Abstract
Background and Objectives:
We sought to provide informed recommendations on transitioning from laparoscopic radical prostatectomy (LRP) to robotic-assisted radical prostatectomy (RAP) through a study of the da Vinci robot.
Methods:
We performed a cost-benefit analysis to determine the impact that purchasing a $1.5 million da Vinci robot with a $112,000 service contract per year and $200 per case of disposables would have on profits of a mature laparoscopic prostatectomy program.
Results:
Seventy-eight cases per year are needed to cover the costs of a purchased robot, while only 20 cases per year are needed if a robot is donated. Once robot costs are covered, increases in caseload lead to increased income. Profit is not feasible at centers performing fewer than 25 cases annually. A donated robot lessens costs and allows reasonable revenue without drastic increases in caseload.
Conclusions:
Our data suggest a high-volume LRP program can convert to RAP and maintain profits; however, the cost of the robot precludes equal income as that with LRP. Purchasing a robot is not fiscally viable in a low-volume program. Given comparable outcomes between LRP and RAP, hospitals need to decide whether market forces or the intangible benefits of robotics outweigh the expenses of obtaining and operating a robot.
Keywords: Carcinoma, Prostate, Robotics, Cost, Cost analysis, Prostatectomy
INTRODUCTION
First described in 2001,1,2 robotic-assisted radical prostatectomy (RAP) now constitutes a substantial portion of the minimally invasive prostatectomy market, as 2 new hospitals acquire a da Vinci robot per week (Intuitive Surgical, personal communication October 2006). The benefits associated with transitioning from open radical retropubic prostatectomy (RRP) to either RAP or laparoscopic radical prostatectomy (LRP) have been well described: shorter length of stay and less blood loss.3–8 Overall, though, the outcomes of LRP and RAP are equivalent, and most mature series report blood loss of 200 mL to 300 mL per case with a 1 day to 2 day length of stay.9–11
Many centers adopt RAP because of the ease with which surgeons can transition from open surgery using the da Vinci robot, thereby rapidly realizing the aforementioned benefits of minimally invasive surgery; however, a mature LRP program already enjoys these improved outcomes. Faced with possible erosion of their market share to RAP programs, institutions and surgeons performing LRP must decide whether they should adopt an expensive technology without necessarily improving their results.
Lotan et al9 demonstrate that RRP is more cost effective than LRP and substantially more cost effective than RAP, and Scales et al10 show that RAP only becomes cost effective in specific markets and at surgical volumes that are not feasible for most centers. On the other hand, little data exist on the economics of converting from LRP to RAP, and thus there is little information to guide an LRP program as to whether it should purchase a da Vinci robot. We performed a cost benefit analysis of obtaining a da Vinci robot at a mature LRP program to offer informed recommendations on transitioning from LRP to RAP.
METHODS
A cost-benefit analysis was performed using single-institutional data on caseload, operative times, and profits for LRP. The cost of the da Vinci robot was obtained from Intuitive Surgical. This analysis utilized the $1.5 million da Vinci-S robot. The cost of the robot was amortized over 5 years; thus, the robot costs $300,000 per year and the service contract is $112,000 per year. The cost of disposables is $200 per case, more than current practice at our institution.
A profit of $5,409 per case was utilized in the analysis, and multiplying this by annual case volume yields total annual profit. The total annual profits less costs of the da Vinci robot equals the annual profitability of RAP. Variable annual case volume of 25 to 250 cases per year was utilized in our model. Calculations were also made if the robot was donated, whereby the institution pays for disposable equipment and the service contract, but not the da Vinci robot.9 The primary outcome was profit per case in 2005 dollars.
This model excludes the learning curve for RAP. After the learning curve, it was assumed that LRP and RAP would take the same amount of operating time and thus the operating room and anesthesia-associated costs to perform RAP are identical to the current practice of LRP. Considering no distinct CPT code exists for RAP, reimbursement was considered equal between LRP and RAP. Furthermore, length of stay (LOS), blood loss, operative time, room turnover time, and all oncologic outcomes were considered equivalent between LRP and RAP. The associated costs of resident involvement in these cases were not assessed. Cost-benefit analysis was performed using Microsoft Excel 2003.
RESULTS
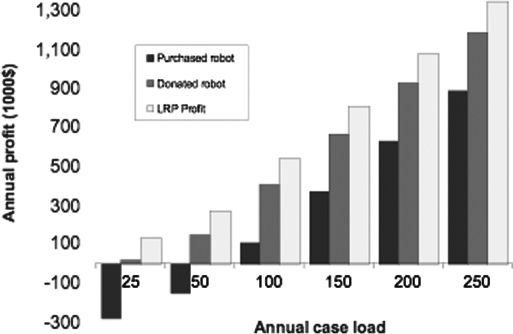
Purchase of a robot reduces income by at least $415,000 per year, due to the cost of the device and the service contract. Donation of a robot lessens the financial impact by $300,000 per year. If an institution maintains an identical caseload when switching from LRP to RAP, then it cannot maintain equivalent profits as illustrated in Figure 1. This holds true even if the robot is donated.
Figure 1.
Annual Profit of laparoscopic radical prostatectomy as a function of caseload.
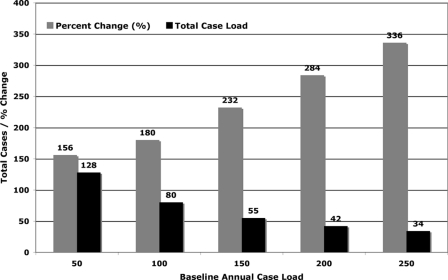
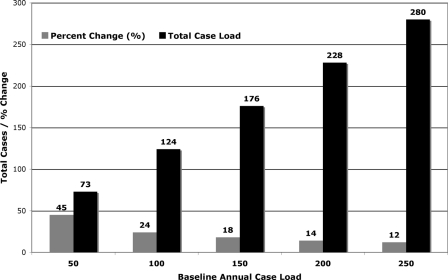
To maintain profits, an increase in caseload is needed to cover the added costs of the robot. Figure 2 shows the annual caseload, compared with baseline case volume, needed to maintain profitability if a robot is purchased. The equivalent data for donation of a robot is shown in Figure 3. At all levels of baseline productivity, purchase of a robot requires a greater case volume to maintain profits, relative to donation of a robot. Centers that perform a high volume of LRP at baseline need to only make small increases in total case volume to maintain profit, while centers with low volumes at baseline need to make very large changes in operative volume to cover the additional costs of robotics.
Figure 2.
Annual Caseload to Maintain Profits with Purchase of Robot
Figure 3.
Annual Caseload to Maintain Profits with Donation of Robot
DISCUSSION
Robotic surgery allows novice laparoscopic surgeons to rapidly incorporate minimally invasive surgery into their armamentarium, and urologists have been leaders in this movement. Robotic surgery is associated with more intuitive instruments and operative skills than laparoscopy is; however, this comes with a price tag in excess of $1 million just for an operative robot. Patient demand has fueled the explosion of RAP in the last 5 years, while convincing evidence that RAP leads to outcomes that are superior to LRP outcomes is absent. Concurrently, LRP has not blossomed and constitutes a small percentage of the overall prostatectomy market in the United States.
Other authors have investigated the economics of converting to LRP or RAP from open surgery and in that comparison a shorter LOS, less blood loss, and fewer transfusions are critical benefits of the minimally invasive approach.10,11 In our analysis, we consider a mature LRP program, where these benefits are incurred costs that cannot be recovered, and whether adopting robotic technology makes financial sense for such a program. The decisive factor for a mature LRP program will likely involve market share relative to rival institutions that offer RAP, as opposed to the true benefit of RAP over LRP.
Like an airline making money with an airplane, the robot will only pay for itself if it is used at a high volume. This distinction is profound if an institution is fiscally responsible for the entire cost of the robot and even more pronounced in a low volume center. A center loses money until it performs 78 RAP per year, at which point the robot and its service contract are paid for. The impact of this relationship cannot be understated, considering 85% of urologists perform fewer than 30 prostatectomies per year,12 and only 7% of all hospitals are high-volume prostatectomy centers, performing over 54 prostatectomies per year.13 Thus, a low-volume prostatectomy center may not overcome the learning curve for RAP rapidly, taking 1 or even 2 years to master the technique. In a geographic region with a small population base, such as ours, there may not be a sufficient number of patients with localized prostate cancer who are even eligible for RAP to make up the difference in caseload needed to maintain profits. With such economic pressures clearly involved in conversion to RAP, there are significant ramifications for providers and patients.
Our analysis has several limitations. Foremost, we utilized data from a single institution, and we used average profit per case as our financial outcome. We did not use costs in our analysis, and rather subtracted the expense of the robot from existing profits, as the additional costs of the robot would be paid for by the current profits from LRP. We did not use charges, as these vary as to who is paying the bill and are subject to wide local variation.
We did not stratify our results based on specific OR time as others have, and rather used total annual case volume as our benchmark. Although OR time is costly, and there will be variation in operative time between LRP and RAP, published results suggest this is a small difference when an LRP program converts to RAP.14,15
Exclusion of the learning curve from our analysis is also a limitation. Not only is the surgeon learning curve an important aspect of adopting a new technology, the operating team adapting to robotics entails costs. Removing these costs from our analysis makes RAP appear more profitable than it really is. Though the learning curve is a short-lived phenomenon at a high-volume center, it may take several months or even years at a low-volume center, where the costs may be substantial.16
Finally, we did not consider the impact that residents or fellows have on costs. Data illustrating the effect of residents and fellows on operative times and on the learning curve for RAP are lacking in the literature, and our data may be most applicable to a setting where trainees are not an integral part of such cases.
CONCLUSION
Our data suggest that a high volume LRP program can convert to RAP and maintain reasonable profits; however, equal profit with LRP is not possible without a dramatic increase in caseload. Certainly if a moderateto high-volume program maintains its caseload after obtaining a robot then it will still be profitable, although less so than before adopting RAP. Given comparable outcomes between LRP and RAP, hospitals need to decide whether market forces or the intangible benefits of robotics outweigh the expenses of obtaining and operating a robot.
Contributor Information
Peter L. Steinberg, Section of Urology Dartmouth Hitchcock Medical Center, Lebanon, New Hampshire, USA..
Paul A. Merguerian, Pediatric Urology, Dartmouth Hitchcock Medical Center, Lebanon, New Hampshire, USA..
William Bihrle, III, Section of Urology Dartmouth Hitchcock Medical Center, Lebanon, New Hampshire, USA..
John A. Heaney, Section of Urology Dartmouth Hitchcock Medical Center, Lebanon, New Hampshire, USA..
John D. Seigne, Section of Urology Dartmouth Hitchcock Medical Center, Lebanon, New Hampshire, USA..
References:
- 1.Binder J, Kramer W. Robotically assisted laparoscopic radical prostatectomy. BJU Int. 2001;87:408–410 [DOI] [PubMed] [Google Scholar]
- 2.Pasticier G, Rietbergen JB, Guillonneau B, Fromont G, Menon M, Vallancien G. Robotically assisted laparoscopic radical prostatectomy: feasibility study in men. Eur Urol. 2001;40:70–74 [DOI] [PubMed] [Google Scholar]
- 3.Ahlering TE, Woo D, Eichel L, Lee DI, Edwards R, Skarecky DW. Robot-assisted versus open radical prostatectomy: a comparison of one surgeon's outcomes. Urology. 2004;63:819–822 [DOI] [PubMed] [Google Scholar]
- 4.Tewari A, Srivasatava A, Menon M. Members of the VIP Team A prospective comparison of radical retropubic and robot-assisted prostatectomy: experience in one institution. BJU Int. 2003;92:205–210 [DOI] [PubMed] [Google Scholar]
- 5.El-Hakim A, Tweari A. Robotic prostatectomy–a review. Med Gen Med. 2004;6:20. [PMC free article] [PubMed] [Google Scholar]
- 6.Menon M, Shrivastava A, Tewari A. Laparoscopic radical prostatectomy: conventional and robotic. Urology. 2005;66:101–104 [DOI] [PubMed] [Google Scholar]
- 7.Ficarra V, Cavalleri S, Novara G, Aragona M, Artibani W. Evidence from robot-assisted laparoscopic radical prostatectomy: a systematic review. Eur Urol. 2007;51:45–56 [DOI] [PubMed] [Google Scholar]
- 8.Tooher R, Swindle P, Woo H, Miller J, Maddern G. Laparoscopic radical prostatectomy for localized prostate cancer: a systematic review of comparative studies. J Urol. 2006;175:2011–2017 [DOI] [PubMed] [Google Scholar]
- 9.Lotan Y, Cadeddu JA, Gettman MT. The new economics of radical prostatectomy: cost comparison of open, laparoscopic and robot assisted techniques. J Urol. 2004;172:1431–1435 [DOI] [PubMed] [Google Scholar]
- 10.Scales CD, Jr., Jones PJ, Eisenstein EL, Preminger GM, Albala DM. Local cost structures and the economics of robot assisted radical prostatectomy. J Urol. 2005;174:2323–2329 [DOI] [PubMed] [Google Scholar]
- 11.Denberg TD, Flanigan RC, Kim FJ, Hoffman RM, Steiner JF. Self-reported volume of radical prostatectomies among urologists in the USA. BJU Int. 2007;99:339–343 [DOI] [PubMed] [Google Scholar]
- 12.Ellison LM, Heaney JA, Birkmeyer JD. The effect of hospital volume on mortality and resource use after radical prostatectomy. J Urol. 2000;163:867–869 [PubMed] [Google Scholar]
- 13.Hu JC, Nelson RA, Wilson TG, et al. Perioperative complications of laparoscopic and robotic assisted laparoscopic radical prostatectomy. J Urol. 2006;175:541–546 [DOI] [PubMed] [Google Scholar]
- 14.Menon M, Shrivastava A, Tewari A, et al. Laparoscopic and robot assisted radical prostatectomy: establishment of a structured program and preliminary analysis of outcomes. J Urol. 2002;168:945–949 [DOI] [PubMed] [Google Scholar]
- 15.Herrell SD, Smith JA., Jr Robotic-assisted laparoscopic prostatectomy: what is the learning curve? Urology. 2005;66:105–107 [DOI] [PubMed] [Google Scholar]