Abstract
Background:
Meckel's diverticulum was first described about 400 years ago and continues to be a rare congenital disorder. Laparoscopic surgery for Meckel's diverticulum has been described in mostly case reports. We present our series of patients with symptomatic Meckel's diverticulum.
Methods:
We have treated 12 patients with symptomatic Meckel's diverticulum from 1994 through 2006 at our institution. All the patients presented with features of either appendicitis or peritonitis, some with a vague abdominal mass. Clinical diagnosis of Meckel's diverticulum was made in only 4 patients. Diagnostic laparoscopy confirmed Meckel's diverticulitis in all patients. Laparoscopic stapler resection of the lesions was performed for all patients, tangential excision in 10 and wedge excision in 2.
Results:
The incidence of Meckel's diverticulum at our institution is 0.3%. The majority of patients were male children. There were no staple-line leaks in any case. All patients recovered well postoperatively, and the day of discharge was in the range of the fourth to the seventh POD. Heterotopic gastric mucosa was found in the majority of the diverticula. Eight patients were followed up for 24 months, and 4 patients reported for follow-up after 45 months and were found to be symptom-free.
Discussion:
The diagnosis of Meckel's diverticulitis is rarely made preoperatively. Surgical resection is indicated only if the diverticulum is symptomatic or if the base is narrow. Traditionally, open wedge resection (including the anterior wall of the ileum) of the diverticulum is the treatment. We think that a simple tangential stapler resection can also be performed, with good outcome.
Conclusion:
Laparoscopy is useful in both diagnosis and treatment. Laparoscopic resection of Meckel's diverticulum is feasible and ideal, especially when performed in specialized centers.
Keywords: Meckel's diverticulitis, Perforation, Laparoscopy, Endostaplers
INTRODUCTION
Meckel's diverticulum is a rare condition. Its incidence is usually quoted as approximately 2% of the population, but the prevalence can vary from 0.2% to 2%.1 The male to female ratio of symptomatic diverticulum is 3:1. It is a diverticular remnant of the omphalomesenteric duct located on the antimesenteric border of the ileum, a short distance from the cecum (60 cm proximal to the ileocecal valve). On average, the diverticulum is 2.99-cm long and 1.92-cm wide. Although jejunal, colonic, rectal, pancreatic, duodenal, and endometrial tissues have all been found in the diverticulum, the heterotopic mucosa is likely to be gastric in origin in 80% of cases.2 As a result, the gastric acid secreted from this lining erodes tissue ultimately causing hemorrhage. Diagnosis of a bleeding Meckel's diverticulum is established by technetium Tc 99m-pertechnate scan (“Meckel scan”). Laparoscopy, however, is the most accurate diagnostic tool.3 Laparoscopic resection of perforated Meckel's diverticulum in a patient with clinical symptoms of acute appendicitis was first reported in 1992 by Ng et al.4 Here, we present our experiences with symptomatic Meckel's diverticulum in a series of adult and pediatric patients managed successfully by laparoscopy.
METHODS
Between 1994 and 2006, we treated 12 patients with symptomatic Meckel's diverticula. Two patients were found to have asymptomatic Meckel's diverticula during surgery for appendicitis. Excision was not performed for them, nor did they receive any prophylactic antibiotics. Patients were mostly male children. Five children presented with lower abdominal pain, nausea, vomiting, and fever. Three of them had, in addition, bloody stools. None of the adult patients had abnormal stools. Physical examination showed an ill-defined mass in the right lower quadrant, in the vicinity of the umbilicus in 4 patients. A clinical diagnosis of Meckel's diverticulitis was made in these 4 patients, and for the other 8 patients a diagnosis of appendicitis was made. Plain X-ray of the abdomen showed no evidence of air under the right diaphragm. In 8 patients, ultrasonogram (USG) and computerized tomography scan (CT) revealed an inflammatory mass in the area of the appendix, suggestive of a diagnosis of appendicular perforation. In the other 4 patients, because the normal appendix was visualized separately from the mass, the possibility of Meckel's diverticulitis was entertained. Diagnostic laparoscopy was planned for all patients after adequate preoperative preparation. Intravenous antibiotics (cefotaxime 1000mg and ornidazole 500mg) were administered 1 hour before surgery.
Treatment
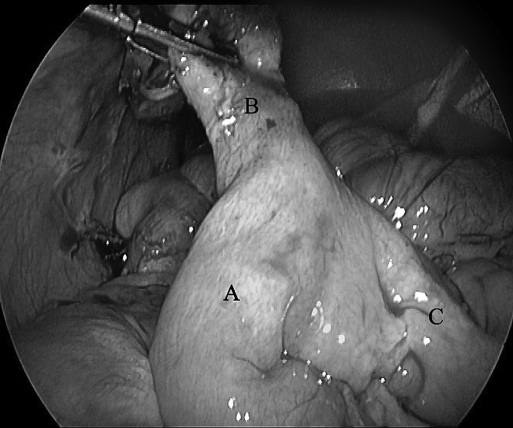
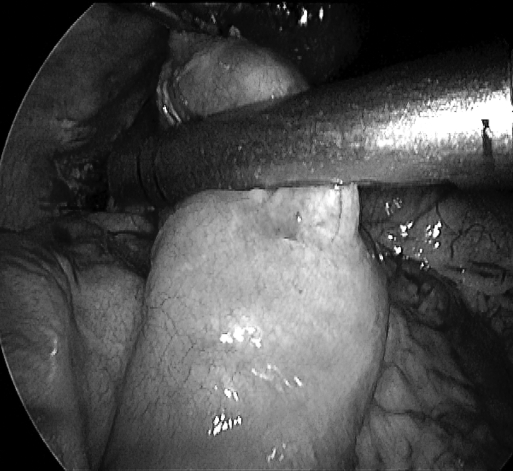
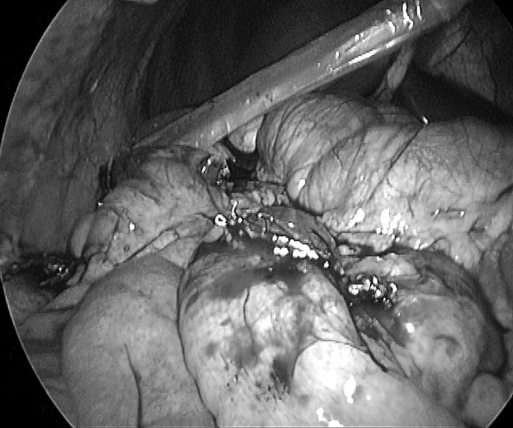
The open Hasson technique was used to establish pneumoperitoneum in all the patients, with the intra-abdominal pressure being maintained at 12mm Hg. A 10-mm trocar was inserted into the umbilicus; a 5-mm trocar was introduced in the suprapubic area, and another 5-mm trocar in the right lower quadrant, under direct vision. A 10-mm (30°) laparoscope was introduced into the 10-mm port for diagnostic laparoscopy. An inflammatory mass formed by the Meckel's diverticulitis was seen in 9 patients and perforated Meckel's diverticulum with localized peritonitis was seen in 3 patients (Figure 1). Few inflammatory flakes were seen on the bowels in the area. The appendix was normal in all patients. The 10-mm laparoscope was removed from the umbilical port and replaced with a 5-mm (30°) laparoscope introduced into the 5-mm suprapubic port. The camera surgeon stood to the left of the chief surgeon. The umbilical port was used for the right-hand instrument, and the right lower quadrant port was used for the left-hand instrument. The bowels were gently separated by using the tip of a suction nozzle, which revealed a pocket of pus and the perforated Meckel's diverticulum. A thorough peritoneal washing was performed, and the decision to resect the diverticulum was made. An endostapler (Endopath ETS-Flex 45 Endoscopic Articulating Linear Cutter, Ethicon, Inc. Cincinnati, OH) was introduced into a 12-mm trocar, replacing the 10-mm umbilical trocar. It was applied to the base of the diverticulum, perpendicular to the base of the diverticulum but transverse to the longitudinal axis of the bowel (Figure 2). The stapler was fired and the diverticulum was resected off the ileum (Figure 3). Small bleeding points at the edge of the staple line, if present, were sutured intracorporeally with 3 0 Vicryl. All the specimens were delivered through an enlarged 12-mm umbilical port with the use of an endobag. A wedge resection was performed for 2 patients where the base of the diverticulum was inflamed. Endostaplers were used for the excision, and bowel continuity was achieved by placing intracorporeal sutures with 2–0 Vicryl. Appendectomy was also performed for all the patients. A drainage tube was kept only in the 3 patients with the perforated diverticula.
Figure 1.
A: terminal ileum; B: inflamed Meckel diverticulum; C: proximal ileum.
Figure 2.
Application of the endostapler.
Figure 3.
Transverse staple line on the ileum after firing the endostapler.
RESULTS
A total of 6700 appendectomies were done between 1994 and 2006 at our institution. Out of this, 0.3% (20/6700) of patients had Meckel's diverticulum and 0.17% (12/6700) were symptomatic. The age range was 6 years to 43 years; there were 3 adults and 9 children, 8 males and 4 females. Perforation of Meckel's diverticulum was present in 3 patients and inflammation in 9 patients. The main findings are listed in Table 1. It can be seen that symptoms did not necessarily correlate with the diagnosis. For example, not all the patients with bloody stools had perforation. Operating time was in the range of 62 minutes to 110 minutes. The patient was allowed liquids orally between the third and fifth postoperative day (POD) and a soft diet thereafter. The drainage tube was removed on the second through the fourth POD. The day of discharge was in the range of the fourth through the seventh POD. There were no port-site hernias, intestinal obstruction, or leaks in any patient. One patient had infection of the umbilical wound, which was treated with the appropriate antibiotics. One patient had postoperative pneumonitis, treated with intravenous piperacillin/tazobactam for 5 days. Histopathology of the diverticulum showed heterotopic gastric mucosa in 11 (73%) patients, pancreatic tissue in 1 (27%) patient, evidence of acute inflammation in 9 patients, and perforation in 3 patients. Figure 4 shows the resected specimen, grossly edematous and inflamed. Eight patients were followed up for 24 months, and 4 patients reported for follow-up after 45 months and were found to be symptom free.
Table 1.
Patient Characteristics
| S No | Age & Sex | Symptoms & Signs* | Diagnosis | Surgery |
|---|---|---|---|---|
| 1 | 9 M | Pain, fever, nausea, blood in stools | Meckel's diverticulitis | Laparoscopic tangential excision |
| 2 | 6 M | Blood in stools | Meckel's diverticulitis | Laparoscopic tangential excision |
| 3 | 16 F | Localized peritonitis, mass | Diverticular perforation | Laparoscopic tangential excision |
| 4 | 32 M | Pain, fever, appetite loss, RIF tenderness | Meckel's diverticulitis | Wedge excision |
| 5 | 23 F | Pain, fever, vomiting, RIF tenderness | Meckel's diverticulitis | Laparoscopic tangential excision |
| 6 | 21 M | Localized peritonitis, mass | Diverticular perforation | Laparoscopic tangential excision |
| 7 | 6 M | Pain, fever, nausea | Meckel's diverticulitis | Laparoscopic tangential excision |
| 8 | 12 M | Blood in stools | Meckel's diverticulitis | Laparoscopic tangential excision |
| 9 | 10 F | Localized peritonitis, mass | Diverticular perforation | Wedge excision |
| 10 | 8 F | Pain, fever, blood in stools | Meckel's diverticulitis | Laparoscopic tangential excision |
| 11 | 14 M | Pain, fever, RIF tenderness | Meckel's diverticulitis | Laparoscopic tangential excision |
| 12 | 13 M | Pain, fever, vomiting, RIF tenderness | Meckel's diverticulitis | Laparoscopic tangential excision |
RIF = Right iliac fossa.
Figure 4.
Resected specimen.
DISCUSSION
Meckel's diverticulum is the most common form of congenital abnormality of the small intestine, resulting from an incomplete obliteration of the vitelline duct. Although originally described by Fabricius Hildanus in 1598, it is named after Johann Friedrich Meckel, who established its embryonic origin between 1808 and 1820.4 The tip of the diverticulum is free in 75% of cases, and in 25% the tip is attached to another organ or structure by means of a band.5 Most patients are asymptomatic, and it is usually an incidental finding when a barium study or laparotomy is performed for other abdominal conditions. In our series of 6700 laparoscopic appendectomies, there were 20 cases of Meckel's diverticula, out of which 12 were symptomatic. Complications include bowel obstruction (35%), hemorrhage (32%), diverticulitis (22%), umbilical fistula (10%), perforation (5%), other umbilical lesions (1%), and intussusception.6 Meckel's diverticulitis may mimic appendicitis, and the correct diagnosis is usually established at the time of laparotomy or laparoscopy. None of the clinical features are pathognomonic, and the diagnosis is rarely made preoperatively. Routine laboratory studies, such as leukocyte and erythrocyte counts, serum electrolytes, blood glucose, and urea serum creatinine, and coagulation screen were helpful in the general workup. These tests showed evidence of acute infection. CT and USG have been used to diagnose Meckel's diverticulum, but despite the availability of modern imaging techniques, the diagnosis is still challenging. So far, only case reports have been appearing in the literature regarding laparoscopic surgery for symptomatic Meckel's diverticula. Laparoscopy is especially more useful in this situation as it is clinically difficult to distinguish between diverticulitis and appendicitis.7 Laparoscopy revealed perforated Meckel's diverticulum in 3 cases and diverticulitis in the others. Definitive treatment of a complication, such as a bleeding, is the excision of the diverticulum. Successful resection of a Meckel's diverticulum can also be accomplished through laparoscopy, using endostapling devices.8 The advantages and benefits of minimal access surgery can be truly appreciated in children with symptomatic Meckel's diverticulum. Excision is mandatory for all symptomatic diverticula. With the advent of gastrointestinal stapling devices, excision has become safer, faster, and more efficient. Another advantage of stapling is that it closes the bowel lumen as it cuts, thereby completely reducing the chance of peritoneal contamination. The only drawback is the high cost. The contraindications for stapler excision is a very broad-based diverticulum or too short a diverticulum where a stapled excision cannot be technically performed.9 In case the diverticulum is too short, there is a danger of including too much of the ileum during stapling or leaving behind part of the diverticulum. Either way, both are undesirable. Another way to accomplish excision is to exteriorize the diverticulum via a minilaparotomy incision, stapler-resection and suturing closed the (common opening) enterotomy.10 In 2 patients, the base of the diverticulum was also inflamed; so a wedge resection including part of the normal ileum had to be performed. Provided the base of the diverticulum is not involved, it is our contention that tangential resection of the lesion alone will suffice. It is vital that the direction of the staple line lie perpendicular to the ileum and not on the longitudinal axis. This way, the ileal lumen will not be compromised while the stapler is being fixed at the base of the diverticulum. The reticulating head of the stapler is invaluable in these situations because it can be maneuvered precisely on the base of the diverticulum. Management of Meckel's diverticulum in asymptomatic patients is controversial because only about 4% develop complications. The only indications for excision of asymptomatic diverticula are size more than 5cm or presence of an omphalomesenteric band at the tip that has a risk of torsion.11 Stapler resection of asymptomatic diverticulum during surgery for unrelated disease has been shown to produce no added morbidity.12 In our series, 2 patients with asymptomatic Meckel's diverticulum in whom we did not perform excision reported later with diverticulitis. We performed a laparoscopic stapler diverticulectomy on them.
To summarize, a diagnosis of Meckel's diverticulitis is rarely made preoperatively, especially in adults. Tangential excision of a symptomatic Meckel's diverticulum using endostaplers is sufficient, provided the base is normal. Otherwise, wedge resection or segmental bowel resection is recommended. Asymptomatic diverticula can be left in situ. Appendectomy should be performed in all patients with Meckel's diverticulitis.
CONCLUSION
Laparoscopy seems to have a definite role in both adult and pediatric patients with symptomatic Meckel's diverticulum, especially when the diagnosis is in doubt. Tangential excision of the diverticula with staplers seems to be adequate. It is crucial that the division be made transverse to the longitudinal axis of the small bowel. Laparoscopy also provides all the benefits of minimally invasive surgery like reduced morbidity, early discharge, and better cosmesis.
References:
- 1.Shalaby RY, Soliman SM, Fawy M, Samaha A. Laparoscopic management of Meckel's diverticulum in children. J Pediatr Surg. 2005;40:562–567 [DOI] [PubMed] [Google Scholar]
- 2.Schmid SW, Schafer M, Krahenbuhl L, Buchler MW. The role of laparoscopy in symptomatic Meckel's diverticulum. Surg Endosc. 1999;13:1047–1049 [DOI] [PubMed] [Google Scholar]
- 3.Memon AA, Memon GA, Ansari AG, Ghumro AA. Symptomatic Meckel's diverticulum. JCPSP. 1999;9:476–479 [Google Scholar]
- 4.Ng WT, Wong MK, Kong CK, Chan YT. Laparoscopic approach to Meckel's diverticulectomy. Br J Surg. 1992;79:973–974 [DOI] [PubMed] [Google Scholar]
- 5.Fansler RF. Laparoscopy in the management of Meckel's diverticulum. Surg Laparosc Endosc. 1996;6:231–233 [PubMed] [Google Scholar]
- 6.Cullen JJ, Kelly KA. Current management of Meckel's diverticulum. Adv Surg. 1996;29:207–214 [PubMed] [Google Scholar]
- 7.Attwood SE, McGrath J, Hill AD, Stephens RB. Laparoscopic approach to Meckel's diverticulectomy (comment). Br J Surg. 1992;79:211. [DOI] [PubMed] [Google Scholar]
- 8.Sanders LE. Laparoscopic treatment of Meckel's diverticulum. Obstruction and bleeding managed with minimal morbidity. Surg Endosc. 1995;9:724–727 [DOI] [PubMed] [Google Scholar]
- 9.Echenique M, Dominguez AS, Echenique I, Rivera V. Laparoscopic diagnosis and treatment of Meckel's diverticulum complicated by gastrointestinal bleeding. J Laparoendosc Surg. 1993;3:145–148 [DOI] [PubMed] [Google Scholar]
- 10.Huang CS, Lin LH. Laparascopic Meckel's diverticulectomy in infants: report of three cases. J Pediatr Surg. 1993;28:1486–1489 [DOI] [PubMed] [Google Scholar]
- 11.Ediz A. Laparoscopy-assisted resection of complicated Meckel's diverticulum. Surg Laparosc Endosc Percutan Tech. 2002;12:450–451 [DOI] [PubMed] [Google Scholar]
- 12.Ruh J, Paul A, Dirsch O, Kaun M, Broelsch CE. Laparoscopic resection of perforated Meckel's diverticulum in a patient with clinical symptoms of acute appendicitis. Surg Endosc. DOI: 10.1007/s00464-002-4207-4 [DOI] [PubMed] [Google Scholar]