Abstract
Objectives:
Single-port surgery is a rapidly advancing technique in laparoscopic surgery. Currently, there is limited evidence on the learning curve and practicality of performing single-port laparoscopic cholecystectomy.
Methods:
Single-port cholecystectomy was performed on 20 consecutive patients for biliary dyskinesia, symptomatic cholelithiasis, or acute cholecystitis. The Tri-Port was placed in the umbilicus, and a combination of straight and articulating instruments were utilized. Patient characteristics and outcomes were reviewed, and a comparison was made with the prior 20 consecutive laparoscopic cholecystectomies performed using the 3-port technique.
Results:
Characteristics were similar in both groups. The 3-port cholecystectomy had a mean time of 65.7 minutes, and patients had an average body mass index of 28.16. The first single-port cholecystectomy took 160 minutes with sequential improvement to the sixth case of 66 minutes with a mean of 68.2 minutes for the last 15 single-port cases. The average patient body mass index was 30.24. No major complications occurred.
Conclusion:
The largest series to date of single-port cholecystectomy for multiple degrees of biliary disease is presented. This study validates that this technique can be applied effectively and performed in comparable operative times to traditional 3-port cholecystectomy with a learning curve of approximately 5 cases.
Keywords: Single incision, Single-port access, Laparoscopic, Cholecystectomy
INTRODUCTION
Over the last 20 years, laparoscopic cholecystectomy has replaced open cholecystectomy as the standard of care for the majority of benign diseases of the gallbladder. Laparoscopic cholecystectomy became a standardized operation using 3 or 4 ports placed around the abdomen. However as early as 1999,1 reports showed that multiple trocars could be placed through a single skin incision to perform the same operation. This came to be called single-incision surgery. Recently, the development of multi-channel port design has allowed laparoscopic procedures to be performed using a single fascial incision, ushering in single-port surgery.
Several types of procedures have been performed via single-port surgery, mostly reported in the urologic literature.2,3 Although single-port laparoscopic cholecystectomy has previously been described in the literature, evaluation of the utility of this procedure is limited to patient-selected case series.4 For single-port surgery to be widely adopted, surgeons must demonstrate reproducibility of the technique across a broad spectrum of patients and clinical scenarios.
In this article, we relate the largest published series of single-port cholecystectomies for consecutive patients presenting with gallbladder disease amenable to laparoscopic surgery. We compared our results in these patients with results for our prior traditional 3-port laparoscopic cholecystectomies to assess feasibility of the technique from an operative and postoperative perspective.
METHODS
Until the beginning of May 2008, we performed 3-port laparoscopic cholecystectomies to treat gallbladder disease. As the Tri-Port (Advanced Surgical Concepts, Breslow, Ireland), an FDA-approved multi-channel port, became available to us for the performance of single-port surgery, we transitioned to performing all laparoscopic cholecystectomies utilizing the single port. We retrospectively reviewed the effects of this transition on operating times and surgical complications.
All patients had been evaluated for biliary disease either in the office or through the emergency room. Surgery was scheduled on an elective or urgent basis, depending on the severity of the presenting disease. A single surgeon (MAK) performed all procedures at 2 different hospitals over a 7-month time period between February and August 2008.
All patients who underwent cholecystectomy during this time period were reviewed. However, patients who underwent open cholecystectomy or did not undergo single-port or 3-port cholecystectomy were excluded from the analysis. Institutional review board approval was obtained for data to be collected retrospectively.
Traditional Cholecystectomy
The 3-port laparoscopic cholecystectomy was performed by first entering the abdomen with the 5-mm Optiview trocar (Ethicon Endosurgery, Cincinnati, OH) through the umbilicus and then exchanging this trocar for a 12-mm port. Two 5-mm trocars were placed, one at the subxyphoid position and another in the right subcostal area. The surgeon operated the 2 working instruments with the assistant holding the camera. In brief, standard dissection principles were followed; the cystic duct and artery were clipped, and the specimen was removed in a specimen bag through the umbilicus. Intraoperative cholangiography was performed if necessary by passing a cholangiocatheter through an 18-gauge needle inserted subcostally.
Single-Port Surgery
For the single-port procedures, the abdomen was accessed using the direct Hasson technique through a 15-mm peri-umbilical incision, and the Tri-Port was deployed into the abdomen. A prior description of the mechanical aspects of this type of port has been published.4
The procedures were performed using a combination of straight and articulating instruments. Articulating instruments, Real Hand (Novare Surgical, Cupertino, CA) are fully articulating instruments allowing 6 degrees of motion that correlate with the motion of the operator's wrist. Depending on the hospital in which the procedure was performed, either Stryker or Olympus 5-mm 30-degree laparoscopes were used for visualization.
Following access and placement of the Tri-Port, the operating surgeon and the assistant stood on the patient's left side with the assistant in front of the surgeon (Figure 1). The single-incision laparoscopic cholecystectomy was commenced by elevating the gallbladder with a 42-inch straight grasper held at the fundus and retracting cephalad. In 18 of 20 cases, a straight needle with an attached Prolene suture was passed via the right lateral abdominal wall through the infundibulum of the gallbladder to serve as an additional traction point. A surgical clip was placed at the puncture point to prevent any spillage of bile (Figure 2). The surgeon held the camera and the operating instruments, while the assistant held the fundal instrument and the Prolene suture. Dissection of the triangle of Calot was performed by using a combination of straight and articulating Maryland dissectors. In 3 cases, a second Prolene suture was passed around the falciform from the left subcostal area for retraction because of obstruction by the liver.
Figure 1.
Placement of the Tri-Port.
Figure 2.
Placement of surgical clip at the puncture point to prevent spillage of bile.
In all cases, meticulous dissection was performed with complete exposure of the cystic duct, the cystic artery, and the shoulder of the common bile duct. No energy sources were used during the dissection of these structures. Intraoperative cholangiography was performed if necessary by passing a cholangiocatheter through an 18-gauge needle inserted subcostally. The cystic duct and artery were clipped with an Ethicon Ligamax 5-mm clip applier. Electrocautery was then used to remove the gallbladder from the liver bed, and the specimen was removed in a specimen bag along with the port.
Statistical Methods
All statistical analyses of categorical variables were performed using Fisher's exact test and those of interval data with the Student t test (OpenEpi Version 2.2.1, updated 2008/04/05).
RESULTS
We retrospectively reviewed 43 consecutive patients who presented with gallbladder disease necessitating surgery. One patient in the series was planned preoperatively to have an open cholecystectomy because of multiple prior abdominal procedures and a large ventral hernia. This patient's data are not included in this review. The first 2 patients who underwent single-port surgery required the placement of an additional port to complete the procedure (discussed later). These were excluded from the analysis as they underwent a 2-port operation. Subsequently, 40 patients were evaluated in the analysis: 20 patients who underwent single-port and 20 patients who underwent 3-port cholecystectomy.
Neither baseline characteristics of the included patients (Table 1) nor the indications for surgery (Table 2) differed statistically between the 2 groups. Operative times were calculated from the first incision to complete closure of the final incision at the end of the case.
Table 1.
Baseline Characteristics
| Single-Port Laparoscopic Cholecystectomy | 3-Port Traditional Cholecystectomy | P Value | |
|---|---|---|---|
| Sex, n (%) | 0.35 | ||
| Male | 4 (20) | 6 (30) | |
| Female | 16 (80) | 14 (70) | |
| Age, yrs | 0.71 | ||
| Mean | 43.95 | 45.8 | |
| Median | 41 | 42 | |
| Body Mass Index | 0.43 | ||
| Mean | 30.24 | 28.16 | |
| Median | 30.5 | 24 | |
| ASA Score, n (%) | |||
| 1 | 2 (10) | 3 (15) | 0.5 |
| 2 | 16 (80) | 15 (75) | 0.5 |
| 3 | 2 (10) | 2 (10) | 0.69 |
| Coronary Artery Disease, n (%) | 1 (5) | 1 (5) | 0.75 |
| Diabetes Mellitus, n(%) | 2 (10) | 1 (5) | 0.5 |
Table 2.
Preoperative Indications for Surgery
| Single-Port Cholecystectomy | 3-Port Cholecystectomy Number (%) of Patients | ||
|---|---|---|---|
| Number (%) of Patients | P Value | ||
| Biliary Dyskinesia | 6 (30) | 8 (40) | 0.37 |
| Symptomatic Cholelithiasis | 10 (50) | 9 (45) | 0.5 |
| Acute Cholecystitis | 4 (20) | 3 (15) | 0.5 |
Three-Port Cholecystectomy
Neither open conversion nor placement of additional ports was required. Two intraoperative cholangiograms were performed; no choledocholithiasis was identified.
Eighteen of 20 patients were discharged home on the same day of surgery. One patient stayed for 1 day, and 1 patient stayed for 2 days after surgery with no major complications occurring. One patient had a postoperative biloma found 1 week after surgery, necessitating percutaneous drainage and endoscopic retrograde cholangiography with stent placement. Recovery proceeded without complication.
Single-Port Cholecystectomy
The first 2 cases, both for acalculous biliary dyskinesia, that were attempted with the single-port technique required placement of an additional subcostal port for completion due to difficulty with elevating the gallbladder and liver. Subsequently, the operative technique was changed where the instrument used to elevate the gallbladder was placed on the fundus rather than the infundibulum, and a Prolene suture was used for retraction of the infundibulum. Therefore, the next 20 patients underwent a single-port laparoscopic cholecystectomy without the need for additional ports or open conversion. No gross gallstone or spillage of bile occurred as a result of the Prolene retraction suture. One intraoperative cholangiogram was performed with no evidence of choledocholithiasis. Of the 4 acute cholecystitis patients who underwent single-port surgery, 2 patients had hydrops. Due to severe inflammation, a drain was placed in the gallbladder bed and brought out through the umbilicus in these select cases.
Sixteen of 20 patients were discharged home on the same day. Of the remaining 4 patients, 2 remained in the hospital for 1 day, 1 patient stayed for 2 days, and 1 stayed for 4 days after surgery. The 4-day stay was required for the anticoagulation needs of the patient.
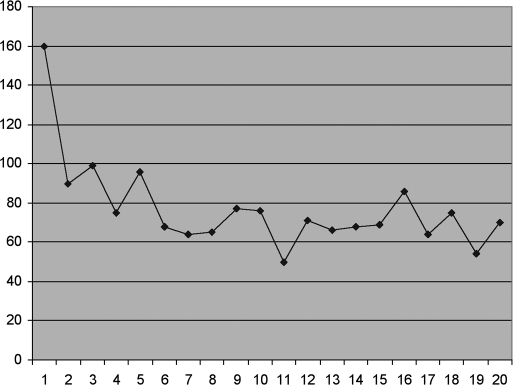
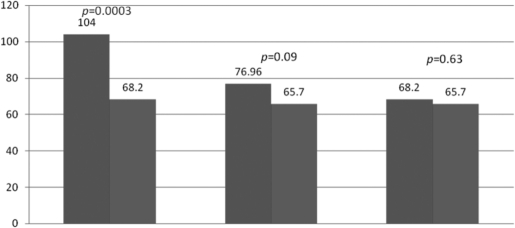
The operative times for the 20 successful single-port cases are shown in Figure 3. No significant postoperative complications were noted. The mean operative time for our first 5 cases was 104 minutes, while the mean operative time for the next 15 cases was 68.2 minutes. The operative times of single-port compared with 3-port cholecystectomy are reviewed in Figure 4. The mean time of the last 15 single-port cases had comparable operative times to the 3-port cholecystectomy.
Figure 3.
Operative times. Patient 9 had an intraoperative cholangiogram performed. Patients 10, 12, 14, and 16 had acute cholecystitis. Insert labels for figure 3: x-axis = Patient y-axis = Operative Time (min)
Figure 4.
Comparison of single port cholecystectomy operating times versus 3-port cholecystectomy operating times. SPC = single port cholecystectomies; 3-Port = 3-port cholecystectomies. Insert labels for figure 4: y axis = Operating Time (min) × axis beneath bar 1 from the left = First 5 SPC × axis bar 2 = Last 15 SPC × axis bar 3 = Total SPC × axis bar 4 = 3-Port × axis bar 5 = Last 15 SPC × axis bar 6 = 3-Port
DISCUSSION
Traditionally, laparoscopic cholecystectomy has been performed using multiple ports around the abdomen. In single-port laparoscopic cholecystectomy, the incision is placed in the peri-umbilical skin fold, and the entire procedure is completed without additional port incisions. This permits a nearly scarless operation. Any port incision has potential complications, although the rate of incidence varies with the port size and type. Port complications may include hernias (0.65% to 2.8%), abdominal wall bleeding (0.2%), bowel injury (0.06%), and wound infection (0.06%).5 Reducing the number of incisions from 4 to 1 should reduce the incidence of these morbidities. Furthermore, as previously studied in single-incision transumbilical laparoscopic cholecystectomy, using only the periumbilical port incision reduces the level of pain engendered by traditional 4-port laparoscopic surgery.6
Unlike prior published series,7 we performed single-port cholecystectomy on all types of biliary disease, including acute cholecystitis with inflammation. We did not exclude patients based on their medical comorbidities, and the average BMI of our single-port patients was 31, which is considered obese. Thus, this report represents a “real-world” consecutive series in which single-port cholecystectomy was applied to all candidates for laparoscopic procedures rather than only a select group.
Single-port cholecystectomy requires a permutation in technique from traditional laparoscopic cholecystectomy. The failure of the first 2-single port cases resulted from attempting to use the same retraction techniques of a 3-port gallbladder. By the third attempt, the proper retraction technique needed to expose the cystic duct and artery had been identified, thus allowing the completion of a single-port cholecystectomy. A subsequent improvement in operative times was seen over the next 5 cases as our learning curve diminished. The final 15 cases were performed with operative times comparable to those for our 3-port laparoscopic cholecystectomy. Because we have eliminated the additional surgical time associated with the placement of multiple ports, we anticipate that our operative times will continue to diminish to a level below that for our 3-port cholecystectomy.
The learning curve for single-port cholecystectomy primarily reflects the difficulty experienced in understanding the spatial restriction caused by the close proximity of the instruments and the camera. With multiple trocar surgery, the degree of instrument conflict is inversely related to the distance between port sites. However, in single-port surgery, all instruments pass through one fascial incision and therefore only one focal point. Consequently, spatial conflict is unavoidable and must be compensated for with learned technique. Although the basic strategy of gallbladder exposure as described in our paper may be easily conveyed, the learning curve is related to the surgeon's ability to discern and manage the spatial conflict of the instruments. The addition of articulating instruments may aid in this process; however, it does not eliminate the technical challenges associated with single-port surgery.
Our study was limited by the retrospective nature of the analysis. Future trials should address potential differences in pain, recovery time, and quality-of-life indicators between multi-port and single-port cholecystectomy. Furthermore, the learning curve described is specific to the author, a fellowship-trained laparoscopic surgeon, and may vary with the comfort level and technical skill of other surgeons. However, anecdotally from our personal experience in training other surgeons on this technique, we have seen that after being supervised for 5 cases the learning surgeon reaches an adequate level to perform single-port cholecystectomy independently and effectively.
CONCLUSION
We report the largest series of single-incision laparoscopic cholecystectomies performed to date. With a learning curve for a surgeon already experienced in multi-port laparoscopic cholecystectomy of approximately 5 cases, it is feasible that such a surgeon could perform single-incision laparoscopic cholecystectomy for both elective and urgent procedures with operative times consistent with 3-port cholecystectomy. The single-port approach has an obvious cosmetic benefit. Additional benefits may include decreased pain, lower hernia rates, and increased patient satisfaction. However, additional prospective trials are necessary to define these benefits.
References:
- 1.Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech. 1999;9:361–364 [DOI] [PubMed] [Google Scholar]
- 2.Rane A, Rao P, Rao P. Single-port-access nephrectomy and other laparoscopic urologic procedures using a novel laparoscopic port (R-Port). Urology. 2008;72(2):260–264 [DOI] [PubMed] [Google Scholar]
- 3.Desai MM, Rao PP, Aron M, Pascal-Haber G, Desai MR, Mishra S, Kaouk JH, Gill IS. Scarless single port transumbilical nephrectomy and pyeloplasty: first clinical report. BJU Int. 2008;101:83–88 [DOI] [PubMed] [Google Scholar]
- 4.Romanelli JR, Mark L, Omotosho PA. Single port laparoscopic cholecystectomy with the triport system: a case report. Surg Innov. 2008;15:223–228 [DOI] [PubMed] [Google Scholar]
- 5.Access-related complications – an analysis of 6023 consecutive laparoscopic hernia repairs. Minim Invasive Ther Allied Technol. 2001;10:23–29 [DOI] [PubMed] [Google Scholar]
- 6.Bresadola F, Pasqualucci A, Donini A, et al. Elective transumbilical compared with standard laparoscopic cholecystectomy. Eur J Surg. 1999;165(1):29–34 [DOI] [PubMed] [Google Scholar]
- 7.Cuesta MA, Berends F, Veenhof AA. The “invisible cholecystectomy”: a transumbilical laparoscopic operation without a scar. Surg Endosc. 22(5):1211–1213, 2008. May [DOI] [PubMed] [Google Scholar]