Abstract
Introduction:
Laparoscopic techniques are difficult to master, especially for surgeons who did not receive such training during residency. To help urologists master challenging laparoscopic skills, a unique 5-day mini-residency (M-R) program was established at the University of California, Irvine. The first 101 participants in this program were evaluated on their laparoscopic skills acquisition at the end of the 5-day experience.
Methods:
Two urologists are accepted per week into 1 of 4 training modules: (1) ureteroscopy/percutaneous renal access; (2) laparoscopic ablative renal surgery; (3) laparoscopic reconstructive renal surgery; and (4) robot-assisted prostatectomy. The program consists of didactic lectures, pelvic trainer and virtual reality simulator practice, animal and cadaver laboratory sessions, and observation or participation in human surgeries. Skills testing (ST) simulating open, laparoscopic, and robotic surgery is assessed in all of the M-R participants on training days 1 and 5. Tests include ring transfer, suture threading, cutting, and suturing. Performance is evaluated by an experienced observer using the Objective Structured Assessment of Technical Skill (OSATS) scoring system. Statistical methods used include the paired sample t test and analysis of variance at a confidence level of P≤0.05.
Results:
Between July 2003 and June 2005, 101 urologists participated in the M-R program. The mean participant age was 47 years (range, 31 to 70). The open surgical format had the highest ST scores followed by the robotic and then the laparoscopic formats. The final ST scores were significantly higher than the initial ST scores (P<0.05) for the laparoscopic (58 vs. 52) and the robotic (114 vs. 95) formats. Open surgical ST scores did not change significantly during the training program (191 vs. 194) (P=0.17).
Conclusion:
Laparoscopic and robotic ST scores, but not open ST scores, improved significantly during this intensive 5-day M-R program. The robotic ST scores demonstrated greater improvement than did the laparoscopic ST scores, suggesting that the transfer of laparoscopic skills may be improved using the robotic interface.
Keywords: Surgical education, Skills training, Laparoscopy, Robotic surgery
INTRODUCTION
The acquisition of laparoscopic skills requires a longer learning curve than that of open surgery. Acquiring these skills is challenging, particularly for postgraduate urologists who have not been exposed to laparoscopic procedures during their residency training. To assist urologists in developing their laparoscopic skills, 2-day and 3-day courses have been created. Although initial follow-up suggested that many participants (84%) were able to incorporate laparoscopy into their clinical practice, longer follow-up suggests that the skill acquisition is not durable.1,2 Five years after completing the course, only 54% of the participants were performing laparoscopic surgery.2 In contrast, all of the urologists who had a dedicated lengthy training period in laparoscopy (eg, 1-year fellowship) were performing an average of 25 laparoscopic cases per year.3 To help postgraduate urologists acquire laparoscopic surgical skills, an intensive 5-day mini-residency (M-R) program was created at the University of California, Irvine through a grant from Yamanouchi Pharma America (now Astellas Pharma, Inc). The purpose of this study was to test whether basic laparoscopic skills are improved by this training program.
METHODS
A maximum of 2 urologists are accepted per week into the M-R program. The course consists of the following training modules, of which the trainee chooses one1: ureteroscopy and percutaneous renal access2; laparoscopic renal ablative (radical nephrectomy)3; laparoscopic renal reconstructive (partial nephrectomy and pyeloplasty)4; and robot-assisted prostatectomy. The course includes 2 hours to 3 hours of didactic lectures, daily practice on pelvic trainers and virtual reality simulators, 1 to 2 porcine laboratories per week, and observation of cases in the operating room. The laparoscopic ablative participants perform porcine laparoscopic nephrectomies while the reconstructive participants perform partial nephrectomies and ureteroureterostomies. The robot-assisted prostatectomy module participants are all certified on the da Vinci robot before attending the course. The initial laboratory involves a porcine nephrectomy, cystostomy and closure, urethrovesical anastomosis, and an anastomosis of the porcine uterus to the bladder. The second laboratory involves a radical prostatectomy and lymph node dissection on a human cadaver.
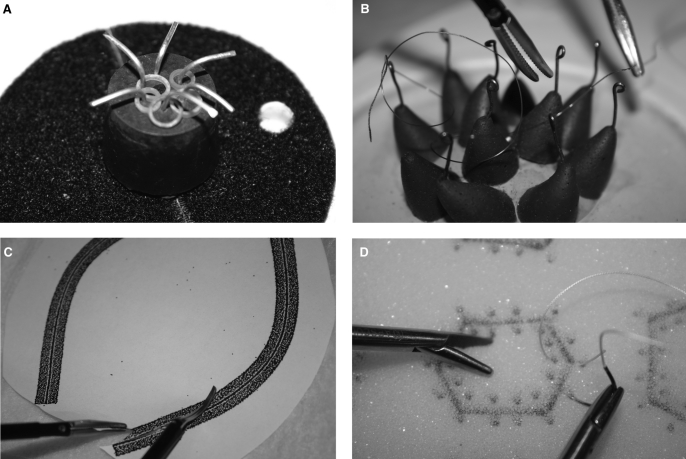
Skills testing (ST) simulating open, laparoscopic, and robot-assisted laparoscopic surgery is performed and evaluated by an experienced observer on training days 1 and 5. The tasks include ring transfer (placing and removing rings from pegs), suture threading (threading a 3–0 Prolene suture through loops), cutting (cutting along designated curved lines), and suturing (continuous running of a suture around a foam hexagon) (Figure 1). Mini-residents undergo ST with open surgical instruments (forceps, needle driver, and scissors) sitting at a table (open ST), with laparoscopic instruments (graspers, needle drivers, and shears) on the pelvic trainer (laparoscopic ST), and with robotic instruments (needle drivers and scissors) on the da Vinci Surgical System (robotic ST). The participants' performance is graded with a validated Objective Structured Assessment of Technical Skill (OSATS) scoring system. The total score is a product of the quantity score (ie, how much of the task is completed in the specified period of time) and the quality score (ie, how accurately the skill task is performed). The data are analyzed using the paired sample t test and analysis of variance at a confidence level of P≤0.05.
Figure 1.
The surgical skills tasks: (A) Participant removes all 6 rings and then places them back on pegs within a 2-minute timeframe. (B) Participant is given 2 minutes to thread a 2–0 Prolene suture through as many of the 11 loops as possible. (C) Participant is given 2 minutes to cut along the inner curved line. (D) Participant is given 3 minutes to run a 4–0 Vicryl suture on an RB-1 as close to the dots as possible.
RESULTS
Between July 2003 and June 2005, 101 urologists from 22 American states and 14 countries participated in the M-R experience at the University of California, Irvine. The representation of surgeons in the 4 training modules included 35 in the laparoscopic ablative module, 17 enrolled in the laparoscopic reconstructive module, 14 for the ureteroscopy and percutaneous renal surgery module, and 35 in the robot-assisted laparoscopic prostatectomy module. Mean participant age was 47 years (range, 31 to 70). Mean time from graduation from urology residency was 15 years (range, 1 to 42). Ninety-eight percent of the participants were male (n=99) and 2% female (n=2).
Ninety-five percent of the participants were right handed (n=95).
The M-R open, laparoscopic, and robotic ST scores for all of the participants on the first and fifth days of the course are shown in Table 1. The maximum possible scores for each of the ST evaluations are 48 for the ring transfer, 44 for the suture threading, 72 for the cutting, 48 for the suturing, and 212 for the cumulative overall score. On both the first and final days of the course, the open ST scores were significantly higher than the robotic ST scores (P<0.0005), which were significantly higher than the laparoscopic ST scores (P<0.0005). This was the case for all of the ST scores, including the overall score. There was no significant difference between the ST scores on the first and final day of the course for any of the open skills tasks. However, the robotic ST scores were significantly higher on the final day compared with those on the first day. This was noted for all the ST scores, including ring transfer (43.4 vs 38.2; P=0.001), suture threading (25.1 vs 21.1; P=0.01), cutting (27.8 vs 22.4; P=0.001), suturing (17.3 vs 14.5; P=0.02), and overall score (114 vs 95; P=0.001). Similarly, laparoscopic ST scores were significantly improved on the final day compared with the first for ring transfer (33.2 vs 28; P=0.001), suture threading (4.2 vs 2.5; P=0.001), cutting (20 vs 13.8; P=0.001), suturing (10 vs 7.8; P=0.01), and overall score (58.2 vs 52.3; P=0.01).
Table 1.
Comparison of Open, Laparoscopic, and Robot-Assisted Total Skills Testing Scores Before and After M-R Training
| Skill Task | Maximum Score | Open Skills | Robot-Assisted Skills | Laparoscopic Skills | P* |
|---|---|---|---|---|---|
| Ring transfer | 48 | ||||
| Day 1 | 46.1 ± 4.7 | 38.2 ± 11.2 | 28 ± 11.7 | <0.0005 | |
| Day 5 | 46.8 ± 3.7 | 43.4 ± 7.6 | 33.2 ± 12.3 | <0.0005 | |
| P value | 0.15 | 0.001 | 0.001 | ||
| Suture threading | 44 | ||||
| Day 1 | 38.1 ± 7.9 | 21.1 ± 11.6 | 2.5 ± 2.8 | <0.0005 | |
| Day 5 | 39.2 ± 6.9 | 25.1 ± 13.1 | 4.2 ± 3.9 | <0.0005 | |
| P value | 0.19 | 0.01 | 0.001 | ||
| Cutting | 72 | ||||
| Day 1 | 67.8 ± 9.4 | 22.4 ± 10 | 13.8 ± 8.9 | <0.0005 | |
| Day 5 | 68.1 ± 8.9 | 27.8 ± 12.8 | 20 ± 11.2 | <0.0005 | |
| P value | 0.76 | 0.001 | 0.001 | ||
| Suturing | 48 | ||||
| Day 1 | 38.2 ±11.1 | 14.5 ± 8.3 | 7.8 ± 6.2 | <0.0005 | |
| Day 5 | 40.3 ± 10 | 17.3 ± 9.2 | 10 ± 5.9 | <0.0005 | |
| P value | 0.10 | 0.02 | 0.01 | ||
| Overall Score | 212 | ||||
| Day 1 | 190.6 ± 25 | 95 ± 30.4 | 52.3 ± 20.3 | <0.0005 | |
| Day 5 | 193.6 ± 19.1 | 114 ± 32 | 58.2 ± 17.5 | <0.0005 | |
| P value | 0.17 | 0.001 | 0.01 |
Open > Robot-Assisted > Laparoscopic.
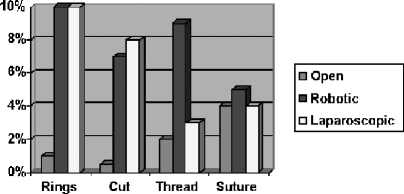
The percentage difference between the mini-resident ST scores on the final day of the course compared with scores on the first day is shown in Figure 2. The percentage difference for the open ST scores, representing the improvement in ST performance, are ring transfer (1%), cutting (0.5%), suture threading (2%), and suturing (4%). The percentage difference for the robotic ST scores are ring transfer (10%), cutting (7%), suture threading (9%), and suturing (5%). The percentage difference for the laparoscopic ST scores are ring transfer (10%), cutting (8%), suture threading (3%), and suturing (4%). It is interesting that the percentage difference of ST improvement in the majority of the ST tasks was essentially the same for the laparoscopic and robotic ST. The more challenging ST tasks, such as suture threading, tend to have less overall score improvement in the laparoscopic ST scores.
Figure 2.
Skill task score improvement following MR. The difference in ST scores on day 5 from ST scores on day 1 is expressed as a percentage of ST scores on day 1.
The participants' performance according to the M-R training module was also examined. Laparoscopic ablative and reconstructive renal module participants demonstrated significant improvement in laparoscopic and robotic ring transfer, suture threading, cutting, and suturing on day 5 compared with day 1 (P<0.05) (Table 2). However, none of this group's open ST changed significantly from day 1 to day 5. In the robot-assisted prostatectomy module participants, significant improvement occurred in the quantity score for the cutting task and the quality score for suturing (P<0.05) (Table 3).
Table 2.
Comparison of Total, Quantity, and Quality Skills Testing Scores Between the Laparoscopic Ablative and Reconstructive Module Participants Before and After Mini-Residency Training
| Skill | Total Score |
Quantity Score |
Quality Score |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | ||||
| Ring transfer | |||||||||
| Open | 46.15 | 46.79 | NS | 12 | 11.98 | NS | 3.85 | 3.9 | NS |
| Laparoscopic | 28.68 | 34.46 | 0.01 | 8.86 | 9.95 | 0.02 | 3.16 | 3.4 | 0.04 |
| Robot-assisted | 32.5 | 43.6 | 0.002 | 10.9 | 11.6 | 0.03 | 3.5 | 3.75 | 0.02 |
| Suture threading | |||||||||
| Open | 39 | 39.13 | NS | 10.67 | 10.6 | NS | 3.63 | 3.67 | NS |
| Laparoscopic | 2.43 | 4.32 | 0.001 | 1.21 | 1.95 | 0.001 | 1.36 | 1.66 | NS |
| Robot-assisted | 19.6 | 25 | 0.01 | 6.02 | 7.16 | 0.01 | 3.09 | 3.27 | NS |
| Cutting | |||||||||
| Open | 68.59 | 68 | NS | 17.76 | 17.88 | NS | 3.86 | 3.8 | NS |
| Laparoscopic | 14.07 | 20.09 | 0.001 | 5.55 | 7.96 | 0.00001 | 2.51 | 2.47 | NS |
| Robot-assisted | 22.3 | 27.5 | 0.02 | 7.05 | 8.17 | NS | 3.12 | 3.29 | NS |
| Suturing | |||||||||
| Open | 38.35 | 40.38 | NS | 10.62 | 11.21 | NS | 3.62 | 3.58 | NS |
| Laparoscopic | 8.14 | 11.14 | 0.009 | 3.21 | 4.02 | 0.02 | 2.39 | 2.77 | 0.009 |
| Robot-assisted | 13.37 | 16.9 | 0.02 | 4.49 | 5.65 | 0.01 | 2.86 | 2.98 | NS |
Table 3.
Comparison of Total, Quantity, and Quality Skills Testing Scores Among the Robot-Assisted Laparoscopic Prostatectomy Module Participants Before and After Mini-Residency Training
| Skill | Total Score |
Quantity Score |
Quality Score |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | ||||
| Ring transfer | |||||||||
| Open | 46.43 | 46.96 | NS | 12 | 12 | NS | 3.87 | 3.91 | NS |
| Laparoscopic | 29 | 31.83 | NS | 9.42 | 9.48 | NS | 3 | 3.25 | NS |
| Robot-assisted | 40.57 | 44.22 | NS | 11.57 | 11.96 | NS | 3.48 | 3.7 | NS |
| Suture threading | |||||||||
| Open | 35 | 39.5 | 0.03 | 10.70 | 10.78 | NS | 3.26 | 3.65 | 0.009 |
| Laparoscopic | 3.04 | 4.42 | NS | 1.46 | 1.83 | NS | 1.54 | 1.92 | NS |
| Robot-assisted | 25.22 | 29.17 | NS | 7.26 | 8.30 | NS | 3.26 | 3.43 | NS |
| Cutting | |||||||||
| Open | 66.26 | 67.7 | NS | 17.74 | 17.61 | NS | 3.74 | 3.83 | NS |
| Laparoscopic | 14.7 | 21 | 0.02 | 5.6 | 7.83 | 0.01 | 2.46 | 2.67 | NS |
| Robot-assisted | 24.19 | 29.29 | NS | 7.52 | 9.3 | 0.04 | 3.1 | 3.1 | NS |
| Suturing | |||||||||
| Open | 36.35 | 40.35 | NS | 10.74 | 10.78 | NS | 3.35 | 3.74 | 0.01 |
| Laparoscopic | 8.88 | 8.21 | NS | 3.63 | 3.38 | NS | 2.17 | 2.29 | NS |
| Robot-assisted | 17.22 | 20 | NS | 6.22 | 6.22 | NS | 2.75 | 3.13 | 0.03 |
Increasing participant age tended to inversely correlate with some of the ST scores. Participants older than 54 years of age scored lower on day 1 of the course for the open ring transfer and suture threading than individuals aged 44 years to 53 years (P=0.03) and <43 years (P=0.03). Moreover, the urologists >54 years of age scored significantly lower on open suture threading on day 5 of the course (P=0.01). For the robotic ST scores, the >54-year-old group scored lower on suture threading on day 1 (P=0.004) and day 5 (P=0.017) as well as on suturing on day 5 (P=0.006). For robotic ring transfer ST scores, surgeons <43 years scored significantly better than the older participants (P=0.0004). The rest of the open and robotic ST scores, and none of the laparoscopic ST scores were significantly different between the various age groups (P>0.05) (Table 4).
Table 4.
Effect of Participant Age on Skills Testing Scores
| Skill | <43 Years | 44-53 Years | ≥54 Years | |
|---|---|---|---|---|
| Open | ||||
| Ring transfer (day 1) | 45.6 ± 5.1 | 48 | 44.5 ± 5.9 | <43 = 44-53 ≥ 54 (0.03) |
| Suture threading (day 1) | 38.9 ± 6.8 | 39.6 ± 7 | 34.17 ± 10.2 | <43 = 44-53 ≥ 54 (0.02) |
| Suture threading (day 5) | 41.2 ± 5.3 | 39.6 ± 6.3 | 35.88 ± 8.4 | <43 = 44-53 ≥ 54 (0.01) |
| Robot-assisted | ||||
| Ring transfer (day 5) | 46.3 ± 4.2 | 42.1 ± 7.6 | 39.8 ± 9.9 | <43 > 44-53 ≥54 (0.004) |
| Suture threading (day 1) | 22.9 ± 10.2 | 21.2 ± 13.2 | 12.8 ± 9.3 | <43 = 44-53 ≥54 (0.004) |
| Suture threading (day 5) | 28.2 ± 12.7 | 26.4 ± 10.8 | 18.1 ± 13.4 | <43 = 44-53 ≥54 (0.017) |
| Suturing (day 5) | 20.6 ± 8.7 | 16.1 ± 9.8 | 12.9 ± 6.8 | <43 = 44-53 ≥54 (0.006) |
Skill task scores of participants who graduated from urology residency less than 10 years ago were compared with those who graduated greater than 10 years ago (Table 5). The more recent graduates had significantly higher scores for robotic suture threading on day 1 (P=0.01), open suture threading on day 5 (P=0.03), and laparoscopic cutting on day 5 (P=0.01). No other ST scores differed significantly between the 2 groups.
Table 5.
Effect of Time Since Graduation From Urology Residency on Skills Testing Scores
| Skill | 0-10 Years | >10 Years | P |
|---|---|---|---|
| Open skills: suture threading (day 5) | 41.2 ± 5.3 | 37.9 ± 7.6 | 0.03 |
| Laparoscopic skills: cutting (day 5) | 23.5 ± 13 | 17.5 ± 8.6 | 0.01 |
| Robot-assisted skills: suture threading (day 1) | 23.3 ± 9.4 | 16.6 ± 11.5 | 0.01 |
DISCUSSION
The learning of laparoscopic skills presents unique challenges not seen in open surgery, such as a small working space, limited instrument movement, decreased tactile sensation, and counterintuitive manipulation of instruments in a 2-dimensional visual field. To help facilitate the development of laparoscopic skills in postgraduate urologists, the University of California, Irvine has established a 5-day M-R program.
The M-R curriculum was designed to facilitate the acquisition of laparoscopic skills by postgraduate urologists. Faculty members in the Department of Urology give didactic lectures, and hold question and answer sessions with the attendees, on subjects that pertain to the laparoscopic learning curve. These subjects include laparoscopic techniques, such as suturing and knot-tying, and management of complications. Mini-residents practice on a pelvic trainer or a computer-based laparoscopic surgery simulator for 30 minutes twice a day. They initially perform suturing and knot-tying on foam pads with hexagonal markings (Figure 1), and also skills train on virtual reality simulators. Once proficient suturing is demonstrated on the rudimentary models, the trainees then practice on silicone models that simulate laparoscopic and robot-assisted closure of the collecting system, urethrovesical anastamosis, and pyeloplasty. Finally, near the end of the 5 days, the animal laboratories allow the mini-residents to further apply skills they have learned to laparoscopic or robot-assisted partial nephrectomy, pyeloplasty, and urethrovesical anastamosis, including complex suturing and knot-tying. Practice occurs in a 1:1 or 1:2 instructor to M-R ratio. The fellows in minimally-invasive surgery education and endourology and laparoscopy are the laboratory instructors for the M-R program. Throughout the 5-day M-R, cognitive and technical learning is enhanced by observation of operative cases. Acquisition of laparoscopic skills is assessed by testing mini-residents at the beginning and at the end of the M-R. Robotic and laparoscopic ST scores on ring transfer, suture threading, cutting and suturing improved significantly. This improvement may be a consequence of the focused and intensive M-R curriculum.
Interestingly, the participants enrolled in the robotic module demonstrated no significant improvement in their preand postrobotic skill task scores except in the cutting skill task category. This may reflect the ease by which the surgeons acquire these basic robotic-assisted surgical skills, making them very good performers almost immediately. Alternatively, there may be a much longer learning curve for these skills, and the M-R did not permit sufficient training time to realize improvement. The former seems more likely given the reported ease of surgeons acquiring robotic-assisted surgical procedures versus the laparoscopic counterpart.4 Conversely, the laparoscopic training modules allowed improvement in the pre- and postlaparoscopic skill task scores, suggesting in this more challenging surgical interface the learning curve effect is still being completed even at the conclusion of the educational program. It is anticipated that most in these training groups will require additional skills practice after their initial learning in the training program.
The purpose of this study was to assess whether those taking the course could develop basic laparoscopic and robotic skills, such as general coordination of instruments (ie, ring transfer and suture threading), and surgically oriented skills, such as cutting, and suturing. The results show that laparoscopic and robotic ST scores significantly improved over the 5-day course, while open ST scores did not. It would be expected that open ST scores would not improve following the M-R course, because these types of skills are not formally addressed during the course. The observation that robotic ST scores are significantly higher than the laparoscopic ST scores at both the beginning and the end of the course reflects the greater degree of complexity associated with performing pure laparoscopic skills. As other investigators have demonstrated, basic robotic skills are more easily acquired than are laparoscopic skills.4 The robot facilitates the skill performance by providing an intuitive working format with more precise instrument movement, 3-dimensional visualization, and increased surgeon comfort at the master console. The counterintuitive, 2-dimensional working environment, long instruments fulcrumed at the abdominal wall, and magnification of the surgeon's natural tremor all compound to make laparoscopy a challenging surgical technique.
Some correlation appears to exist between ST scores and age, particularly the robot-assisted ST scores. Urologists older than 54 years of age had significantly poorer scores on suture threading on both days 1 and 5 and ring transfer on day 1. Although robot-assisted suturing was no different between the groups on day 1, urologists older than 54 years had significantly lower scores on day 5 for ring transfer and suture threading. These data suggest that surgeons older than 54 years of age may have poorer fine motor coordination when using the robot and may have more difficulty learning robot-assisted suturing. These surgeons may require a longer training program to reach the same proficiency level as their younger counterparts, although this study did not assess that. Conversely, age does not appear to influence laparoscopic ST scores, including suturing. This may reflect the fact that all surgeons require more training and practice time learning laparoscopic skills than was provided during this 5-day education program. Time since graduation appears to have a less significant impact on ST scores than does age. Only robot suture threading (day 1), open suture threading (day 5), and laparoscopic cutting (day 5) varied significantly with time since graduation.
The M-R program at the University of California, Irvine improves basic laparoscopic and robotic skills, such as fine instrument coordination, cutting, and suturing. The degree of improvement is up to 10% from baseline. The question that remains is whether this degree of improvement translates into improved performance of laparoscopic surgery in the clinical realm. One of the first groups to study the impact of laparoscopy courses on urologists' practice patterns was the Department of Urology at the University of Iowa.1,2 These courses were held over a 2-day period and focused on teaching laparoscopic varicocelectomy and pelvic lymph node dissection. They consisted of 8 hours of didactic lectures, 4.5 hours on pelvic trainers, 4.5 hours on animal models, and observation of 2 live surgery video broadcasts. A questionnaire assessing laparoscopic practice patterns was sent at 1 and 5 years after course completion. Of the 322 urologists that participated in these courses, 166 (51%) responded. The initial results were encouraging with 84% of participants performing some form of laparoscopic surgery at 1-year follow-up.1 However, at 5-year follow-up, only 54% of course participants were performing laparoscopic surgery. The indicated reasons for this decrease in performing laparoscopic procedures included lack of indications for laparoscopic surgery, increased cost, decreased patient interest, higher complication rates, decreased institutional support, and increased operative time.2
A questionnaire on laparoscopic practice patterns was sent to the initial 32 participants in the laparoscopic ablative or reconstructive renal surgery M-R, 1 to 15 months (mean 8 months) after completion of the course.5 The response rate to the questionnaire was 100%. Most (72%) of the participants had prior laparoscopic training during their urology residency. Twenty-six participants (81%) were performing some form of laparoscopic surgery after their M-R. More of the participants were performing laparoscopic radical nephrectomy, nephroureterectomy, and pyeloplasty. Similarly, a questionnaire was sent to the initial 21 participants in the robot-assisted laparoscopic prostatectomy M-R 1 to 14 months (mean, 7.2) later.6 The response rate to this questionnaire was also 100%. Most (80%) of the participants had prior laparoscopic training in their urology residency, and 25% were performing robot-assisted laparoscopic prostatectomy before their M-R. After their M-R, 95% of the participants were performing robot-assisted laparoscopic prostatectomy. These data support the use of a focused, intensive 5-day M-R in assisting postgraduate urologists with the acquisition of laparoscopic and robot-assisted laparoscopic skills that are applicable to their clinical practice. Additional follow-up will reveal the durability of such skills acquisition and elucidate those factors responsible for skills maintenance.
Another method for postgraduate urologists to train in laparoscopic skills is through a mentor-trainee relationship. Shalhav et al7 developed a “mini-fellowship” model that consisted of 3 phases: 1) a 2- to 3-day hands-on course on pelvic trainers and animal laboratories; 2) observing the clinical mentor perform 6 or more major renal laparoscopic procedures; and 3) the trainee performing 6 or more major renal procedures under mentor guidance on the trainee's patients at the mentor's or trainee's hospital. In the initial report, 2 community urologists underwent this course in 2000. One trainee performed 30 laparoscopic procedures, including 17 radical nephrectomies, 4 simple nephrectomies, 4 nephroureterectomies, 4 renal cyst ablations, and 1 renal biopsy within the first 8 months after completing the training program. The second trainee performed 10 laparoscopic procedures within the first 3 months after training. Subsequent update of this course included 5 community urologists (personal communication with Dr. A. Shalhav). From this experience, 3 trainees have gone on to perform numerous laparoscopic surgeries following training. Two additional trainees who practice in a smaller group setting have had limited performance of laparoscopic procedures to date. This program was extremely time intensive for both the trainee and the mentor and was a significant financial burden to the trainee (ie, the mentor would bill as the primary surgeon). However, it enabled 3 of 5 (60%) trainees to gradually become more skilled and confident in laparoscopic surgery. The M-R program at the University of California, Irvine has attempted to foster the mentoring concept while providing a potential proctoring opportunity. It is interesting that only 14 of the 101 (14%) M-R registrants have participated in the proctoring/preceptoring opportunity of this program. It is unclear why so few M-R participants have taken advantage of this unique aspect of the program.
Similarly, Rane and colleagues8 proctored 6 postgraduate urologists and recommend that each trainee perform 12 to 15 cases under the supervision of the expert before independently performing laparoscopic procedures. These educators recommended that the proctors have a minimum experience of 50 laparoscopic cases. Thus far, 5 of the 6 trainees have successfully completed the program within 4 months of commencing the training.8 The overall 85% success or “take” rate of the University of California, Irvine M-R program compares favorably to the 83% take rate of this time-intensive laparoscopic proctoring training program.5,6 Of course, further long-term follow-up of both courses is necessary to determine the durability of these learned skills.
CONCLUSION
Laparoscopic and robotic skills are difficult to acquire, especially for those urologists who were not exposed to the technique during residency training. It appears that the 5-day intensive M-R course improves both laparoscopic and robotic basic skills. Further long-term assessment will help to determine whether the basic skills learned in the M-R course translate into the ability to perform advanced laparoscopic procedures safely in clinical practice. The M-R represents a new paradigm in postgraduate surgical education.
References:
- 1.See WA, Fisher RJ, Winfield HN, et al. Laparoscopic surgical training: effectiveness and impact on urological surgical practice patterns. J Urol. 1993;149:1054–1057 [DOI] [PubMed] [Google Scholar]
- 2.Colegrove PM, Winfield HN, Donovan JF, See WA. Laparoscopic practice patterns among North American urologists 5 years after formal training. J Urol. 1999;161:881–886 [PubMed] [Google Scholar]
- 3.Cadeddu JA, Wolfe JS, Nakada S, et al. Complications of laparoscopic procedures after concentrated training in urological laparoscopy. J Urol. 2001;166:2109–2111 [PubMed] [Google Scholar]
- 4.Kaul S, Shah NL, Menon M. Learning curve using robotic surgery. Curr Urol Rep. 7(2):125–129, 2006. Review [DOI] [PubMed] [Google Scholar]
- 5.Corica FA, Boker JR, Chou DS, et al. Short-term impact of a laparoscopic “mini-residency” experience on postgraduate urologists' practice patterns. J Am Coll Surg. 2006;203(5):692–698 [DOI] [PubMed] [Google Scholar]
- 6.McDougall EM, Corica FA, Chou DS, et al. Short-term impact of a robot-assisted laparoscopic prostatectomy ‘mini-residency’ experience on postgraduate urologists' practice patterns. Int J Med Robotics Comput Assist Surg. 2006;2:70–74 [DOI] [PubMed] [Google Scholar]
- 7.Shalhav AL, Dabagia MD, Wagner TT, Koch MO, Lingeman JE. Training postgraduate urologists in laparoscopic surgery: the current challenge. J Urol. 2002;167:2135–2137 [PubMed] [Google Scholar]
- 8.Rane A, Dasgupta P. Mentorship in laparoscopic surgery. J Endourol. 2004;18(suppl 1):A47 Abstract MP6/8 [Google Scholar]