Abstract
Background and Objectives:
The unfortunate complication of a colotomy resulting from a colonoscopic polypectomy can be disastrous. Using the versatility of laparoscopic surgery, we aim to provide a treatment algorithm for these colonoscopic perforations.
Methods:
We report a case of cecal perforation, in a 70 year old female, following colonoscopic polypectomy that was treated successfully with laparoscopic application of an Endo-GIA linear stapler.
Results:
Four months following staple resection of her cecal perforation, the patient is asymptomatic and has undergone a repeat colonoscopy without any sequelae.
Conclusions:
Laparoscopic techniques can be safely applied in the treatment of colonic perforations following therapeutic polypectomies. A suggested management algorithm is provided highlighting the role laparoscopy may provide in selected patients.
Keywords: Laparoscopy, Colonoscopy, Complications, Perforation
INTRODUCTION
Colon perforation during therapeutic colonoscopy has been estimated to occur at a rate of approximately 0.1% to 0.3%.1,2 Perforation may occur through a variety of mechanisms, including energy application at the polyp site, direct mechanical trauma from the tip of the endoscope, lateral pressure from the side of a bowed endoscope, and pneumatic injury from overinsufflation.3 Several case reports advocating laparoscopic repair of colonic perforation following colonoscopy have been described in the literature.4–16 In our present case report, we discuss the single application of an endoscopic linear stapler to close the perforation while preserving colonic lumen integrity in the presence of endoscopically placed mucosal clips.
CASE REPORT
A 70-year-old Caucasian female with a past medical history significant for sigmoid diverticulosis and previous benign polyps of the colon was found to have a lipomatous lesion in the ascending colon during routine surveillance colonoscopy. The patient was subsequently scheduled for a colonoscopy with endoscopic miniprobe ultrasound. A 30-mm sessile polyp was found in the cecum opposite the ileocecal valve. A complete resection of the polyp was performed using a 15-mL saline injection with India ink lift and a hot snare. After resection, the mucosal biopsy site was larger than anticipated, and it became difficult to maintain insufflation. An attempt to bridge the defect with 3 endoscopically placed clips was unsuccessful. The procedure was halted secondary to progressive abdominal pain and the clinical suspicion of a colonic perforation. The perforation was confirmed with the presence of substantial free air on radiographs. In this rare situation of early discovery and hemodynamic stability, the patient was taken immediately to the operating room for surgical repair.
In the operating theater, pneumoperitoneum was established with a Veress needle, and a 5-mm camera with an optical access trocar was placed in the left lower quadrant.
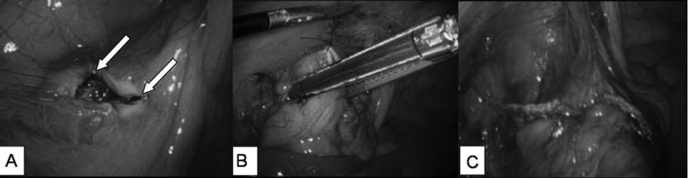
Of note, the abdominal pressure at initial access was measured at 10mm Hg, consistent with pneumoperitoneum from insufflation through the colotomy. A 5-mm anterior perforation of the cecum was clearly visible with an area of circumferential coagulation extending approximately 2 mm (Figure 1A). The cecum was noted to be adhered to the side wall, and hence one additional 5-mm port and one 10-mm port were placed for mobilization in the midline. The ports were placed in the umbilicus and the suprapubic position. After a sufficient segment of the cecum was freed, a single 3–0 silk stitch was placed to provide temporary closure and to provide a handle for elevation of the cecum. An Endo-GIA 60-mm blue load was applied to preserve the lumen of the cecum while incorporating the entirety of the defect including the area of coagulation necrosis (Figure 1B). The suture line incorporated healthy pink mucosa with preservation of the colonic lumen (Figure 1C). The abdomen was irrigated and the port sites closed. The patient had an uncomplicated recovery with discharge on hospital day 4. At the 4-month follow-up, the patient is without any complaints, tolerating a regular diet, and at baseline health. She has had an interval surveillance colonoscopy without any abnormalities and a well-healed polypectomy/surgical site.
Figure 1.
Operative Images Demonstrating Findings and Stapling Technique. A: Anterior cecal perforation with surrounding circumferential area of necrosis and endoscopically placed clips (white arrows). B: Endo-GIA 60 mm stapling with careful preservation of colonic lumen with incorporation of the entirety of the defect and area of coagulation necrosis. C: Final staple line showing colonic lumen integrity.
DISCUSSION
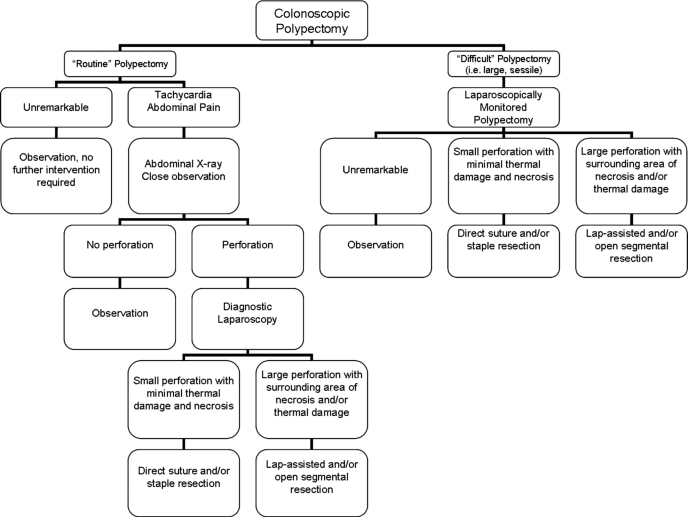
Colotomy that occurs during colonoscopy is a specialized subset of colon perforations for a variety of reasons. To begin with, in many cases the patient is under the care of a physician in a monitored setting with established intravenous access. Second, the patient has a prepped colon. Although there may be some question as to the precise benefits of mechanical preparation in elective colorectal surgery, in the emergent setting it may be advantageous in minimizing the amount of gross spillage. In addition, the endoscopist may provide localization of the suspected injury, allowing for more directed treatment. It has been advocated by some that colonoscopic polypectomy should be performed in conjunction with laparoscopy when a particularly difficult or suspicious polyp is anticipated.17,18 In keeping with the success of previous case reports and advances in minimally invasive techniques, we propose an active role of laparoscopy in complex colonoscopies as outlined in Figure 2.
Figure 2.
Algorithm Following Colonoscopic Polypectomy. Difficult polypectomies should be performed under laparoscopic monitoring. Perforations, depending upon their size, may be treated with direct suturing, staple resection or segmental resection.
Our approach to this cecal perforation was fundamentally the same as that for an appendectomy. The technical skills involved in the procedure are well within the capabilities of practicing general surgeons, but several technical tips merit further comment. In this case, primary repair with intracorporeal suturing was technically possible. However, it seemed ill advised, given the visible zone of coagulation necrosis surrounding the defect. In regards to the surgical stapler, it would have been technically easier to place a single firing across the cecum rather than 2 angled applications; however, 2 factors suggested multiple stapling1: the endoscopically placed clips may have interfered with proper staple line creation, and2 a single firing raised the concern for luminal compromise.
It may be argued that in this case the procedure was effective, but that minimally invasive techniques are not broadly applicable. No large series exists to offer guidance in the case of colonoscopic perforation. However, in the analogous situation of perforated appendicitis, there have been multiple studies in which laparoscopy does not have an increased rate of complications over open laparotomy.19–21 Conceptually, it seems there is little harm in starting with a diagnostic laparoscopy and proceeding based on the nature of the injury and the experience of the surgeon.
CONCLUSION
Many general surgeons will be confronted with the problem of colon perforation during colonoscopy. In the case presented here, we modified the established technique of laparoscopic appendectomy to the specific problem of cecal perforation and have demonstrated the feasibility of such an approach.
References:
- 1.Basson MD, Etter L, Panzini LA. Rates of colonoscopic perforation in current practice [letter]. Gastroenterology. 1998;114:1115. [DOI] [PubMed] [Google Scholar]
- 2.Waye JD, Lewis BS, Yessayan S. Colonoscopy: a prospective report of complications. J Clin Gastroenterol. 1992;15:347–351 [PubMed] [Google Scholar]
- 3.Kavic SM, Basson MD. Complications of endoscopy. Am J Surg. 2001;181:319–332 [DOI] [PubMed] [Google Scholar]
- 4.Mattei P, Alonso M, Justinich C. Laparoscopic repair of colon perforation after colonoscopy in children: report of 2 cases and review of the literature. J Ped Surg. 2005;40:1651–1653 [DOI] [PubMed] [Google Scholar]
- 5.Yamamoto A, Ibusuki K, Koga K, et al. Laparoscopic repair of colonic perforation associated with colonoscopy: use of passing sutures and endoscopic linear stapler. Surg Laparosc Endosc. 2001;11(1):19–21 [PubMed] [Google Scholar]
- 6.Wullstein C, Köppen, Gross E. Laparoscopic treatment of colonic perforations related to colonoscopy. Surg Endosc. 1999;13:484–487 [DOI] [PubMed] [Google Scholar]
- 7.Miyahara M, Kitano S, Shimoda K, et al. Laparoscopic repair of a colonic perforation sustained during colonoscopy. Surg Endsoc. 1996;10:352–353 [DOI] [PubMed] [Google Scholar]
- 8.Velez MA, Riff DS, Mule JM. Laparoscopic repair of a colonoscopic perforation. Surg Endosc. 1997;11:387–389 [DOI] [PubMed] [Google Scholar]
- 9.Alfonso-Ballester R, López-Mozos F, Martí-Obiol R, et al. Laparoscopic treatment of endoscopic sigmoid colon perforation. Surg Laparosc Endosc Percutan Tech. 2006;16:44–46 [DOI] [PubMed] [Google Scholar]
- 10.Schlinkert RT, Rasmussen TE. Laparoscopic repair of colonoscopic perforations of the colon. J Laparoendsoc Surg. 1994;4(1):51–54. [DOI] [PubMed] [Google Scholar]
- 11.Mehdi A, Closset J, Gay F, et al. Laparoscopic treatment of a sigmoid perforation after colonoscopy. Surg Endsoc. 1996;10:352–353 [DOI] [PubMed] [Google Scholar]
- 12.Hayashi K, Urata K, Munakata Y, et al. Laparoscopic closure for perforation of the sigmoid colon by endoscopic linear stapler. Surg Laparosc Endosc. 1996;6(5):411–413 [PubMed] [Google Scholar]
- 13.Goh PMY, Kum C-K, Chia Y-W, et al. Laparoscopic repair of perforation of the colon during colonoscopy. Gastrointest Endsoc. 1994;40(4):496–497 [DOI] [PubMed] [Google Scholar]
- 14.Fine A. Laparoscopically assisted surgery for colonic perforation with peritonitis – a case report. J Soc Laparoendosc Surg. 1998;2:189–190 [PMC free article] [PubMed] [Google Scholar]
- 15.Ibrahim IM, Sussman B, Wolodiger F, et al. Laparoscopic management of iatrogenic colonic perforation. N J Med. 1997;94(12):35–37 [PubMed] [Google Scholar]
- 16.Agresta F, Michelet I, Mainente P, et al. Laparoscopic management of colonoscopic perforations related to colonoscopy. Surg Endosc. 2000;14:592–593 [DOI] [PubMed] [Google Scholar]
- 17.Franklin JR ME, Diaz-E JA, Abrego D, Parra-Davila E, Glass JL. Laparoscopic-assisted colonoscopic polypectomy. Dis Colon Rectum. 2000;43(9):1246–1249 [DOI] [PubMed] [Google Scholar]
- 18.Bleier JI, Moon V, Feingold D, et al. Initial repair of iatrogenic colon perforation using laparoscopic methods. Surg Endosc. 2007; June 26; [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a meta-analysis. J Am Coll Surg. 1998;186:545–553 [DOI] [PubMed] [Google Scholar]
- 20.Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999;177:250–256 [DOI] [PubMed] [Google Scholar]
- 21.Kirshstein B, Bayme M, Domchik S, et al. Complicated appendicitis: laparoscopic or conventional surgery? World J Surg. 2007;31:744–749 [DOI] [PubMed] [Google Scholar]