Abstract
Background:
Laparoscopic cholecystectomy (LC) is the gold standard for gallstone disease. Many studies have confirmed the safety and feasibility of LC and have shown that it is comparable regarding complications to open cholecystectomy (OC).
The aim of this study was to evaluate the outcomes of LC including safety, feasibility in a resource-poor setting like Yemen, and also to compare the outcomes of LC with those of OC.
Methods:
This was a prospective, nonrandomized, comparative study of 112 patients who were admitted to Alburaihy Hospital with a diagnosis of gallstone disease and underwent cholecystectomy from July 1998 to March 2004. Hospital stay, duration of operation, postoperative analgesia, and morbidity due to wound infection, bile leak, common bile duct (CBD) injury, missed CBD stone, bleeding, subphrenic abscess, and hernia were evaluated. Patients were followed up on an outpatient basis.
Results:
Forty-nine patients underwent LC and 63 patients underwent OC. The mean age of LC patients was 43.96 years and of OC patients was 44.63 years. The 2 groups were similar in terms of age (p=0.740) and sex (p=0.535).
No significant difference was found in the incidence of acute cholecystitis between the 2 groups (p=0.000). The mean operative duration for LC was 39.88 minutes versus 56.76 minutes for OC (p=0.000), and the mean hospital stay was 1.63 and 5.38 days for LC and OC, respectively (p=0.000). A drain was used frequently in OC (p=0.000). LC patients needed less analgesia (p=0.000). The morbidity rate in LC was 12.2% versus 6.3% for OC, which was not statistically significant (p=0.394), (p>0.05). Wound infection and bile leak were more common with LC. No mortalities were reported in either group.
Conclusion:
An experienced surgeon can perform LC safely and successfully in a resource-limited setting. As in other studies, LC outcomes were better than OC outcomes.
Keywords: Gallbladder, Laparoscopic cholecystectomy, Open cholecystectomy, Cholecystectomy, Common hepatic duct, Common bile duct
INTRODUCTION
Laparoscopic cholecystectomy (LC) is the gold standard for the treatment of symptomatic and uncomplicated gallbladder stone disease.1 Its benefits over open cholecystectomy (OC) are well documented and accepted worldwide. It is safe, cost-effective, has rapid recovery times, superior cosmetic results, and comparable morbidity to that of OC.2–7 Most of these data come from developed countries where approximately 80% of all cholecystectomies are done laparoscopically.8 In contrast, Yemen is a resource-poor country with a primitive health care system and only a small number of government and private health centers offer laparoscopic surgery. A mere 5.1% of Yemen's already meager gross domestic product is spent on health care. There are only 0.33 doctors per 1000 persons and 5.9 hospital beds per 10 000 persons. With such constraints on health care infrastructure and training opportunities, one would expect this kind of service to be of limited application.9
LC is traditionally performed through 4 ports: 3 are 5 mm each and 1 is 10 mm. LC can also be performed using only three 5-mm ports (Mini LC). Standard 12-mm ports have been replaced by 2-mm ports, and experiments have been implemented to achieve cholecystectomy with no ports— known as the transgastric technique10 or natural orifice transluminal endoscopic surgery (NOTES).
OC is performed through right paramedian, midline and Kocher's incisions. This study evaluated the outcomes of 49 LC performed by the same consultant surgeon in a secondary referral center in Yemen, after acquiring laparoscopic training in Tyrol, Austria. The morbidities of the patients who underwent LC and those who underwent OC were compared.
METHODS
Between July 1998 and March 2004, 112 patients underwent either LC or OC for calculus cholecystitis at Alburaihy Hospital, Taiz, Yemen. A prospective review of patients undergoing LC (49 patients) and OC (63 patients) was performed.
Selection Criteria
All patients with confirmed gallstone disease, whether in acute or elective settings, were included. Patients with a preoperative diagnosis of calculus cholecystitis in addition to common bile duct (CBD) stones were excluded from the study. Patients with noncalculous cholecystitis, other gallbladder pathologies, and high-risk patients (comorbidities) were also excluded.
Study Design
This was a prospective, nonrandomized, comparative study. Each patient had a routine preoperative assessment by history, physical examination, and laboratory investigations. The benefits, risks, and complications of both procedures were explained to the patients, and they were given the choice of either operation. All provided informed consent, and LC patients gave consent for OC as well. Epidemiological and demographic matches were ensured. Outcome measures, such as duration of surgery, hospital stay, postoperative pain and analgesia, patient's morbidities including wound infection, bile leak, CBD injury, missed CBD stone, bleeding, subphrenic abscess, and hernia were recorded. Patients were followed up on an outpatient basis.
Laparoscopic Cholecystectomy
Cefuroxime 1.5 g was administered preoperatively to all patients. The Hasson technique was used to create pneumoperitoneum. The procedure was performed through 3 reusable ports: infraumbilical (10 mm), epigastric (5 mm), and right hypochondrium (5 mm). The cystic duct and cystic artery were identified, clipped, and cut. Dissection of the gallbladder was carried out using a hook dissector. The gallbladder was delivered through the infraumbilical port. Copious normal saline peritoneal irrigation was used at the end of procedure, and the ports were closed in the usual way after securing hemostasis.
Open Cholecystectomy
Cefuroxime 1.5 g was administered to all patients. The abdomen was opened by right paramedian incision. Identification of gallbladder anatomy and biliary system as well as Calot's triangle was ensured. Division of the peritoneum fold at the gallbladder neck was the first step in open skeletonization followed by identification of the cystic duct, common bile duct CBD, common hepatic duct, and cystic artery prior to double ligation and cutting of the cystic duct and artery. Silk sutures were used for double ligation. The dissection of the gallbladder was completed using finger dissection while dense adhesion to the gallbladder bed was freed by sharp dissection. Secured hemostasis was confirmed, and a drain was left in the subhepatic space in most cases. The paramedian wound was closed in layers.
RESULTS
The incidence of cholecystectomy was higher in females 78 (69%) than in males 34 (22%) (Table 1). The majority of patients (60%) were 30 years to 50 years of age. The mean age for LC was 43.96 years compared with 44.63 years for OC. The 2 groups were similar with respect to age (t test of significance: 0.740) (Table 1).
Table 1.
Patients' Characteristics and Data Related to the Surgical Procedure and Outcomes (N = 18)
| Parameters | Mean ± SD | Median | Percentile 25th, 75th | Range |
|---|---|---|---|---|
| Age (years) | 46.6 ± 4.4 | 47.5 | 43, 51 | 38–53 |
| Body Mass Index (kg/m2) | 25.4 ± 4.3 | 25 | 22.3, 27.9 | 19.3–34.9 |
| Parity | 1.8 ± 0.8 | 2 | 1, 2 | 0–3 |
| Surgical Procedure Length (min) | ||||
| Laparoscopic stage | 154 ± 41 | 140 | 130, 180 | 80–245 |
| Vaginal stage | 32 ± 20 | 30 | 15, 45 | 5–70 |
| Total | 186 ± 47 | 185 | 155, 230 | 90–260 |
| Volume of CO2 Insufflated (L) | 280 ± 131 | 300 | 185, 354 | 75–575 |
| Uterine Weight (g) | 575 ± 218 | 540 | 370, 776 | 280–1,015 |
| Difference of Hemoglobin Concentration | 1.5 ± 1 | 1.3 | 0.6, 2.2 | 0.1–3.5 |
| (Preoperative Value vs. Day 1 Value, g%) | ||||
| Length of Hospitalization (days) | 3.1 ± 0.9 | 3 | 3, 3 | 2–5 |
The mean duration of surgery was 39.8 minutes and 56.76 minutes for LC and OC, respectively. This was statistically significant (P=0.000). Forty-five cases (91%) of LC were performed in less than 60 minutes, while only 34 cases (53%) of OC were completed in less than 60 minutes. Indeed, only 3 (7%) LC took longer than 60 minutes, while 25 (39%) OC were completed in 60 minutes to 89 minutes. One case of OC was performed in more than 90 minutes (Table 1).
The mean hospital stay for LC and OC was 1.63 days versus 5.38 days. Forty-two LC patients (85%) were discharged on the first postoperative (PO) day, 5 (10%) patients stayed for 2 days, and 2 (5%) patients stayed for 1 week to 2 weeks. This is in stark contrast to the OC cohort where 45 (71%) patients were discharged on the fifth PO day, 15 (23%) on the sixth PO day, and 3 (6%) patients 1–2 weeks later. There was a significant difference in the hospital stay between the two groups (p=0.000) (Table 1).
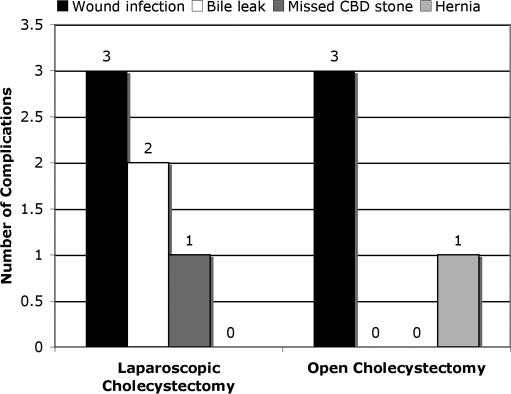
Five (10%) patients developed wound infection after LC compared with 2 (3.17%) patients for OC. Two LC operations (4%) were complicated by bile leak, while no bile leak was reported in OC cases. Only one (2%) case of missed CBD stone was confirmed after LC. One (1%) patient developed incisional hernia following OC. There were no CBD injuries, subphrenic abscess/hematoma, thromboembolic complications, or deaths in any case. (Table 1) (Figure 1).
Figure 1.
Postoperative complications.
Surgical drains were required in 60 (95.2%) OC cases compared with just 4 (8.2%) LC cases. The difference is quite significant (Table 1).
Paracetamol 500 mg TDS was needed in 5 (10%) LC patients. Another 33 (67.3%) and 11 (22.4%) LC patients needed paracetamol 500 mg TDS plus tramadol 100 mg BD, paracetamol 500mg+tramadol100mg BD+pethidine 100 mg BD to control the pain, respectively, while paracetamol 500 mg TDS+tramadol 100 mg BD, paracetamol 500 mg+tramadol 100 mg BD+pethidine 100 mg BD used in 30 (47.6%), 33 (52.4%) OC patients, respectively (Table 1). Paracetamol alone failed to control postoperative pain in any OC patients.
Nine (18.4%) cases of LC and 12 (19%) cases of OC were acute cholecystitis, and these patients were operated on within 72 hours of the onset of the symptoms. No significant difference was found between the 2 groups (Table 1).
The conversion rate was 4%. Two LC surgeries were converted to OC due to difficulty in identifying the anatomy and uncontrollable bleeding.
The average total cost for OC was 500 UK pounds ($950 USD), and 520 UK pounds ($1000 USD) for LC.
DISCUSSION
The efficacy of LC has been proven by countless studies and is regarded as the procedure of choice for gallstone disease despite the initial skepticism of many surgeons. Many authors have demonstrated the value of laparoscopic over open cholecystectomy with lower postoperative adhesion rates, faster recovery times, and shorter hospitalizations with marked social and economic advantages.10–14 Not only is LC a better operation than is OC, it has also been shown to safely supplant OC as the preferred modality for the management of symptomatic cholelithiasis in regional referral centers.15 However like many hot surgical issues, the debate continues. Moreover, 3 recent prospective studies16 comparing laparoscopic versus minilaparotomy demonstrate that the advantages of the laparoscopic approach in terms of cost and recovery speed are (with the exception of obese patients) much less evident than one would expect.
More than 95% of cholecystectomies in Yemen are performed by the open technique because of the lack of laparoscopic experience and the limited number of centers providing this service. Of major concern is the safety and efficacy of the procedure in a country where a definite shortage exists in health care resources and support. For example, because there are no endoscopic retrograde cholangiopancreatography (ERCP) facilities in Yemen, any cases of CBD stone have to be dealt with by open surgery. Also several social, educational, and financial factors force patients to choose the open method over the laparoscopic one. Although we have shown the difference in cost between the 2 operations to be minimal, the level of poverty in Yemen is such that, for most, even the small savings of $50 US made by opting for OC is preferable. There is also an inherent mistrust of “new” techniques among the majority of our patients who are illiterate and therefore unable to fully comprehend the benefits of LC proven elsewhere.
The major obstacle to implementing the new modern surgical techniques in Yemen is the lack of surgical education and training programs. Therefore, surgeons have to travel abroad to acquire the necessary experience in a specific field. The other major problem is who is going to help you in case of complications. This challenging situation has been overcome by the enthusiasm to develop new techniques, surgical experience, and the support of colleagues at Bezirkskrankenhaus BKH, Tyrol, Austria.
We were able to start laparoscopic surgery in such circumstances and our results have been acceptable. We present a single-center experience comparing the outcomes of the first series of LC with those of OC performed by the same surgeon.
As in other parts of the world, LC is performed more frequently in females. The age of the patients in the majority of cases was between 30 years to 50 years. Cholecystectomy for acute cholecystitis can be performed by either laparoscopic or open techniques without any major clinically relevant differences in postoperative outcomes. Both techniques offer low morbidity and rapid postoperative recovery.17 In acute settings, LC performed by experienced surgeons is a safe, effective technique for the treatment of acute cholecystitis. Patients treated within 48 hours of onset of symptoms experience a lower conversion rate to an open procedure, shorter operative time, and reduced hospitalization.18 About one-fifth of our patients (18%) presented acutely, and surgery was performed within 72 hours of the onset of the symptoms.
The duration of surgery in our LC and OC groups is comparable to that of other studies.19,20 Forty-five (91%) LC cases were completed in less than 60 minutes, which was a very good time for a beginner. Indeed, there were 20 (40%) cases performed in less than half an hour, while 60 (92%) cases of OC were completed in 30 minutes to 89 minutes.
Several factors can explain this relatively short operative time for a newly started LC program. Surgical experience and familiarity with OC is boosting the ability of the surgeon to identify the anatomy and to perform dissection safely to finish the procedure with increasing confidence. One of the causes of long procedure time is uncertainness about the anatomy, which may lead to iatrogenic injuries to the adjacent vital organs, which require subsequent management of these injuries. We found that past surgical experience with and mastery of OC was very helpful to reduce the operative time of LC. Good patient selection was another factor, as we included a relatively younger population (as compared with patients in aging Western communities) in our study and thus avoided patients with multiple comorbidities. We think that the well-trained team has contributed to the shorter operative time in our series.
The complications in our acute and elective operations were comparable. Regarding morbidity, previous studies have shown that the overall complication rate was significantly higher for OC.21 We had a higher wound infection rate with LC compared with OC. This was related to the use of reusable trocars. All 5 wound infection cases occurred in the first 34 LC patients, while the last 15 LC patients developed no wound infections because of improved sterilization techniques for instruments, gowns, and towels.
Of the 2 cases of bile leak post-LC, one patient was operated on in the acute setting while the other was done electively. These complications were related to difficulty in identifying the normal anatomy due to inflammation. Although significant bile leakage is an uncommon complication after biliary tract surgery, it may constitute a serious and difficult management problem.22,23 We managed both cases conservatively using drains. The leaks resolved within 2 weeks and the drains were removed. The first patient was a 62-year-old woman who was confirmed as having a retained CBD stone. She developed 3 episodes of jaundice in the first year and was reluctant to have any further intervention. The other patient was a 42-year-old man who was treated without further problems and did not develop biliary colic or deranged liver functions. The question of whether these 2 cases represented a CBD injury is difficult to answer, because we do not perform laparoscopic preoperative cholangiography routinely. We usually perform preoperative cholangiography for suspected or confirmed common bile duct stones pat. Once this diagnosis is confirmed, the procedure is converted to OC plus exploration of the CBD because we do not have ERCP facilities. These patients were not included in our series. Moreover, no intraoperative diagnosis of CBD stone was confirmed in our LC cohort and hence no intraoperative cholangiography was conducted for any LC patients.
We concluded that a complete preoperative diagnostic workup proved to be of fundamental importance for decreasing the incidence of residual bile duct stones, and therefore intraoperative cholangiography may be safely omitted during LC.24
The conversion rate was 4% (only 2 cases). The reasons for conversion were uncontrollable bleeding from the cystic artery in the first instance and inflammation and disturbed anatomy in the second patient.
Complications in the first year after OC included one incisional hernia in an obese patient, which was repaired by the open method. Two (3.17%) patients developed wound infection, which was resolved with drainage and antibiotics. Follow-up of both LC and OC patients showed no significant difference in the occurrence of postcholecystectomy syndrome. This has also been confirmed in other studies.25
CONCLUSION
A general surgeon can safely perform LC in a resource-limited setting thereby offering patients the advantages of short hospital stay, minimal pain, and speedy convalescence with early return to work and normal activity. Associated morbidities can be decreased further by performing more operations and adherence to the standard operative technique and acquiring operative skills.
References:
- 1.Mosimann F. Laparoscopic cholecystectomy has become the new gold standard for the management of symptomatic gallbladder stones. Hepatogastroenterology. 2006;53(69):1. [PubMed] [Google Scholar]
- 2.Victorzon M, Tolonen P, Vuorialho T. Day-case laparoscopic cholecystectomy: treatment of choice for selected patients? Surg Endosc. 2007;21(1):70–73 [DOI] [PubMed] [Google Scholar]
- 3.Kasem A, Paix A, Grandy-Smith S, El-Hasani S. Is laparoscopic cholecystectomy safe and acceptable as a day case procedure? J Laparoendosc Adv Surg Tech A. 2006;16(4):365–368 [DOI] [PubMed] [Google Scholar]
- 4.Kiely JM, Brannigan AE, Foley E, Cheema S, O'Brien W, Delaney PV. Day case laparoscopic cholecystectomy is feasible. Med Sci. 2001;170(2):98–99 [DOI] [PubMed] [Google Scholar]
- 5.Chok KS, Yuen WK, Lau H, Lee F, Fan ST. Outpatient laparoscopic cholecystectomy in Hong Kong Chinese—an outcome analysis. Asian J Surg. 2004;27(4):313–316 [DOI] [PubMed] [Google Scholar]
- 6.Kelley JE, Burrus RG, Burns RP, Graham LD, Chandler KE. Safety, efficacy, cost, and morbidity of laparoscopic versus open cholecystectomy: a prospective analysis of 228 consecutive patients. Am Surg. 1993;59(1):23–27 [PubMed] [Google Scholar]
- 7.Madan AK, Aliabadi-Wahle S, Tesi D, Flint LM, Steinberg SM. How early is early laparoscopic treatment of acute cholecystitis? Am J Surg. 2002;183(3):232–236 [DOI] [PubMed] [Google Scholar]
- 8.Teerawattananon Y, Mugford M. Is it worth offering a routine laparoscopic cholecystectomy in developing countries? A Thailand case study. Cost Eff Resour Alloc. 2005;31:3:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Core health indicators Available at: http//www.who.int/whosis/core/coreselectprocess.cfm Accessed 14/11/2006
- 10.Osborne DA, Alexander G, Boe B, Zervos EE. Laparoscopic cholecystectomy: past, present, and future. Surg Technol Int. 2006;15:81–85 [PubMed] [Google Scholar]
- 11.Testa S, Sfarzo A, Velluso A, Perretta LC, Cretella A, Caliendo RA. Laparoscopic cholecystectomy. Our experience. Minerva Chir. 2000;55(4):197–200 [PubMed] [Google Scholar]
- 12.Shamiyeh A, Wayand W. Current status of laparoscopic therapy of cholecystolithiasis and common bile duct stones. Dig Dis. 2005;23(2):119–126 [DOI] [PubMed] [Google Scholar]
- 13.Szabo G, Miko I, Peto K, Brath E, Nagy P, Gamal EM. Laparoscopic versus open cholecystectomy: reaction in the liver bed [in Hungarian]. Magy Seb. 2005;58(2):106–110 [PubMed] [Google Scholar]
- 14.Schietroma M, Carlei F, Liakos C, et al. Laparoscopic versus open cholecystectomy. An analysis of clinical and financial aspects. Panminerva Med. 2001;43(4):239–242 [PubMed] [Google Scholar]
- 15.Vagenas K, Karamanakos SN, Spyropoulos C, Panagiotopoulos S, Karanikolas M, Stavropoulos M. Laparoscopic cholecystectomy: a report from a single center. World J Gastroenterol. 2006;28:12(24):3887–3890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al Hadi FH, Chiedozi LC, Salem MM, George TV, Desouky M, Pasha SM. Comparison of laparoscopic and open cholecystectomy at Prince Abdulrahman Al Sudairy Hospital, Saudi Arabia East Afr Med J. 1998;75(9):536–539 [PubMed] [Google Scholar]
- 17.Boutelier P. Complications of laparoscopic cholecystectomy: evaluation study [in French]. Bull Acad Natl Med. 1998;182(3):617–629 [PubMed] [Google Scholar]
- 18.Johansson M, Thune A, Nelvin L, Stiernstam M, Westman B, Lundell L. Randomized clinical trial of open versus laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg. 2005;92(1):44–49 [DOI] [PubMed] [Google Scholar]
- 19.Dominguez EP, Giammar D, Baumert J, Ruiz O. A prospective study of bile leaks after laparoscopic cholecystectomy for acute cholecystitis. Am Surg. 2006;72(3):265–268 [PubMed] [Google Scholar]
- 20.Mcgee JM, Malnar KF, Bellefeuille CE, Berry BL, Katsis SB, Clingan FA. Longitudinal cholecystectomy study: patterns of care in a total community experience J Laparoendosc Adv Surg Tech A. 7(2):99–109, 1997 [DOI] [PubMed] [Google Scholar]
- 21.Porte RJ, De Vries BC. Laparoscopic versus open cholecystectomy: a prospective matched-cohort study. HPB Surg. 1996;9(2):71–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buanes T, Mjaland O. Complications in laparoscopic and open cholecystectomy: a prospective comparative trial. Surg Laparosc Endosc. 1996;6(4):266–272 [PubMed] [Google Scholar]
- 23.Agarwal N, Sharma BC, Garg S, Kumar R, Sarin SK. Endoscopic management of postoperative bile leaks. Hepatobiliary Pancreat Dis Int. 2006;5(2):273–277 [PubMed] [Google Scholar]
- 24.Uccheddu A, Pisanu A, Cois A, Cillara N. Can intraoperative cholangiography be avoided during laparoscopic cholecystectomy? Chir Ital. 2005;57(5):571–577 [PubMed] [Google Scholar]
- 25.Peterli R, Schuppisser JP, Herzog U, Ackermann C, Tondelli PE. Prevalence of postcholecystectomy symptoms: long-term outcome after open versus laparoscopic cholecystectomy. World J Surg. 2000;24(10):1232–1235 [DOI] [PubMed] [Google Scholar]