crural hernias: a report of nine cases. Hernia. 2008;12(2):185–188 Epub 2007 Nov 15 [DOI] [PubMed] [Google Scholar]
- 24.Mainik F, Flade-Kuthe R, Kuthe A. [Total extraperitoneal endoscopic hernioplasty (TEP) in the treatment of incarcerated and irreponible inguinal and femoral hernias]. Zentralbl Chir. 130:550–553, 2005. German [DOI] [PubMed] [Google Scholar]
- 25.Saggar VR, Sarangi R. Endoscopic totally extraperitoneal repair of incarcerated inguinal hernia. Hernia. 2005;9:120–124 [DOI] [PubMed] [Google Scholar]
- 26.Lavonius MI, Ovaska J. Laparoscopy in the evaluation of the incarcerated mass in groin hernia. Surg Endosc. 2000;14:488–489 [DOI] [PubMed] [Google Scholar]
- 27.Anadol ZA, Ersoy E, Taneri F, et al. Outcome and cost comparison of laparoscopic transabdominal preperitoneal hernia repair versus Open Lichtenstein technique. J Laparoendosc Adv Surg Tech A. 2004;14:159–163 [DOI] [PubMed] [Google Scholar]
- 28.Jacobs VR, Morrison JE., Jr Comparison of institutional costs for laparoscopic preperitoneal inguinal hernia versus open repair and its reimbursement in an ambulatory surgery center. Surg Laparosc Endosc Percutan Tech. 2008;18:70–74 [DOI] [PubMed] [Google Scholar]