Abstract
Objectives:
Complications of polypropylene pubovaginal tension-free tape slings (TVT, SPARC, and others), such as erosion into the bladder or chronic pain attributed to the mesh sling are rare events; however, when they occur, it may necessitate removal of the sling. To date, removal through a laparotomy incision or by operative cystoscopy has been the most common approach. We present 5 cases of a laparoscopic approach for removal of polypropylene pubovaginal tension-free tape slings.
Methods:
We report 5 cases of laparoscopic removal of TVT mesh. Three were removed for mesh erosion into the bladder, and 2 were removed secondary to the patients having persistent pain and discomfort attributed to the sling. An intraperitoneal approach was used to enter the retropubic space to remove the sling. Dissection was completed with a Harmonic scalpel blade as well as blunt dissection to identify the mesh sling retropubically. Average operating time was 104 minutes. Average blood loss was 70 mL. Average hospital stay was <23 hours. Postoperative courses were uneventful; however, 4 of the 5 patients continue to have urgency and frequency symptoms following sling removal.
Conclusion:
These cases illustrate the use of laparoscopy in the removal of polypropylene pubovaginal tension-free tape slings for bladder erosion or persistent pain, or both, attributed to the sling. Erosion and pain are known complications of polypropylene pubovaginal slings and may cause significant morbidity like persistent detrusor instability or urge incontinence, or both. Patients must be informed of these risks and possible complications before making their decision to undergo surgery.
Keywords: Sling complication, Mesh, Tension-free vaginal tape, Complications, Laparoscopic, Bladder erosion
INTRODUCTION
The tension-free vaginal tape (TVT, Gynecare, Sommerville, NJ) was introduced in 1995 by Ulmsten and Petros for female stress urinary incontinence (SUI) and has quickly gained worldwide acceptance due to good functional results and low complication rates. Other pubovaginal polypropylene sling systems have been developed in parallel with the TVT with similar efficacy, such as the SPARC (American Medical Systems, Minnetonka, MN) and Urotek (Bard Urology, Covington, GA) slings. Erosion of sling materials into the genitourinary tract is an uncommon but known complication after pubovaginal sling placement with reported incidences ranging from 0.3% to 14%.1 Widespread use is resulting in increasing numbers of complications creating certain circumstances like erosion or pain that necessitate removal of the mesh either partially or totally from the body. Mesh that has eroded vaginally can easily be removed with the patient under local anesthesia through a small suburethral incision.2 Mesh erosion into the urethra requires a vaginal approach with removal of the mesh and repair of the urethra. Mesh erosion into the bladder necessitates removal and has been described using laparotomy,3 or by operative cystoscopy.4,5 Laparoscopy has been shown to be a safe mode of access into the space of Retzius, even when previous surgery has occurred in the space6 and has the advantages of improved visualization with magnification of the operative field, decreased blood loss, and a low rate of lower urinary tract injuries.7 Other advantages over laparotomy include less postoperative pain, shorter hospital stays, and faster recovery times. Despite these advantages, its use in the removal of tension-free mesh tape slings from the retropubic space or bladder, or both, has not been described. We report on 5 patients from whom polypropylene mesh slings were removed successfully via a laparoscopic approach from the space of Retzius and from the bladder if erosion had occurred.
METHODS
Five patients presented to our center with complications from pubovaginal tension-free polypropylene mesh tape slings that had been placed at other centers for SUI. Complications necessitated removal of a portion of or all of the sling from the retropubic space because of either mesh erosion into the bladder or persistent pain attributed to the sling. Three patients (Table 1) had their slings removed because of erosion into the bladder. They presented between 4 and 13 months after sling placement with persistent frequency, urgency, dysuria, hematuria, and urge incontinence. One of the 3 also had recurrent urinary tract infections. Erosion of mesh into the bladder was diagnosed by office cystoscopy in all 3 cases. All 3 erosions were found to be on the patients’ right side at approximately the 8 o’clock to 11 o’clock position in the bladder.
Table 1.
Patients With Bladder Erosion
| Patient | Age | Months From Sling Placement | Reason for Removal | Op Time | Estimate of Blood Loss | Surgical Complications | Length of Stay | Postoperative Diagnosis |
|---|---|---|---|---|---|---|---|---|
| 1 | 33 | 13 | Mesh in bladder | 1:21 | 100 mL | None | <23 hrs | Urge and Stress leakage |
| 2 | 72 | 4 | Mesh in bladder | 1:03 | 25 mL | None | <23 | hrs Urge Leakage IC (+ k test) |
| 3 | 64 | 11 | Mesh in bladder | 2:37 | 50 mL | None | <23 hrs | Doing well at 12 week follow up |
Two patients (Table 2) had their slings removed because of persistent vaginal/pelvic pain following placement of their slings that was attributed to the sling itself. These patients were carefully counseled preoperatively that removal did not guarantee cessation of pain and that incontinence may return or persist. Both patients had both vaginal and retropubic pain since placement of their mesh sling that they attributed to the sling itself. They also complained of dysuria, and one had persistent SUI (patient #5). On examination, they both had reproduction of their pain with direct palpation of the sling vaginally on either side of the urethra and bladder neck that radiated retropubically. One patient (#4) previously had the sling released (cut) in the midline under the urethra secondary to persistent urinary obstruction following placement and then subsequently developed mesh erosion vaginally that could be felt by the patient and her husband. She had persistent distal vaginal pain under the urethra that radiated retropubically as well. She also had a pulling sensation retropubically that would turn into pain when she would raise her right leg. The patient had a hysterectomy at the time of her sling placement, and on examination also had persistent pain at the vaginal vault. She understood that this pain was most likely not secondary to her sling and that we would evaluate her vaginal cuff and apex at the time of laparoscopic removal of the sling.
Table 2.
Patients With Pain Only
| Pt | Age | Months From Sling Placement | Reason for Removal | Operative Time | Blood Loss (mL) | Intraoperative Complication | Length of Stay (Hours) | Postoperative Diagnosis |
|---|---|---|---|---|---|---|---|---|
| 4 | 30 | 11 | Pelvic pain | 1:45 | 75 | None | <23 | Supra-Pubic pain improved |
| Mesh erosion into vagina | Leg pain improved | |||||||
| 5 | 66 | 36 | Pelvic pain | 1:54 | 100 | None | <23 | Pain improved |
| SUI | Urge Leakage IC |
Surgical Technique
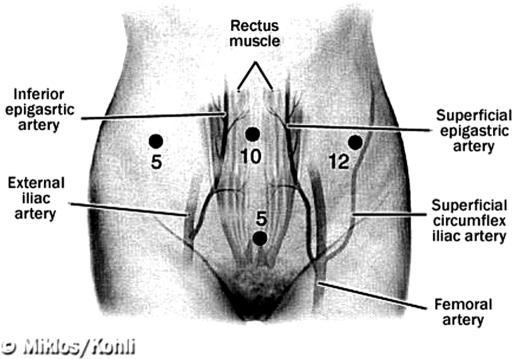
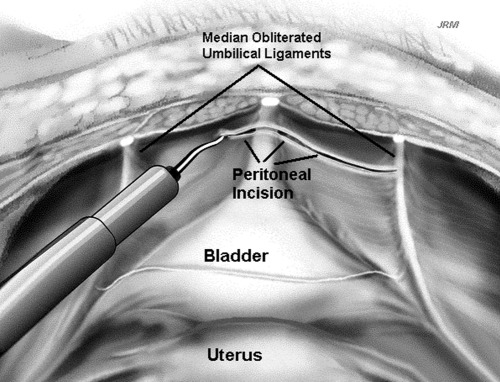
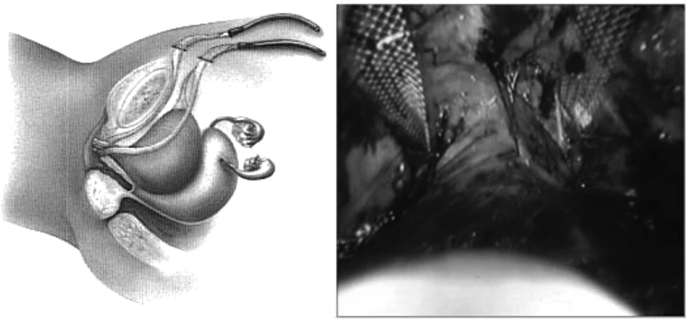
A laparoscopic approach was utilized in all patients to remove their polypropylene mesh sling from the retropubic space, bladder, or both. Our technique consists of using open laparoscopy to enter the peritoneal cavity through the umbilicus and then placing 3 ancillary ports under direct vision (Figure 1). A 10-mm port is placed in the left paramedian region for suturing, and 5-mm ports are placed suprapubically and in the right paramedian region. After the pneumoperitoneum is created, and any adhesions taken down, the bladder is filled in a retrograde manner with 200 mL to 300 mL of saline, allowing for identification of the superior border of the bladder edge. Entrance into the space of Retzius is accomplished by a transperitoneal approach (Figure 2) by using a Harmonic scalpel, which is the identical approach we use when completing laparoscopic Burch procedures or paravaginal repairs, or both together.8 The incision is made approximately 3 cm above the bladder reflection, beginning along the medial border of the right obliterated umbilical ligament. Identification of loose areolar tissue at the point of incision confirms the proper place of dissection. After the space of Retzius is entered and the pubic ramus visualized, the bladder is drained to prevent injury during dissection. Separation of the loose areolar and fatty layers using blunt dissection develops the retropubic space, and dissection is continued until the retropubic anatomy is clearly visualized. When the retropubic space has been invaded with a previous procedure, such as polypropylene mesh, a large amount of scar tissue can be encountered and extreme care in the dissection is necessary. Additionally, the surgeon must be aware of the location of the obturator/neurovascular bundle at all times, as injury to the vessels can be a life threatening injury. Identification of the sling mesh is most commonly made where it touches the pubic rami approximately 2 cm to 3 cm lateral from midline (Figure 3). Once identified, the mesh can be grasped and excised from the anterior abdominal wall and then peeled free of the pubic rami periosteum. Dissection is then continued down along the mesh toward the bladder and pubocervical fascia. Extensive scarring is often encountered, and the mesh will need to be cut out with the scared tissue. If the mesh is eroded into the bladder, the dissection is continued down to where the mesh goes into the bladder, the bladder opened, and the mesh removed from the bladder with clean margins of bladder excised with the mesh. The resulting cystotomy will then have clean, mesh-free margins, and repair of the cystotomy is accomplished laparoscopically by using a double-layer closure of interrupted 3.0 Vicryl suture on an SH needle. Cystoscopy is completed before mesh removal in the bladder to ensure the excision will not compromise the ureters. If any concerns exist with the proximity of the ureter to the mesh erosion, a ureteral stent is placed. Dual cystoscopy and laparoscopy are used throughout the excision and repair to check the proximity of the cystotomy to the ureteral orifice and uretero-vesical junction before and after excision and closure. Cytoscopy also confirms a watertight closure by retrograde filling of the bladder and observing laparoscopically to check for leakage. Cystoscopy is then done again at the end of the case to visualize ureteral reflux of indigo carmine dye given intravenously to ensure ureteral patency and bladder integrity. If the sling was removed for pain and had not eroded the bladder, the dissection is continued down to and through the pubocervical fascia on both sides. An incision is then made suburethrally, and the remaining mesh below the urethra is identified, cut in the midline, and then freed up to the pubocervical fascia dissection done from above, allowing removal of the entire vaginal and retropubic portion of the mesh sling from above or below. Cystoscopy is then completed following removal of the mesh to ensure that bladder injury did not occur.
Figure 1.
Laparoscopic port placement used for removing pubovaginal slings.
Figure 2.
Incision used to enter the space of retzius created with the harmonic scalpel.
Figure 3.
Location of pubovaginal sling mesh in the space of retzius and laparoscopic appearance of TVT sling retropubically at time of initial placement.
RESULTS
All 5 patients had their mesh successfully removed either from the retropubic space or bladder, or both, with a laparoscopic approach. In the patients in whom the tape had eroded into the bladder, only the side of the mesh that had eroded into the bladder was removed and the resulting cystotomy was closed laparoscopically as well. In the patients who suffered from retropubic pain, both sides of the mesh were removed from the abdominal wall to the pubocervical fascia laparoscopically and then the suburethral portions removed through a small vaginal incision.
All 3 patients with mesh erosion into the bladder had the mesh removed via laparoscopy without any complications. A summary of the operative data is seen in Table 1. All 3 patients had suprapubic catheters placed for drainage for 2 weeks following repair. They were all discharged from the hospital in less than 24 hours, and no postoperative complications occurred. Two of the women (patients 1 and 2, Table 1) continue to have stress and urge incontinence 6 months after removal, but are being controlled with anticholinergic agents. Follow-up cystoscopy has shown the bladders to be well healed without any mesh exposure/erosion present. Their dysuria has resolved. The third patient had slight urge symptoms at 12 weeks postoperatively; however, she stated that her symptoms are 90% better than they were preoperatively. She no longer has dysuria or urge leakage and generally feels better than she has since the sling had been originally placed.
The 2 patients who presented with pain attributed to their sling had successful removal of their slings retropubically via a laparoscopic approach. No intraoperative complications (Table 2) occurred, and both were discharged from the hospital in less than 24 hours after their surgery. They had uneventful postoperative courses as well. Patient number 4 had a Burch urethropexy done at the time of mesh erosion for persistent stress incontinence; however, at 14 months she still suffers from stress and urge incontinence and is being treated for interstitial cystitis. Her vaginal pain however is improved to the level it was before sling placement.
At the time of sling removal, patient number 5 was noted to have stage 3 endometriosis in the pelvis with pelvic adhesions, implants throughout the sidewalls and on each ovary. At 12 weeks postoperation following retropubic and vaginal removal of her sling, she had resolution of her distal vaginal and suprapubic pain on examination, as well as resolution of pain when she raised her right leg. She continued to have pain at the vaginal cuff on examination as well as some right, lower, quadrant pain that we believe to be due to her endometriosis. She has been referred to a specialist and is currently undergoing treatment of her pelvic endometriosis.
DISCUSSION
Because of the close proximity, bladder injury at the time of pubovaginal sling placement is reported to occur in up to 5.8% of cases.9 Although less common, later erosion of mesh into the bladder has also been reported.3,4 It is possible that some of these erosions may have been undetected primary perforations; however, another mechanism is possible, namely pressure necrosis and slow penetration of the bladder wall, particularly in slings that pass very close to the bladder or even through the bladder wall, yet not penetrating the bladder mucosa, making them undetectable at the time of surgery. Whatever the mechanism, erosion necessitates removal of the eroded portion of mesh. A foreign body in the bladder, such as occurs with mesh erosion, can cause hematuria, stone formation, recurrent urinary tract infection, dysuria and/or persistent urgency, frequency or urge incontinence. Authors have described removal of whole tapes from the space of Retzius via a retropubic approach through laparotomy.3,10 Others have removed the intravesicular portions of mesh with operative cystoscopy.4,5,11 Tsivian12 describes resection through a suprapubic incision after a failed attempt at removal with operative cystoscopy. Hodroff et al11 describe successful cystoscopic removal of bladder mesh erosion using a Holmium laser. To our knowledge, we describe the first cases of a laparoscopic approach for removal of tension-free polypropylene mesh tape slings from the retropubic space for pain or erosion into the bladder, or both. This method is minimally invasive, safe, and, unlike cystoscopic removal, it allows the entire portion of the eroded mesh sling to be removed through the full thickness of the bladder wall with clean margins to close. We feel that cystoscopic removal with simple excision or laser is limited in this regard and has a high potential for recurrence at the edges of the mesh that remain in the bladder wall and are likely to re-erode through the bladder mucosa during or after healing occurs.
Removal of a sling for pain alone did not improve all symptoms of pain in our patients. Pelvic pain is typically multifocal, and strong consideration of this should be given and counseling provided to the patient, before removal of the sling. However, in both patients, their pain in the suburethral and retropubic region did not exist before sling placement, and they attributed the pain to the mesh sling and wished for it to be removed. Both had undergone months of conservative therapy before surgical intervention and they clearly understood there was no guarantee that their pain would improve following removal. After removal, their suburethral and retropubic pain seemed to improve; however, they both continued to have pelvic pain that required further treatment. This is an important issue to consider not only in counseling patients before initial placement, but also before attempts at removal.
Another issue to consider is the effect on continence following removal of a part of the sling or the whole sling. Theoretically, if the sling is totally removed, incontinence should be expected to return or worsen. Partial removal of sling material from the bladder or suburethrally may preserve continence.2,10,12 Clemens et al13 however describe a 58% incontinence rate after sling removal, and Kobashi et al2 found a 74% mild to severe stress incontinence rate after removal. Removal of only the bladder portion of the mesh with a cystoscopic approach may preserve continence1; however, patients may have increased risk of recurrent erosion at the cut edges of the mesh into the bladder. We attempted laparoscopic Burch in one patient at the same time of removal of her sling for pain as she had persistent stress incontinence even with the sling in place; however, this was not successful and she still had SUI postoperatively as well. Of the 3 patients that had partial removal of their slings for mesh erosion, one has recurrent stress incontinence symptoms. All patients however continue to have urgency/frequency symptoms following removal, requiring treatment that can be difficult to control.
CONCLUSION
Mesh erosion into the bladder is a rare but known complication of pubovaginal tension-free polypropylene mesh slings that requires removal of the portion of the sling that has eroded into the bladder. Additional reasons, such as persistent pain attributed to the sling itself, may necessitate removal as well. Total or partial removal of polypropylene pubovaginal type slings can be done successfully via a laparoscopic approach by experienced surgeons, offering a less invasive approach than suprapubic removal with laparotomy. We feel this is an ideal approach not only for removal of the retropubic portion of the sling, but also for mesh erosion into the bladder as it ensures complete removal of the mesh from the bladder and minimizes the chances of recurrent erosion of the cut edges of the mesh that can occur with the cystoscopic approach. In the current series, 5/5 patients had successful removal of the retropubic or intravesical portion of the TVT sling, or both, with a laparoscopic approach. No intraoperative complications occurred, and all patients had minimal hospital stays (<24 hours) with very rapid recovery. Although this is a small series, we believe that it demonstrates a viable approach when removal is necessary. Further study is warranted in this and other minimally invasive alternatives to laparotomy; however, in the future, we may see less of this type of complication with the advent of the transobturator approach to place suburethral slings, which avoids the retropubic space.
References:
- 1. Boubili V, Ciofu C, Traxer O, Sebe P, Haab F. Complications of urethral sling procedures. Curr Opin Obstet Gynecol. 2002; 14 ( 5): 515– 520 [DOI] [PubMed] [Google Scholar]
- 2. Kobashi K, Dmochowski R, Mee SL, et al. Erosion of woven polyester pubovaginal sling. J Urol. 1999; 162 ( 1): 2070– 2072 [DOI] [PubMed] [Google Scholar]
- 3. Volkmer BG, Nesslauer T, Rinnab L, Schradin T, Hautmann RE, Gottfried HW. Surgical intervention for complications of the tension-free vaginal tape procedure, J Urol. 2003; 169 ( 2): 570– 574 [DOI] [PubMed] [Google Scholar]
- 4. Levin I, Groutz A, Gold R, Pauzner D, Lessing JB, Gordon D. Surgical complications and medium-term outcome results of tension-free vaginal tape: a prospective study of 313 consecutive patients. Neurourol Urodyn. 2004; 23 ( 1): 7– 9 [DOI] [PubMed] [Google Scholar]
- 5. Irer B, Aslan G, Cimen S, Bozkurt O, Celebi I. Development of vesicle calculi following tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16: 245– 246 [DOI] [PubMed] [Google Scholar]
- 6. Moore RD, Speights S, Miklos JR. Laparoscopic Burch colposuspension for treatment of recurrent stress urinary incontinence. J Am Assoc Gyn Laparosc. 2001; 8 ( 3): 389– 392 [DOI] [PubMed] [Google Scholar]
- 7. Speights S, Moore RD, Miklos JR. Frequency of lower urinary tract injury at laparoscopic Burch and paravaginal repair. J Am Assoc Gynecol Laparosc. 2000; 7: 515– 518 [DOI] [PubMed] [Google Scholar]
- 8. Miklos JR, Moore RD, Kohli N. Laparoscopic surgery for pelvic support defects. Curr Opinion Obstet Gynecol. 2002; 14: 387– 395 [DOI] [PubMed] [Google Scholar]
- 9. Abouassaly R, Steinberg ML, Lemieux M, et al. Complications of tension-free vaginal tape surgery: a multi-institutional review. BJU Int. 2004; 94 ( 1): 110– 113 [DOI] [PubMed] [Google Scholar]
- 10. Tsui KP, Ng SC, Tee YT, Yeh GP, Chen GD. Complications of synthetic graft materials used in suburethral sling procedures. Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16: 165– 167 Epub 2004 Oct 19 [DOI] [PubMed] [Google Scholar]
- 11. Hodroff M, Portis A, Siegel SW. Endoscopic removal to intravesical polypropylene sling with the holmium laser. J Urol. 2004; 172: 1361– 1362 [DOI] [PubMed] [Google Scholar]
- 12. Tsivian A, Kessler O, Mogutin B, et al. Tape related complications of the tension-free vaginal tape procedure. J Urol. 2004; 171: 762– 764 [DOI] [PubMed] [Google Scholar]
- 13. Clemens JQ, DeLancey JO, Faerber GJ, Westney OL, Mcguire EJ. Urinary tract erosions after synthetic pubovaginal slings: Diagnosis and management strategy. Urology. 2001; 56 ( 4): 589– 594 [DOI] [PubMed] [Google Scholar]