Abstract
Background:
The prevalence of gallstone disease in the community makes it an important area of service in district general hospitals. Laparoscopic surgical techniques in synergy with modern imaging and endoscopic and interventional techniques have revolutionized the treatment of gallstone disease, making it possible to provide prompt and definitive care to patients.
Methods:
Patients with gallstone disease were treated based on a predetermined protocol by a special-interest team depending on the patient's mode of presentation. Data were collected and analyzed prospectively.
Results:
Our team treated 1332 patients with gallstone disease between September 1999 and December 2007. Patients (249) with acute symptoms presented through Accident and Emergency (A&E). Despite varied presentations, laparoscopic treatment was possible in all but 8 patients. The study comprised 696 patients who underwent laparoscopic cholecystectomy (LC) as in-hospital (23 hour) cases in a stand-alone center, and 257 outpatients and 379 inpatients. Sixty-seven patients with acute cholecystitis had their surgery within 96 hours of acute presentation. Seventy patients had laparoscopic subtotal cholecystectomy. The overall morbidity was 2.33% with 3 patients having residual common bile duct stones; 3 patients had biliary leak from cystic or accessory duct stumps and one had idiopathic right segmental liver atrophy; 19 had wound infections, 5 had port-site hernia. No mortalities occurred during the 30-day follow-up.
Conclusion:
We believe that prompt investigation with imaging and endoscopic intervention if needed along with LC at the earliest safe opportunity by a specialized dedicated team represents an effective method for treating gallstone disease in district general hospitals. Our experience with over 1000 patients has offered us the courage of conviction to say that justice is finally here for gallstone sufferers.
Keywords: Gallstones, Cholecystectomy, Laparoscopic
INTRODUCTION
Gallstone disease remains a common and significant cause of suffering in most parts of the world. It has been reported that there are 5.5 million gallstone sufferers in the UK and that over 50 000 cholecystectomies are performed each year1 with 15% of patients being symptomatic over a period of 15 years.2 Treatment of gallstone disease therefore continues to remain an important area of service in the peripheral district general hospital setting. Paradigm shifts in the concepts governing the management of gallstone disease are necessary to provide prompt and definitive care in most cases to enable patients to return to the community and to their productive lives. We discuss our philosophy and experience of having treated 1332 patients with gallstone disease in a National Health Service (NHS) district general hospital over the last 8 years. An evidence-based multidisciplinary approach together with incorporation of imaging and endoscopic and minimal access surgical techniques is the key to providing expected standards of care to patients.
METHODS
Gallstone disease can present in a variety of clinical scenarios, and the mode of management needs to be tailored to the manifestation of the condition. Our basis of management of gallstone disease has been the evidence-based consensus that definitive treatment should be provided as early as is feasible if not in the very same admission to prevent symptom recurrence or complications. We have endeavored to build a team of professionals with interest and experience in this field. An option to refer cases to this team was also provided to other surgeons in the hospital who formed part of the Accident and Emergency (A&E) cover but had other areas of special interest. Patients were treated based on a predetermined protocol depending on their mode of presentation (Table 1).
Table 1.
Protocol Followed in Management of Patients With Gallstone Disease
| Case Scenario | Mode of Presentation | Management Plan* |
|---|---|---|
| A | Presentation with history and chronic symptoms of gallstone disease or Gallstones diagnosed on community ultrasound | LFT and Imaging (US +/−MRI) to confirm diagnosis and normal CBD and proceed to planned LC. |
| B | Cholelithiasis with severe biliary pain or acute cholecystitis | LC within 96 hours |
| C | Cholelithiasis with choledocholithiasis | ERCP with clearance of common bile duct stones followed by LC as early as possible after watching for development of ERCP-related complications |
| D | Cholelithiasis with gallstone pancreatitis | LC as soon as patient is symptom free and biochemical parameters are normal. CT scan 7 days after onset of symptoms to rule out pancreatic necrosis or if evidence of infection. |
Patients referred as outpatients with a diagnosis of gallstones or with symptoms suggestive of gallstone disease were investigated for the presence of abnormalities in liver function, common bile duct stones, and biliary tract obstruction before being booked for surgery. Those presenting through our A&E services with symptoms or signs suggestive of gallstone disease were investigated with blood investigations including liver function tests (LFT), resuscitated, and treated supportively. They had ultrasound scans (US) and/or magnetic resonance imaging (MRI) if required. Patients with dilated extrahepatic biliary tract or common bile duct stones had endoscopic retrograde cholangiopancreatography (ERCP) for clearance of obstruction before laparoscopic cholecystectomy at the earliest opportunity.
Laparoscopic cholecystectomy (LC) was performed using a standard technique with reusable instruments. One 10-mm epigastric port and three 5-mm ports were situated in the umbilicus, right subcostal, and right flank regions, respectively. Pneumoperitoneum was achieved by Veress needle through the umbilicus with a standard insufflation pressure of 14 mm Hg. Lower pressures (10 mm to 12 mm) were used for patients with cardiovascular insufficiency. Calot's triangle dissection was performed with diathermy and hook dissection. Medium large clips (Horizon Ligating Clips, Pilling Weck closure systems, Canada) were used to clip the cystic duct and cystic artery preferring to stay closer to the gallbladder. Gallbladder was hook dissected off the liver bed and retrieved through the epigastric port incision using a BERT bag (Vernon-Carus Ltd, Lancashire, UK).
In patients with a frozen Calot's triangle secondary to adhesions, risk of iatrogenic injury to the adjoining biliary ducts and blood vessels in the hilar region during dissection to identify the cystic duct and artery is high in either laparoscopic or open surgery. These patients had laparoscopic subtotal cholecystectomy (LSC) through the most proximal accessible part of Hartman's pouch or gallbladder neck by suturing closed or ligation of the stump using Vicryl Endoloop (Ethicon, Johnson & Johnson, Cincinnati, OH) after visual inspection of the stump lumen for any residual calculi and free flow of bile on milking with an atraumatic instrument. Anterior and posterior branches of the cystic artery were identified separately if possible and clipped. Failing this, they were ligated en mass with the cystic stump.
Patients were allowed to eat and drink immediately postoperatively and discharged as soon as comfortable on regular oral analgesics as needed. They were followed up as outpatients for 3 weeks before being finally discharged unless any outstanding findings were identified.
Data were prospectively collected by our team and regularly audited and discussed in relevant forums.
RESULTS
Our team had the opportunity to provide treatment to 1332 patients with various presentations of gallstone disease over the 7-year period between September 1999 and December 2007.
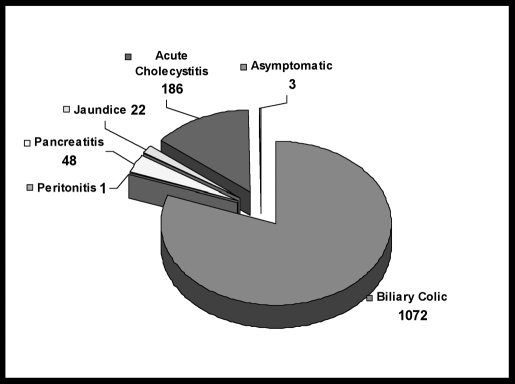
From the community, 1083 patients were referred to us with symptoms of gallstones or with asymptomatic gallstones having being diagnosed on imaging. Acute symptoms of gallstone disease were present in 249 patients who were admitted for treatment. Their presentations are outlined in Figure 1. Eight patients had empyema of the gallbladder, and 124 patients in the series had evidence to suggest biliary obstruction necessitating further imaging with MRI (30 patients). Endoscopic intervention with ERCP was needed in 92 patients before they could be schueduled for LC.
Figure 1.
Mode of presentation of gallstone disease.
The surgery could be completed laparoscopically in all except 8 patients who needed conversion to open surgery; 3 of these patients had intraabdominal adhesions and 5 had difficult anatomy. Seventy patients underwent LSC.
We had low morbidity in all cases. The overall morbidity was 2.33%. Among patients who underwent LC, 5 had residual stones in the common bile duct (CBD) necessitating further imaging and ERCP. One patient with a wide cystic duct had a bile leak from the sutured stump 48 hours after surgery. This was corrected by ERCP and stent insertion as well as laparoscopic lavage and drainage of the peritoneal contamination. The stent was removed 3 months later. Another patient had a bile leak from a loose Endoloop around the cystic stump following LSC. This was managed by laparoscopy and Endoloop reapplication with additional suturing of the stump to ensure a repair. One patient developed peritonitis from a bile leak from an accessory bile duct that necessitated a laparotomy for adequate drainage and peritoneal lavage.
One patient was re-referred with an incidentally noted derangement of LFT 13 months after emergency LC. Investigations did not reveal any damage to the biliary tract, but an MRI revealed features of right segmental liver atrophy suspected to be due to vascular injury. The patient was therefore referred to a specialist liver unit where a hepaticojejunostomy was advised and performed. The patient is well and asymptomatic but continues to have deranged LFTs for reasons that are still not fully understood.
No mortalities occurred in the 30-day follow-up. No patient required intervention or return to the operating theater for bleeding. Nineteen patients had wound infections that were treated conservatively. Five patients had epigastric port wound incisional hernia.
Sixty-seven of 186 patients with acute cholecystitis underwent surgery within 96 hours of acute presentation. The rest were delayed due to the need for recovery from pancreatitis and the need for further imaging or interventions.
Of 1332 patients who had LC, 684 were discharged within 23 hours of surgery; 253 were discharged home on the same day (Figure 2); 379 patients required inpatient LC either because they were treated as emergencies during an acute attack or because they did not fulfill criteria for a short stay or outpatient treatment. One patient had to be admitted from the outpatient surgery unit due to unexplained persistent postoperative hypotension that later resolved spontaneously. Three were admitted due to urinary retention. Twelve patients from the 23-hour cases stayed longer due to social and care-related issues including pain management.
Figure 2.
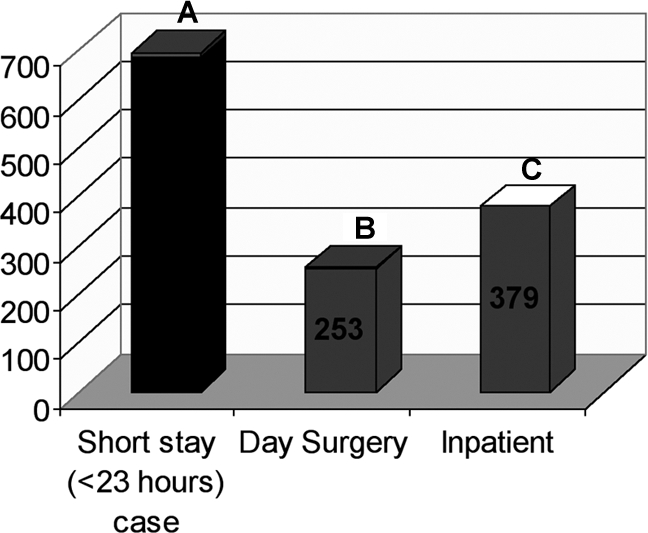
Mode of delivery of care and admission and discharge pattern for laparoscopic cholecystectomy. A: 684 cases; 12 discharge failures. B: 253 cases; 4 discharge failures. C: 379 cases.
The cost of providing the service was kept low by reducing the use of disposables to a minimum and a low complication rate. The only disposable instruments used were the scissor tips (Endocut Scissor tips, Microline Pentax Inc, Beverly, MA, USA) and endoscopic retrieval (BERT) bags. We consider this a good policy given the present need for economic and ecological prudence.
DISCUSSION
The prevalence of gallstone disease makes it imperative for responsibility of care to remain the domain of the generalist in the district general hospital, and referral to a specialist center is practicable only for difficult clinical cases. In spite of the uniform availability and growing skill and safety of LC, the provision of an acceptable standard of care in the NHS district general hospital setting based on current evidence requires multidisciplinary team-based management strategies to treat gallstone disease in all its forms using minimal access techniques. It would also benefit the patient if a surgeon agreeing to care for a patient with gallstone disease as part of his on-call commitment had an in-hospital special-interest team to refer the patient onward for definitive care. The specialist team would be able to give greater priority to the case than the receiving surgeon who is quite likely to be committed to targets specific to his area of special interest. This team will also be keen to keep abreast of new skills and methods evolving in the treatment of gallstones and therefore continue to provide optimal care to every patient seeking treatment from his local hospital.
Cholecystectomy has evolved over a span of a century from the initial open cholecystectomy described by Langenbuck in 1882 to LC described by French surgeon Phillipe Mouret of Lyon in March 1987.3,4 The introduction of modern imaging techniques and the widespread availability of LC has brought about a paradigm shift with regards to management of gallstone disease. Surgical options can now be offered even to elderly individuals who were previously denied open cholecystectomy due to comorbid features. Even with asymptomatic gallstones, the principle seems to have moved from “best left alone if not troublesome” to one that says, “leave alone only if you have to”! The recognition that a significant proportion of patients suffer repeated symptoms and complications has prompted this change. LC allows inspection of the gallbladder without the need for commitment to completion or a large abdominal incision.
Patients referred through the community have different treatment needs compared with those presenting as acute emergencies. Patients presenting through A&E had a varied spectrum of gallstone symptoms like acute cholecystitis, CBD stones, jaundice, pancreatitis, and other complications of gallstone disease5 and needed control of these before they could undergo LC. The challenge is to achieve these ideally within 4 days of onset of acute symptoms, which is by and large accepted as the best time for cholecystectomy in the acute setting though this can vary based on the surgeon's level of experience and the individual patient.6–9 The common problems that prevent immediate LC are obstruction of the CBD by stones, empyema of the gallbladder with sepsis, and pancreatitis. We were also bound by certain inherent methods in the health system with being able to coordinate investigations, surgical theater booking, and the availability of specialists to perform procedures due to tight advance scheduling of the above resource allocations.
Patients with CBD stones confirmed by imaging underwent ERCP at the earliest and then LC at the next available opportunity during regular hours.10 Those with pancreatitis without CBD stones were observed for clinical and biochemical recovery before having LC.11
Empyema of the gallbladder was treated by US-guided percutaneous drainage and interval cholecystectomy. This allows for resolution of systemic sepsis that could add to the morbidity if any surgery is undertaken under such circumstances.12 We feel that emergency LC is only useful in suspected perforation or gangrene of the gallbladder where drainage of the gallbladder alone would not be sufficient.13
Most outpatient referrals for gallstone disease can be safely treated either as outpatient cases or as short overnight (23 hour) in-hospital cases.14 Inpatient care would only be needed for those with medical comorbidities and social care needs for a smooth pre- and postoperative journey. Whilst we have endeavored to provide surgery at the earliest in this subgroup of patients, we were bound by list availability and fair prioritization inherent to the best institutions in the public health system.
The concept of LSC has gained increasing acceptance over the past decade. One of the commonest reasons for conversion from LC to open cholecystectomy used to be the discovery of a “frozen” Calot's triangle due to adhesions from previous attacks of cholecystitis. At this juncture, it would not be untrue to say that the risk of iatrogenic collateral biliary or vascular injury involved with dissection of a difficult frozen Calot's triangle is no higher with laparoscopic surgery than with conventional open surgery. We join many other peers in continuing with this concept of LSC, because we do not see any benefits in conversion to open surgery towards achieving a better result in such cases.15–20
Being able to choose and deliver effective treatment thus needs training,21 experience, and a team approach to the problem involving experts from the field of imaging, upper GI endoscopy, and minimal access surgery.
We believe that these principles can be easily adopted in most peripheral institutions with little additional cost and good results. Outpatient or short-stay treatment for most patients (71.5% in our cohort) reduced bed occupancy in the main hospital. This has a positive impact on the quality of life, the cost of health care provision, and the economy of the society at large.22 The promptness of therapy reduces the need for repeated outpatient visits and admissions due to recurrent attacks of symptoms from gallstone disease whilst returning patients quickly to their life and careers.
CONCLUSION
The treatment of gallstone disease has evolved from the singular option of having a major abdominal operation to present practice based on the latest interventional and minimal access surgery techniques. The treatment of gallstone disease continues to remain the bane of the generalist in district general hospitals. Though treatments by individuals with general interests may appear to give satisfactory results, optimum results and minimal complications are best achieved when treatment is delivered by a specialized multidisciplinary team of experts in the district hospital, who have good experience, commitment, and continued training in the management of gallstone disease.
Our results over the 8-year period of our study show that this approach can deliver good results, minimum morbidity, and maximum resource efficiency in an NHS district general hospital setting.
Prompt investigations with the appropriate modern imaging and endoscopic techniques to elucidate the problem with LC performed at the earliest safe opportunity is a safe and definitive method of treating gallstone disease.
Our experience with over 1000 patients has offered us the courage of conviction that long-awaited justice is finally here for gallstone sufferers.
References:
- 1. Beckingham IJ. ABC of diseases of liver, pancreas, and biliary system. Gallstone disease. BMJ. 2001;322(7278):91–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benign diseases of the biliary tract. In: Morris PJ, Wood WC, eds. Oxford Textbook of Surgery, Vol 2 2nd ed New York, NY: Oxford University Press; 2000;1670–1674 [Google Scholar]
- 3. Litynski GS. Profiles in laparoscopy: Mouret, Dubois, and Perissat: the laparoscopic breakthrough in Europe (1987–1988). JSLS. 1999;3(2):163–167 [PMC free article] [PubMed] [Google Scholar]
- 4. De U. Evolution of cholecystectomy: a tribute to Carl August Langenbuch. Indian J Surg. 2004;66:97–100 [Google Scholar]
- 5. Glasgow RE, Cho M, Hutter MM, Mulvihill SJ. The spectrum and cost of complicated gallstone disease in California. Arch Surg. 2000;135(9):1021–1025 [DOI] [PubMed] [Google Scholar]
- 6. Lau H, Lo CY, Patil NG, Yuen WK. Early versus delayed-interval laparoscopic cholecystectomy for acute cholecystitis: A meta analysis. Surg Endosc. 2006;20:82–87 [DOI] [PubMed] [Google Scholar]
- 7. Cheruvu CV, Eyre-Brook IA. Consequences of prolonged wait before gallbladder surgery. Ann R Coll Engl. 2002;84(1):20–22 [PMC free article] [PubMed] [Google Scholar]
- 8. Claudio Papi, Marco Catarci, Letizia D'Ambrosio, et al. Timing of cholecystectomy for acute calculous cholecystitis: a meta-analysis. Am J Gastroenterol. 2004;99(1):147–155 [DOI] [PubMed] [Google Scholar]
- 9. Somasekar K, Shankar PJ, Foster ME, Lewis MH. Costs of waiting for gall bladder surgery. Postgrad Med J. 2002;78(925):668–669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alimoglu O, Ozkan OV, Sahin M, Akcakaya A, Eryilmaz R, Bas G. Timing of cholecystectomy for acute biliary pancreatitis: outcomes of cholecystectomy on first admission and after recurrent biliary pancreatitis. World J Surg. 2003;27(3):256–259 [DOI] [PubMed] [Google Scholar]
- 11. Taylor E, Wong C. The optimal timing of laparoscopic cholecystectomy in mild gallstone pancreatitis. Am Surg. 2004;70(11):971–975 [PubMed] [Google Scholar]
- 12. Tseng LJ, Tsai CC, Mo LR, et al. Palliative percutaneous transhepatic gallbladder drainage of gallbladder empyema before laparoscopic cholecystectomy. Hepatogastroenterology. 2000;47(34):932–936 [PubMed] [Google Scholar]
- 13. Habib FA, Kolachalam RB, Khilnani R, Preventza O, Mittal VK. Role of laparoscopic cholecystectomy in the management of gangrenous cholecystitis. Am J Surg. 2001;181(1):71–75 [DOI] [PubMed] [Google Scholar]
- 14. Vuilleumier H, Halkic N. Laparoscopic cholecystectomy as a day surgery procedure: implementation and audit of 136 consecutive cases in a university hospital. World J Surg. 28(8):737–740, 2004 [DOI] [PubMed] [Google Scholar]
- 15. Palanivelu C, Rajan PS, Jani K, et al. Laparoscopic cholecystectomy in cirrhotic patients: the role of subtotal cholecystectomy and its variants. J Am Coll Surg. 2006;203(2):145–151 [DOI] [PubMed] [Google Scholar]
- 16. Ji W, Li LT, Li JS. Role of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. Hepatobiliary Pancreat Dis Int. 2006;5(4):584–589 [PubMed] [Google Scholar]
- 17. Beldi G, Glättli A. Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Endosc. 2003;17(9):1437–1439 [DOI] [PubMed] [Google Scholar]
- 18. Chowbey PK, Sharma A, Khullar R, Mann V, Baijal M, Vashistha A. Laparoscopic subtotal cholecystectomy: a review of 56 procedures. J Laparoendosc Adv Surg Tech A. 2000;10(1):31–34 [DOI] [PubMed] [Google Scholar]
- 19. Palanivelu C, Jani K, Maheshkumar GS. Single-center experience of laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2007;17(5):608–614 [DOI] [PubMed] [Google Scholar]
- 20. Sinha I, Smith ML, Safranek P, Dehn T, Booth M. Laparoscopic subtotal cholecystectomy without cystic duct ligation. Br J Surg. 2007;94(12):1527–1529 [DOI] [PubMed] [Google Scholar]
- 21. Ayerdi J, Wiseman J, Gupta SK, Simon SC. Training background as a factor in the conversion rate of laparoscopic cholecystectomy. Am Surg. 2001;67(8):780–785 [PubMed] [Google Scholar]
- 22. Rosen MJ, Malm JA, Tarnoff M, Zuccala K, Ponsky JL. Cost-effectiveness of ambulatory laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2001;11(3):182–184 [PubMed] [Google Scholar]