Abstract
Background and Objectives:
The first laparoscopic appendectomy was performed over 25 years ago, and yet controversy still exists over the open method vs. the laparoscopic approach, and whether an incidental appendectomy is warranted. This study aimed to evaluate our experience in performing a laparoscopic incidental appendectomy and to address these issues.
Methods:
A total of 772 laparoscopic appendectomies were performed and analyzed and statistically evaluated.
Results:
Mean age of the patients was 30.8±7.0 years. Mean operating time for an incidental appendectomy was 12.3±4.5 minutes. Most common pathology result was adhesions, and the rarest was endometriosis. Of patients with confirmed appendicitis, 75.8% did not have an initial preoperative diagnosis of appendicitis. When warranted, 103 (13.3%) patients underwent a second-look laparoscopy: 75.5% had no adhesions, 23.5% had mild adhesions, 2% had moderate adhesions. Backward elimination logistic regression revealed that endometriosis (P=0.016), endometrioma (P=0.039), pelvic or abdominal adhesions (P=0.015) were associated with a reduced likelihood of encountering appendicitis on pathology examination. The complication rate was 0.13%. Anesthesia cost was lower for an incidental appendectomy compared with an urgent one.
Conclusion:
Laparoscopic incidental appendectomy is safe and quick to perform. Due to the complex nature of confirming the diagnosis of pelvic and abdominal pain, this study supports the routine performance of an incidental appendectomy in the female patient.
Keywords: Laparoscopy, Incidental appendectomy, Surgical technique
INTRODUCTION
Since its introduction in 1983,1 laparoscopic appendectomy has not completely replaced the conventional method of open appendectomy. Previous randomized studies of laparoscopic appendectomy had conflicting results2–4 due in part to limited sample sizes, contributing to the controversy of this relatively new surgical technique. It seems reassuring however that in recent years, with some implementation of advanced endoscopic training in surgical programs in the United States and abroad, there is a progressing trend acknowledging the superiority of the mentioned approach compared with the traditional open technique.5–8
Incidental appendectomy, once commonly performed in gynecological surgery, has been discouraged during recent years; however, laparoscopic surgery has undergone dramatic improvements in technology and surgical technique during the last 10 years, raising the possibility that incidental appendectomy can be performed in a safe, efficient, and cost-effective manner. This study investigates the safety and feasibility of incidental appendectomy in women by evaluating 772 laparoscopic appendectomies performed during routine laparoscopic gynecological surgery.
MATERIALS AND METHODS
The study sample consisted of 772 women who underwent laparoscopic incidental appendectomy during operative laparoscopy for evaluation and treatment of infertility, endometriosis, as well as for other diverse pelvic pathologies. All surgeries were performed at an outpatient surgical center in Oak Brook, Illinois during the 7-year period from January 1995 through December 2002. Although 1372 appendectomies were performed from 1995 to 2008, statistical analysis was performed on cases up to the year 2002 due in part to the large sample size and the time it took to process the data. More information will be available in future studies.
General endotracheal anesthesia was administered to all patients undergoing surgery, and every patient received 2 g of Cephalexin IV as prophylactic antibiotics 30 minutes before the scheduled procedure. Patients with penicillin allergy were given 900 mg of Clindamycin. All patients underwent routine induction of pneumoperitoneum. The standard technique of open laparoscopy9 was applied. Under direct visualization, three 5-mm ancillary trocars were placed in the abdomen. Two were placed in the right and left lower quadrants (RLQ and LLQ), and the third was placed approximately 2 to 3 fingerbreadths above the pubic symphysis. The placement of all 3 ancillary trocars however varied, depending on the size and location of the pathology encountered. Grasping forceps, scissors, endoloops, suction and irrigation, and electrocautery were introduced into the abdomen through the ancillary trocars. Resection of pelvic pathology was performed using laparoscopic scissors and unipolar cautery, and hemostasis was accomplished utilizing bipolar and unipolar cautery.
The procedures ranged from relatively simple surgeries, such as endometriosis ablation, tubal ligations, ovarian cystectomy, salpingo-ovariolysis, salpingectomy, salpingo-oophorectomy and salpingostomy, to more technically challenging surgeries, such as laparoscopic enterolysis, myomectomy, hysterectomy, fimbrioplasty, and tubal reanastomosis.
Once the primary problems were managed, attention was turned to the appendix. Periappendicular and pericecal adhesions were taken down sharply when adhesions were present, to mobilize the cecum and appendix. This was done primarily using atraumatic forceps introduced through the left and right lower quadrant trocars to put the organs under traction, and the scissors introduced through the suprapubic port to cut the adhesions.
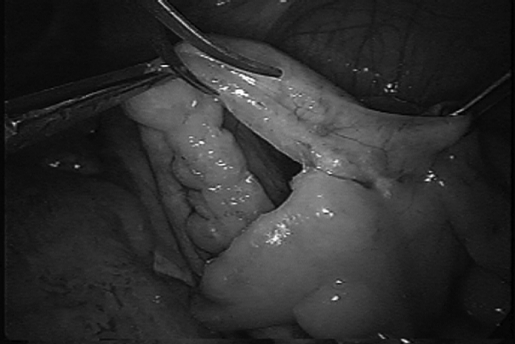
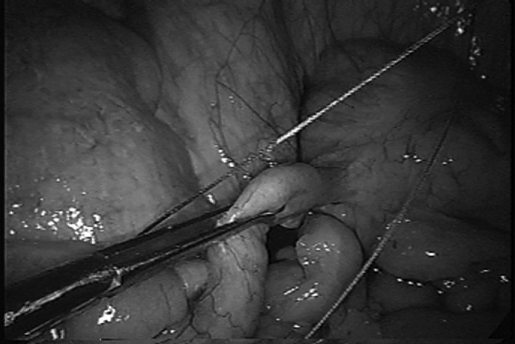
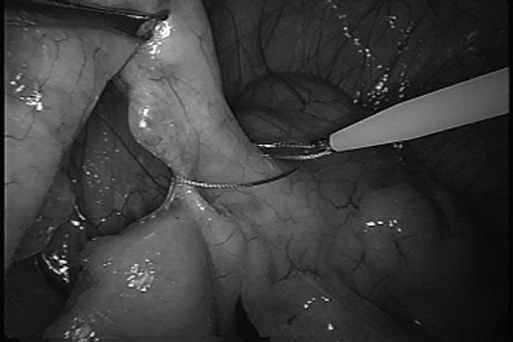
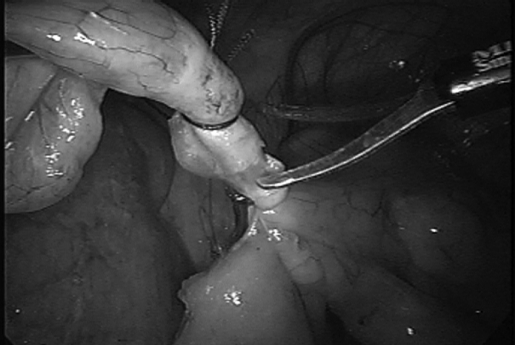
After the cecum and appendix were mobilized, the mesoappendix was cauterized and cut, and the appendicular artery was isolated, cauterized, and transected (Figure 1). Three Endoloop (CooperSurgical) ligatures were introduced through the right lower quadrant (RLQ) trocar and applied to the junction where the appendix extends into the cecum (Figures 2, 3). This was done by maneuvering the forceps through the loop and grasping the appendix, lifting it up and placing it under tension so as to allow the tip of the endoloop to meet at the area of interest on the appendix in a perpendicular fashion. Two ligatures were placed at the base of the appendix in this manner approximately 2 mm apart. Holding the appendix under careful tension, the bipolar cautery was then introduced through the RLQ trocar perpendicular to the appendix. The appendix was initially crushed with the bipolar cautery in an upward fashion to facilitate the movement of any fecal matter if present, and then the same areas were subsequently cauterized (Figure 4). At this point, the third and final ligature was placed approximately 7 mm above the last ligature placement in a gentle fashion, so as to prevent premature amputation of the organ. The area between the second and third ligature application was cut-cauterizedcut respectively, all through the RLQ trocar.
Figure 1.
Cauterization of appendicular artery and mesoappendix takedown.
Figure 2.
Manipulation and positioning of the appendix for the Endo Loop.
Figure 3.
Endo Loop application.
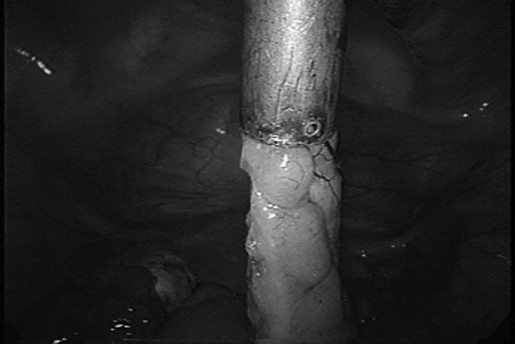
Figure 4.
Cauterization and transection of the appendix.
The amputated appendix was held with atraumatic graspers from the right, as a 10-mm trocar was introduced through the suprapubic port after the 5-mm ancillary trocar was removed and the incision site was extended (Figure 5). Care was taken to prevent the appendix from coming into contact with any surrounding tissues. Through the now 10-mm suprapubic port, a grasper with teeth was introduced, and the appendix was secured and removed through the same port to avoid contamination to the anterior abdominal wall. All other resected specimens were also removed through this trocar. The entire suprapubic incision was then cauterized from the inside out to destroy any tracks left behind. The fascial incision was reapproximated with 0-absorbable polyglactin suture at the end of the procedure. All operative sites were evaluated for hemostasis, and a final peritoneal lavage was performed with the suction/irrigator. All instruments were removed from the abdomen, and the gas was allowed to escape.
Figure 5.
Removal of the appendix through a protective cannula.
All patients went home the same day, and most underwent uneventful postoperative recoveries. Patients were seen in the office one week later to assess their postoperative recovery.
For the 772 women in the study, data were collected on age, gravidity, parity, race, primary diagnosis, procedure, operative time, pathology, gynecologic findings, results of second-look laparoscopies when applicable, and complications. Four types of complications were of primary interest: infection (wound infection and peritonitis), hospital admission (nausea and vomiting, ileus, obstruction, pain management), visceral injury, and bleeding (intraand postoperative). There were no conversions to a laparotomy, and only one complication was observed. One patient developed a wound cellulitis that resolved with oral antibiotics.
SPSS for Windows (Version 11) was used for data management and statistical analysis. Comparison of independent groups with respect to percentages was done with Fisher's exact test. The pooled-variance or separate-variance t test was used to compare 2 independent groups with respect to normally distributed variables. Levene's test was used to determine whether the pooled-variance or separate-variance t test should be done. To compare 2 independent groups with respect to nonnormally distributed, noncategorical variables, the nonparametric Mann-Whitney test was used. All means are presented as mean ± standard deviation (SD). A 0.05 significance level was used for all statistical tests. No one-sided statistical tests were done.
RESULTS
Table 1 summarizes the demographic and clinical characteristics of the study sample, including the percentage of patients with an initial diagnosis of appendicitis and diagnoses present for at least 5% of the women. Nearly all of the women in the study were Hispanic. The mean age was 30.8±7.0 years (range, 14 to 56).
Table 1.
Demographic and Clinical Characteristics of Study Sample
| Characteristics | Mean ± SD or % |
|---|---|
| Age | 30.8 ± 7.0 |
| Gravidity | 1.7 ± 1.9 |
| Parity | 1.2 ± 1.5 |
| Race | |
| Hispanic | 98.3 |
| Caucasian | 1.2 |
| African-American | 0.4 |
| Asian | 0.1 |
| Initial diagnosis | |
| Appendicitis | 3 |
| Endometriosis | 81.1 |
| Appendicular endometriosis | 5.2 |
| Endometrioma | 7.6 |
| Pelvic or abdominal adhesions | 11.1 |
| Periappendicular or appendicular adhesions | 86.8 |
| Ovarian, CL, or simple cyst | 35.4 |
| Paratubal cyst | 21.8 |
| Myoma, fibroma, or fibroids | 16.8 |
| Hydrosalpinx | 9.2 |
| Menometrorrhagia | 8.7 |
| Tubal occlusion or obstruction | 6.5 |
Only 3% of the women had an initial diagnosis of appendicitis. Women with an initial diagnosis of appendicitis were more likely than women without this diagnosis to have appendicitis on pathology examination (34.8% versus 3.3%; P<0.0005). However, 75.8% of the women with confirmed appendicitis did not have an initial diagnosis of appendicitis.
Every case was videotaped from the beginning to the end; this allowed the ability to time any specific portion of the operation very accurately. The mean operating time for the incidental appendectomy was 12.3±4.5 minutes (range, 4.0 to 39.8). The operating time was less than 15 minutes for 78.1% of the cases and less than 20 minutes for 94.3% of the cases. The length of the procedure reflected anatomical considerations (eg, retrocecal ascending appendix) and the severity of the pelvic pathology (eg, stage IV endometriosis, previous surgeries with adhesions, and chronic pelvic inflammatory disease), as well as the participation of residents and fellows. Complications were extremely rare, with one case of postoperative cellulitis involving a skin incision that resolved with a 10-day course of oral antibiotics. Pathology results found in at least 1% of the women are shown in Table 2.
Table 2.
Appendix Pathology Results
| Result | % |
|---|---|
| Appendicitis | 4.3 |
| Chronic | 0.5 |
| Acute | 3.2 |
| Vermiform | 0.1 |
| Catarrhal | 0.1 |
| Acute and chronic | 0.1 |
| Granulomatous | 0.1 |
| Periappendicitis | 0.1 |
| Obliteration or obliterative changes | 7.4 |
| Inflammation | 4.5 |
| Endometriosis | 2.2 |
| Adhesions | 29.1 |
| Fibrosis | 24.2 |
| Fecalith | 3.4 |
| Hyperplasia | 11.8 |
| Vermiform | 22.7 |
| Involutional changes | 9.7 |
| Congestion | 10.2 |
Only 22.7% of the appendixes in 772 cases were normal; the rest had varying degrees of pathology. The most common pathology result was adhesions, followed by fibrosis. Excluding vermiform appendix, hyperplasia, congestion, involutional changes, and obliteration of the appendix followed in terms of descending frequency before the diagnosis of appendicitis was encountered.
There was no statistically significant difference between women with appendicitis and women without in respect to age (P=0.06) or parity (P=0.12); however, women with appendicitis had higher gravidity than women without (2.5±2.8 versus 1.6±1.8) (P=0.046).
A second-look surgery was performed in 103 (13.3%) of the women. The mean time from the initial surgery to the second-look surgery was 1.5±1.4 years (range, 0.1 to 6.0). At the second-look surgery, 75.5% of the women had no pericecal, cecal, or periappendicular stump adhesions. Mild adhesions of these types, defined as the presence of one of the mentioned adhesions, were found in 23.5% of the women with a second-look surgery. Moderate adhesions, defined as the presence of no more than 2 of the mentioned adhesions, were found in 2%.
In most cases, the preoperative and postoperative diagnoses were virtually the same. Backward elimination logistic regression (using likelihood ratio P-values) was performed with the following potential independent variables to investigate whether any preoperative variables could be used to predict appendicular pathology: age, gravidity, and each of the following preoperative diagnosis indicator variables: endometriosis; endometrioma; pelvic or abdominal adhesions; paratubal cysts; pelvic pain; menometrorrhagia; appendicular endometriosis; pelvic or abdominal adhesions; ovarian, corpus luteum (CL), or simple cyst; salpingitis isthmica nodosa; myoma, fibroma, or fibroids; adenomyosis or adenomyoma; PCOD; hydrosalpinx; cervical dysplasia; and lipoma. The following variables were kept in the final model and were all specifically associated with a reduced chance of finding appendicitis on pathology: endometriosis (P=0.016); endometrioma (P=0.039); pelvic or abdominal adhesions (P=0.015). The sensitivity and specificity of these 3 variables for predicting the pathology of appendicitis were low: 52% and 72%, respectively. The positive and negative predictive values were 8% and 97%, respectively.
A few interesting associations in regards to the preoperative diagnosis and appendicular pathology that were statistically significant were also found. They are as follows: a preoperative diagnosis of paratubal cysts was associated with an increased chance of appendix pathology showing inflammation (7.7% versus 3.6%; P=0.024). A preoperative diagnosis of appendicular endometriosis was associated with an increased chance of a sclerosed appendix (5.0% versus 0.4%; P=0.024). A preoperative diagnosis of pelvic or abdominal adhesions was associated with an increased chance of appendix with a fecalith (8.1% versus 2.8%; P=0.019). A preoperative diagnosis of adenomyosis or adenomyoma was associated with an increased chance of the following appendix pathology findings: fibrosis (38.9% versus 23.5%; P=0.035); obliteration or obliterative changes (16.7% versus 6.9%; P=0.042). A preoperative diagnosis of hydrosalpinx was associated with an increased chance of the following appendix pathology findings: vermiform appendix (32.4% versus 21.7%; P=0.040); obliteration or obliterative changes (14.1% versus 6.7%; P=0.023).
A preoperative diagnosis of cervical dysplasia was associated with an increased chance of the appendix showing fibrosis (40.5% versus 23.4%; P=0.018). The cost of additional anesthesia time was also factored into our study. A cost comparison analyzing additional operative time to perform the incidental appendectomy during a routine case was assessed against a laparoscopic appendectomy performed under an acute/emergent setting, as summarized in Table 3. The base number of units is determined by a variety of factors, such as airway class; elective, acute or emergent settings; and the medical condition of the patient. Thus, more seriously ill patients undergoing surgery in emergent conditions will be charged with a higher base number of units plus additional units depending on the length of the surgery. The costs reflect the 2008 fiscal year based on a large private practice anesthesia group in our community (Associated Anesthesiologists of Joliet, Joliet, Illinois).
Table 3.
Anesthesia Cost for Appendectomy: Incidental vs Acute
| Incidental | Acute |
|---|---|
| 4 base units | 6-8 base units |
| Average cost starting at $200-250* | Average cost starting at $300-400* |
$50 per unit. One unit = 15 min.
DISCUSSION
The incidence of appendicitis in the general population is approximately 11 per 10 000 population per year.10 According to the life table model produced by Addiss et al,10 the lifetime risk for appendicitis in women is 6.7%. The lifetime risk of undergoing an appendectomy in general for women in the United States is 23.1%. Over 250 000 appendectomies are performed annually in the United States.10 Much debate has occurred regarding whether laparoscopic appendectomy should replace traditional open appendectomy,11–21 and whether an incidental appendectomy is truly cost effective and appropriate.22–26
In our experience, performing an incidental appendectomy during routine gynecologic laparoscopic surgery is safe and quick. In 772 cases, the complication rate was 0.13%. We had one patient who experienced a postoperative cellulitis involving the skin incision, but only a 10-day course of oral antibiotics was required.
The mean operative time for performing the appendectomy was 12.3 minutes (±4.5 minutes), with a range spanning anywhere between 4 minutes and 39.8 minutes. The times varied depending on whether a fellow or resident was present, as well as the type of pathology and anatomical factors encountered. The operating time was <15 minutes 78.1% of the time.
The most common appendicular pathology was adhesions, followed by fibrosis. The rarest result seen was endometriosis. As Table 2 demonstrates, hyperplasia, congestion, involutional changes, and obliteration of the appendix were encountered in terms of descending frequency before appendicitis was seen. This may perhaps represent the progression of the disease process. Because we have routinely performed incidental appendectomies on all patients in the study, our pathology represents a cross-sectional view of the general female population being evaluated for a gynecological problem.
A few interesting associations found in our results that were statistically significant should be elaborated on. The diagnosis of paratubal cysts was associated with an increased chance of having an appendix with inflammation on pathology. This may be explained by the formation of peritoneal or inflammatory cysts in general when an infection process is present. The paratubal cyst formation may be a by-product of a general inflammatory/infectious process. Also, the presence of endometriosis was associated with a sclerosed appendix. The effects on the appendix may be the scarring and defects commonly seen throughout the pelvic peritoneum in moderate to severe cases of endometriosis. Abdominal/pelvic adhesions associated with a higher incidence of fecalith may be relatively self-explanatory, reinforcing the notion that a blocked and compromised appendicular lumen can lead to congestion, inflammation, and adhesions, and finally to a possible early appendicitis.
Backward elimination logistic regression study however revealed the contrary: the diagnosis of endometriosis, endometrioma, pelvic or abdominal adhesions was associated with a decreased likelihood of finding appendicitis on pathology examination. We are not certain why this was observed. In our practices, we treat a large number of infertility and chronic pelvic pain patients with the abovementioned diagnosis. We have speculated that the incidence of appendicitis in our study was low due in part to the large sample size of patients. Few and rare case reports in the literature cite the incidental diagnosis of endometriosis of the appendix when an appendectomy was performed for presumed appendicitis.27,28 Perhaps the reason this finding is so rare to begin with is the possible existence of a protective factor for appendicitis in patients with endometriosis. Further study will be required to see if this is true, but a comprehensive literature review by Gustofson et al29 also found that appendiceal endometriosis was not common in patients with endometriosis.
Of 772 cases, 103 involved a second-look laparoscopy to assess tubal healing and other factors pertinent to reproductive function, or due to recurring pathology. This opportunity allowed us to evaluate the outcomes of our surgical technique, and in the majority of the cases (75.5%) no adhesions were seen at the appendectomy site. The technique described in this study seems favorable when it comes to decreasing postoperative adhesion formation; however, a prospective trial evaluating adhesion formation comparing stapling devices to dissolvable sutures would be invaluable.
CONCLUSION
For our general surgery colleagues, because both male and female patients are evaluated and treated, the idea of performing an incidental appendectomy in general may not appear to be so compelling. For female patients, however, the presentation of pelvic and/or abdominal pain may not be as straightforward as in their male counterparts, and delays in confirming the diagnosis may lead to serious consequences. Guss and Richards30 reported in their study that the mean time from emergency room presentation to operative intervention was 477 minutes for men and 709 minutes for women for confirmed appendicitis; however, this delay was not associated with an increased rate of perforation. Contrary to our expectations, Flum et al31 showed in their study that the diagnosis of appendicitis has not improved with the availability of today's advanced imaging technology. By and large, establishing an accurate diagnosis in the female patient with pelvic and abdominal pain still remains a challenge.
Flum and Koepsell32 found in their study that female patients had a greater negative appendectomy rate (22.2%) than male patients (9.3%) had, which again supports the notion that confirming the diagnosis is easier in men than in women. Itskowitz and Jones33 have also shown similar negative appendectomy rates in women (20%), with Incesu and Taylor34 reporting the highest false-positive appendectomy rates in women at 47%. Due to the complexity of confirming diagnoses in women, these findings suggest that an incidental appendectomy holds a higher value in females than in males.
A recent study by Sporn et al,35 who analyzed 235 473 appendectomies, concluded that in general, an open appendectomy may be preferable to the laparoscopic approach in patients with acute appendicitis, due to the higher costs and increased morbidity in the latter group. If incidental appendectomy were to be performed in all patients undergoing scheduled surgeries, perhaps this issue of cost and potential complications would not be a factor any longer. The cost of the workup for a possible appendicitis in the female patient can be reduced or avoided, or both, and the potential source for pelvic and abdominal pain can become clearer if appendicitis need not be considered.
Although the incidence of appendicitis was low in our study (4.3%) for reasons stated earlier, 75.8% of the women with appendicitis did not have an initial diagnosis of appendicitis preoperatively. The diagnosis was only confirmed after the fact. In the authors' hands, the complication rate for performing incidental appendectomy was very low. The authors believe that individual results and complication rates will vary; however, when factoring in the short amount of time required to perform an incidental appendectomy and the extremely low complication rate, as well as the low cost of anesthesia time compared with time performing one under acute settings, the authors suggest considering performing an incidental appendectomy when given the opportunity in the female patient.
Acknowledgments
The authors would like to express their sincere gratitude to Susan Shott, PhD, for her help in the statistical analysis of this study.
Contributor Information
Jonathan Y. Song, TLC Medical Group, SC, Oak Brook Institute of Endoscopy, Rush Medical College, St. Charles, Illinois, USA..
Edgardo Yordan, Oak Brook Institute of Endoscopy, Rush Medical College, Downers Grove, Illinois USA..
Carlos Rotman, Oak Brook Institute of Endoscopy, Rush Medical College, Downers Grove, Illinois USA..
References:
- 1.Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64 [DOI] [PubMed] [Google Scholar]
- 2.Laine S, Rantala A, Gullichsen R, Ovaska J. Laparoscopic appendectomy-is it worthwhile? A prospective, randomized study in young women Surg Endosc. 1997;11:95–97 [DOI] [PubMed] [Google Scholar]
- 3.Macarulla E, Vallet J, Abad JM, Hussein H, Fernandez E, Nieto B. Laparoscopic versus open appendectomy: a prospective randomized trial. Surg Laparosc Endosc Percutan Tech. 1997;7(4):335–339 [PubMed] [Google Scholar]
- 4.Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999;177(3):250–256 [DOI] [PubMed] [Google Scholar]
- 5.Kehagias I, Karamanakos S, Panagiotopoulos S, Panagopoulos K, Kalfarentzos F. Laparoscopic versus open appendectomy: which way to go? World J Gastroenterol. 2008;14(31):4909–4914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jaffer U, Cameron A. Laparoscopic appendectomy: a junior trainee's learning curve. JSLS. 2008;12(3):288–291 [PMC free article] [PubMed] [Google Scholar]
- 7.Rezola E, Villanueva A, Garay J, et al. Laparoscopic appendectomy after the learning curve. Cir Pediatr. 2008;21(3):167–172 [PubMed] [Google Scholar]
- 8.Delgado A, Sotomayor R. Comparison between open and laparoscopic appendectomy in non-complicated appendicitis. Bol Asoc Med P R. 2008;100(1):20–25 [PubMed] [Google Scholar]
- 9.Hasson HM, Rotman C, Rana N, Kumari NA. Open laparoscopy: 29-year experience. Obstet Gynecol. 2000;96(5):763–766 [DOI] [PubMed] [Google Scholar]
- 10.Addis DG, Schaffer N, Fowler B, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–925 [DOI] [PubMed] [Google Scholar]
- 11.Pier A, Gotz F, Bacher C. Laparoscopic appendectomy in 625 cases: from innovation to routine. Surg Laparosc Endosc. 1991;1:8–13 [PubMed] [Google Scholar]
- 12.Pier A, Gotz F, Bacher C, Ibald R. Laparoscopic appendectomy. World J Surg. 1993;17:29–33 [DOI] [PubMed] [Google Scholar]
- 13.Frazee RC, Roberts JW, Symmonds RE, et al. A prospective randomized trial comparing open vs. laparoscopic appendectomy. Ann Surg. 1994;219:725–731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen JB, Smithers BM, Schache D, Wall DR, Miller BJ, Menzies BL. Laparoscopic vs. open appendectomy: prospective randomized trial. World J Surg. 1996;20:17–21 [DOI] [PubMed] [Google Scholar]
- 15.Hellberg A, Rudberg C, Kullman E, et al. Prospective randomized multicenter study of laparoscopic vs. open appendectomy. Br J Surg. 1999;86:48–53 [DOI] [PubMed] [Google Scholar]
- 16.Vallina VL, Velasco JM, McCulloch CS. Laparoscopic vs. conventional appendectomy. Ann Surg. 1993;218:685–692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moberg A, Montgomery A. Appendicitis: laparoscopic vs. conventional operation. A study and review of the literature Surg Laparosc Endosc. 1997;7:459–463 [PubMed] [Google Scholar]
- 18.McAnena OJ, Austin O, O'Connell PR, Hedennan WP, Gorey TF, Fitzpatrick J. Laparoscopic vs. open appendectomy: a prospective evaluation. Br J Surg. 1992;79:818–820 [DOI] [PubMed] [Google Scholar]
- 19.Attwood SEA, Hill ADK, Murphy PG, Thornton J, Stephens RB. A prospective randomized trial of laparoscopic vs. open appendectomy. Surgery. 1992;112:497–501 [PubMed] [Google Scholar]
- 20.Heinzelmann M, Simmen HP, Cummins AS, Largiader F. Is laparoscopic appendectomy the new ‘gold standard’? Arch Surg. 1995;130:782–785 [DOI] [PubMed] [Google Scholar]
- 21.Tate JJT, Dawson JW, Chung SCS, Lau WY, Li AKC. Laparoscopic vs. open appendectomy: prospective randomized trial. Lancet. 1993;342:633–637 [DOI] [PubMed] [Google Scholar]
- 22.Wang HT, Sax HC. Incidental Appendectomy in the era of managed care and laparoscopy. J Am Coll Surg. 2000;192(2):182–188. [DOI] [PubMed] [Google Scholar]
- 23.Sugimoto T, Edwards D. Incidence and costs of incidental appendectomy as a preventive measure. Am J Public Health. 1987;77(4):471–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nezhat C, Nezhat F. Incidental appendectomy during video-laseroscopy. Am J Obstet Gynecol. 1991;165:559–564 [DOI] [PubMed] [Google Scholar]
- 25.Snyder TE, Selanders JR. Incidental appendectomy-yes or no? A retrospective case study and review of the literature Infec Dis Obstet Gynecol. 1998;6:30–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lynch CB, Sinha P, Jalloh S. Incidental appendectomy during gynecological surgery. Int J Gynecol Obstet. 1997;59:261–262 [DOI] [PubMed] [Google Scholar]
- 27.Uncu H, Taner D. Appendiceal endometriosis: two case reports. Arch Gynecol Obstet. 2008;278(3):273–275 [DOI] [PubMed] [Google Scholar]
- 28.Duinslaeger M, Goovaerts G, De Waele B, Willems G. Endometriosis of the appendix. Acta Chir Belg. 1985;85(4):219–221 [PubMed] [Google Scholar]
- 29.Gustofson R, Kim N, Liu S, Stratton P. Endometriosis and the appendix: a case series and comprehensive review of the literature. Fertil Steril. 2006;86(2):298–303 [DOI] [PubMed] [Google Scholar]
- 30.Guss D, Richards C. Comparison of men and women presenting to an ED with acute appendicitis. Am J Emerg Med. 2000;18(4):372–375 [DOI] [PubMed] [Google Scholar]
- 31.Flum DA, Morris A, Koepsell T, Dellinger EP. Has misdiagnosis of appendicitis decreased over time? JAMA. 2001;286(14):1748–1753 [DOI] [PubMed] [Google Scholar]
- 32.Flum DA, Koepsell T. The clinical and economic correlates of misdiagnosed appendicitis. Arch Surg. 2002;137:799–804 [DOI] [PubMed] [Google Scholar]
- 33.Itskowitz MS, Jones SM. Appendicitis. Emerg Med. 36(10):10–15, 2004 [Google Scholar]
- 34.Incesu L, Taylor C. Appendicitis. Available at: http://www.emedicine.medscape.com/article/363818-overview
- 35.Sporn E, Petroski GF, Mancini GJ, Astudillo JA, Miedema BW, Thaler K. Laparoscopic appendectomy-is it worth the cost? Trend analysis in the US from 2000 to 2005. J Am Coll Surg. 2009;208(2):179–185 [DOI] [PubMed] [Google Scholar]