Abstract
Background and Objectives:
Preconditioning gas by humidification and warming the pneumoperitoneum improves laparoscopic outcomes. This prevents peritoneal desiccation and detrimental events related to traditional cold-dry gas. Few comparisons have been done comparing traditional cold-dry, heated-only, and humidified-warmed carbon dioxide.
Methods:
A prospective, controlled, randomized, double-blind study of laparoscopic gastric banding included 113 patients and compared traditional dry-cold (n=35) versus dry-heated (n=40), versus humidified-warm gas (n=38). Pain medications were standardized for all groups. Endpoints were recovery room length of stay, pain location, pain intensity, and total pain medications used postoperatively for up to 10 days.
Results:
The humidified-warmed group had statistically significant differences from the other 2 groups with improvement in all end points. The dry-heated group had significantly more pain medication use and increased shoulder and chest pain than the other 2 groups had.
Conclusion:
Using warm-humidified gas for laparoscopic gastric banding reduces shoulder pain, shortens recovery room length of stay, and decreases pain medication requirements for up to 10 days postoperatively. Dry-heated gas may cause additional complications as is indicated by the increase in pain medication use and pain intensity.
Keywords: Pneumoperitoneum, Insuflow®, Pain, Lap-Band, Desiccation, Humidified
INTRODUCTION
The acceptability of the laparoscopic adjustable gastric banding (lap-band) procedure for obesity is well recognized by both surgeons and patients for many reasons. Laparoscopic surgical methods and variations have been advanced to improve outcomes, reduce pain, shorten recovery, reduce complications, and improve quality of life. The outcome of laparoscopic procedures has focused on the nature of the disease process, patient selection, technical aspects of the procedure performed, and surgeon skills without regard to the quality of gas used to create the intraabdominal operating space. Changing the quality of carbon dioxide (CO2) used to create and maintain pneumoperitoneum by preconditioning the gas with humidification and warming has been shown to improve laparoscopic outcomes for Roux-en-Y gastric bypass procedures using the Insuflow gas conditioning technology.1 Although it would not be anticipated that the outcome of a laparoscopic Roux-en-Y gastric bypass procedure compared with a lap-band would be different, a clinical trial is best to assert scientific findings. In addition, no study to our knowledge has been done comparing different qualities of gas used for laparoscopic gastric banding procedures. The focus of this study is to evaluate in a prospective, randomized, controlled study postoperative outcomes of pain, narcotic (opioid equivalent) use with 10-day follow-up of patients having laparoscopic gastric banding comparing traditional dry-cold, dry-warmed, and humidified-warmed gas.
MATERIALS AND METHODS
This study was performed at the Surgery Center of Richardson, Richardson, Texas, and was approved by its Institutional Review Board. The authors performed all procedures and anesthesia instillation. The study was compliant with all HIPAA regulations. Data regarding past abdominal surgery, comorbidities, demographics, and anthropometry was obtained preoperatively. There was no specific intervention or change in usual practices during the study. Eligibility inclusion criteria included National Institutes of Health criteria for bariatric surgery (including BMI of 40 to 60 kg/m2 or 35 to 39 kg/m2 with associated obesity-related comorbidities), acceptable operative risk (including good cardiopulmonary function and overall health status), and willingness to sign the informed consent and follow the study protocol including the follow-up assessments. Exclusion criteria included prior upper abdominal surgery, except cholecystectomy, large abdominal ventral hernia, patients with hiatal hernia, minors, and pregnant women. Informed written consent was obtained from all patients. Randomization to 1 of the 3 groups was done using a computerized software algorithm random-number generator. The group assignment was unknown by any of the investigators throughout the entire study (surgery through 10-day follow-up). A total of 113 (n=113) patients, 101 females and 12 males, were enrolled. The surgical procedure was the same for each participant in all groups, being the pars flaccida approach as previously described.2 One surgeon (RB) performed all surgeries. The only difference was the use of dry-cold (dc), dry-warmed (dw), or humidified-warmed (hw) gas for the pneumoperitoneum. The study was done as a prospective, controlled, randomized, double-blind study of laparoscopic gastric banding comparing traditional dry-cold (n=35) versus dry-heated only [Stryker Heated Insufflator Tubing (620 – 030-407)] (n=40) vs. humidified-warm [LEXION Medical, Insuflow® gas conditioning system (6198)] 35° Centigrade/95% relative humidity (rh) (n=38). Pain medications were given based on pain and nausea scores by using an 11-point verbal rating scale (VRS), with 0 being = none to 10 = maximal, at 15-minute intervals until discharge. VRS scores were standardized for all groups based on their postoperative score, and analgesic medication usage was converted to morphine equivalents. Shoulder and abdominal pain were scored and tracked separately. After discharge, patients self-administered their pain medication, self-scored the level of pain, and recorded this information for follow-up assessment. All patients were in American Society of Anesthesiology (ASA) classification I or II. Postoperative follow-up was done by the surgeon and his staff. All participants completed treatment, and 10-day follow-up as allocated by their study group. No data were excluded from analysis. A sample size of 30 for each group was determined to be necessary to have a high probability (power) of detecting statistically significant and clinically important differences of outcomes. Statistical assessment was done by testing for differences in treatment group outcomes using parametric and nonparametric tests for differences in means and differences in variances. P values were generated from t tests by using pooled (Lilliefors test) or separate (Wilcoxon rank sum) variance. A P≤0.05 was considered significant.
RESULTS
Ages ranged from 21 years to 61 years. BMI ranged from 35 to 55. Comorbidities included hypertension, diabetes, dyslipidemia, sleep apnea, arthralgia, and gastric reflux. No conversion from laparoscopy to laparotomy occurred in any group. No intraoperative or postoperative complications occurred. All patients went home the same day of surgery. No protocol violations occurred. The length of the operation was similar for all groups, with the dry-cold group ranging from 18 minutes to 52 minutes with a mean of 31 minutes, the Insuflow® group ranging 14 minutes to 48 minutes with a mean of 28 minutes, and the dry-heated only group ranging from 19 minutes to 50 minutes with a mean of 30 minutes. The total volume of gas used during the procedures averaged 32.2 liters (L) for the humidified-warm group, 28.2L for the dry-warm group, and 31.6L for the dry-cold group. Recovery room time to discharge was significantly shorter for the Insuflow group compared with both other groups. The dry-cold group ranged from 62 minutes to 262 minutes with a mean of 153, the Insuflow group ranged from 76 minutes to 200 minutes with a mean of 138 minutes, and the dry-warm group ranged from 78 minutes to 270 minutes with a mean of 160 minutes (Table 1).
Table 1.
Comparison of Surgery Time, Recovery Room Time, Postoperative Pain Medication Use, Postoperative Shoulder Pain Score
| Humidified Warm CO2 Insuflow® Group (n=38) | Dry Warm CO2 Stryker Group (n=40) | Dry Cold CO2 Standard Group (n=35) | P Value | |
|---|---|---|---|---|
| Surgery Time [mean min (range)] | 28 (14–48) | 30 (19–50) | 31 (18–52) | |
| Volume of Gas (L) | 32.3 | 28.2 | 31.6 | |
| Recovery Room Time [mean min (range)] | 138 (76–200) | 160 (78–270) | 153 (62–262) | <0.05 |
| Morphine Equivalent (mg) | ||||
| Recovery room | 5.1 | 9.2 | 7.7 | <0.01 |
| Day 1 | 4.5 | 6.4 | 6.7 | <0.05 |
| Day 2 | 2.5 | 4.4 | 4.8 | <0.05 |
| Day 3 | 1.5 | 3.2 | 3.4 | <0.05 |
| Day 5 | 0.9 | 3.1 | 3.5 | <0.01 |
| Day 7 | 0.2 | 1.9 | 1.7 | <0.01 |
| Day 10 | 0.2 | 1.9 | 0.5 | <0.01 |
| Postoperative Shoulder Pain Score | 3.8 | 7.3 | 6.7 | <0.01 |
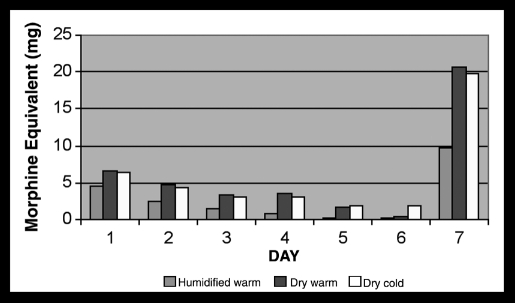
Medication requirements for the Insuflow vs. dry-heated and Insuflow vs. dry-cold groups was statistical significantly less, P<0.05 total morphine requirements. The total morphine requirements for the Insuflow group was less than half that for the dry-warm and dry-cold groups (Figures 1). VRS pain score comparisons and statistical evaluations comparing each group showed a statistically significant reduction in pain scores for the Insuflow group (based on VAS scoring). Humidified-warmed Insuflow® produced the lowest pain scores compared to dry-cold and dry-warm and combined (P<0.05). The dry-cold conventional group had pain scores higher than the humidified-warmed P<0.05 and less than the dry-heated group. The dry-heated Stryker group had the highest pain scores compared with dry-cold and humidified-warmed P<0.05.
Figure 1.
Humidified-warm vs dry-cold vs dry-warm medication requirements. The humidified-warm group used statistically significantly less pain medication on all days. The dry-cold group had significantly improved outcomes compared with the dry-warm group.
DISCUSSION
Shoulder pain is a well-recognized common problem in gastric banding and other laparoscopic procedures.3–5 Shoulder pain is so common that it is specifically mentioned on hospital and patient Web sites and included in preoperative counseling materials given to patients by physicians, clinics, and hospitals. Laparoscopic pain is not improved by only heating the gas and is reported to be made worse.6–8 Use of the Insuflow device significantly reduces laparoscopic pain and reduces opioid medication compared with conventional and warmed-only CO2.9 Improvement in clinical outcomes using Insuflow has also been shown for laparoscopic cholecystectomy and Roux-en-Y procedures.1,10,11 Many studies1,9–15 show clinical improvements using humidified-warmed gas compared with traditional cold-dry gas. Conditioning the gas to 95% rh and close to body temperature (35°C) mimics the normal condition of the peritoneal cavity to maintain a physiologic homeostatic environment preventing tissue desiccation that results in an acute inflammatory response. The extreme dryness of the gas initiates evaporation and desiccation, causing peritoneal cell stress, releasing acute-phase reactive inflammatory materials like interleukin-6 (IL-6) and C-reactive protein (CRP) that are associated with pain.16,17 Desiccation of the peritoneum during laparoscopy causes adhesion formation that is reduced by using humidified-warmed carbon dioxide.18
Improved well-being extending to 14 days when the Insu-flow device is used has been reported compared with traditional gas in cholecystectomy and gynecology patients.9–11,15 Prevention of peritoneal desiccation as a cause of inflammation and trauma is the significant factor related to these findings. The dryness of the gas in the unconditioned state whether cold or warmed is 5000 times dryer than desert conditions, because it has <200 parts per million of water vapor or 0.0002% rh. This causes rapid loss of water content of the peritoneal fluid resulting in laparoscopic hypothermia due to evaporations and leads to peritoneal cell desiccation. The stress of desiccation caused an inflammatory response inducing release of interleukin-6, CRP, tumor necrosis factor-alpha and other lymphokines, cytokines, and prostaglandins indicative of cellular trauma.16 The results are increased requirements for pain medication up to 10 days after surgery in the dry-cold and dry-warm groups compared with the humidified-warm group, and the warmed-only gas has higher pain scores and more medication use than dry-cold gas alone or compared with the dry-cold and humidified-warm separately.
The cost of the Insuflow humidified warmed device is similar to the Stryker dry-heated tubing. Both cost more than standard tubing. However, the standard tubing does nothing but transport dry-cold gas from the insufflator to the patient. The dry-heated tubing only changes the temperature of the gas. The humidified-warmed device changes the extremely dry gas to normal homeostatic levels and also warms the gas. As this study demonstrates, there is a clinical difference in that the humidified-warmed gas significantly changes and improves outcomes. It was also noted that there is cost savings with the humidified-warmed gas because of the reduced recovery time and increasing utilization.
CONCLUSION
Changing the quality of the gas used for laparoscopy, making it physiologically humidified and warmed to 95°F and 95% relative humidity results in statistically significant improved outcomes extending up to 10 days compared with cold-dry or warm-dry gas. Dry heated-only gas may cause additional complications due to the increase in pain medication and pain intensity. When dry gas, cold or warmed, was compared, cold-dry gas was found to be less harmful to patients. This comparative study of the quality of gas used for the pneumoperitoneum showed that the combination of the lap-band procedure and the Insuflow device offered the best surgical outcome regarding pain, opioid use, and extended follow-up. From the evidence found in this study, humidified-warmed gas for the pneumoperitoneum significantly improved clinical outcomes by reducing postoperative pain, reducing the use of morphine equivalents, and improving quality of life immediately in the postoperative recovery with improved early convalescence.
References:
- 1.Hamza M, Schneider B, White P, et al. Heated and humidified insufflation during laparoscopic gastric bypass surgery: effect on temperature, postoperative pain, and recovery outcomes. J Laparoendosc Adv Surg Tech. 2005;15:6–12 [DOI] [PubMed] [Google Scholar]
- 2.Ren C, Fielding G. Laparoscopic adjustable gastric banding: surgical technique. J Laparoendosc Surg. 2003;13:257–263 [DOI] [PubMed] [Google Scholar]
- 3.Li TC, Saravelos H, Richmond M, Cooke ID. Complications of laparoscopic pelvic surgery: recognition, management and prevention. Hum Reprod Update. 1997;3:505–515 [DOI] [PubMed] [Google Scholar]
- 4.Alexander JI. Pain after laparoscopy. Br J Anaesth. 1997;79:369–378 [DOI] [PubMed] [Google Scholar]
- 5.Dixon JB, Reuben Y, Halket C, O'Brien PE. Shoulder pain is a common problem following laparoscopic adjustable gastric band surgery. Obes Surg. 2005;15:1111–1117 [DOI] [PubMed] [Google Scholar]
- 6.Slim K, Bousquet J, Kwiatkowski F, Lescure G, Pezet D, Chipponi J. Effect of CO2 gas warming on pain after laparoscopic surgery: a randomized double-blind controlled trial. Surg Endosc. 1999;13:1110–1114 [DOI] [PubMed] [Google Scholar]
- 7.Saad S, Minor I, Mohri T, Nagelschmidt M. The clinical impact of warmed insufflation carbon dioxide gas for laparoscopic cholecystectomy. Surg Endosc. 2000;14:787–790 [DOI] [PubMed] [Google Scholar]
- 8.Wills VL, Hunt DR, Armstrong A. A randomized controlled trial assessing the effect of heated carbon dioxide for insufflation on pain and recovery after laparoscopic fundoplication. Surg Endosc. 2001;15:166–170 [DOI] [PubMed] [Google Scholar]
- 9.Beste T, Daucher J, Holbert D. Humidified compared with dry, heated carbon dioxide at laparoscopy to reduce pain. Obstet Gynecol. 2006;107:263–268 [DOI] [PubMed] [Google Scholar]
- 10.Mouton WG, Bessell JR, Millard SH, Baxter PS, Maddern GJ. A randomized controlled trial assessing the benefit of humidified insufflation gas during laparoscopic surgery. Surg Endosc. 1999;13:106–108 [DOI] [PubMed] [Google Scholar]
- 11.Mouton WG, Bessell JR, Otten KT, Maddern GJ. Pain after laparoscopy. Surg Endosc. 1999;13:445–448 [DOI] [PubMed] [Google Scholar]
- 12.Ott D, Reich H, Love B, et al. Reduction of laparoscopic-induced hypothermia, postoperative pain and recovery room length of stay by pre-conditioning gas with the Insuflow device: a prospective randomized controlled multi-center study. JSLS. 1998;2:321–329 [PMC free article] [PubMed] [Google Scholar]
- 13.Demco L. Effect of heating and humidifying gas on patients undergoing awake laparoscopy. J Am Assoc Gynecol Laparosc. 2001;8:247–251 [DOI] [PubMed] [Google Scholar]
- 14.Almeida O. Awake microlaparoscopy wit the Insuflow device. JSLS. 2003;6:199–201 [PMC free article] [PubMed] [Google Scholar]
- 15.Farley R, Greenlee S, Larson D, Harrington J. Double-blind, prospective, randomized study of warmed, humidified carbon dioxide insufflation vs standard carbon dioxide for patients undergoing laparoscopic cholecystectomy. Arch Surg. 2004;139:739–744 [DOI] [PubMed] [Google Scholar]
- 16.Ott D. Desertification of the peritoneum by thin-film evaporation during laparoscopy. JSLS. 2003;7:189–195 [PMC free article] [PubMed] [Google Scholar]
- 17.Elenkov IJ, Iezzoni DG, Daly A, Harris AG, Chrousos GP. Cytokine dysregulation, inflammation and well-being. Neuroimmunomodulation. 2005;12:255–269 [DOI] [PubMed] [Google Scholar]
- 18.Binda M, Molinas C, Hansen P, Koninckx P. Effect of desiccation and temperature during laparoscopy on adhesion formation in mice. Fert Stert. 2006;86:166–175 [DOI] [PubMed] [Google Scholar]