Abstract
Background:
Since first reported in 1996, endoscopic minimally invasive surgery of the cervical region has been shown to be safe and effective in the treatment of benign thyroid and parathyroid disease. The endoscopic transaxillary technique uses a remote lateral approach to the thyroid gland. Because of the perceived difficulty in accessing the contralateral anatomy of the thyroid gland, this technique has typically been reserved for patients with unilateral disease.
Objectives:
The present study examines the safety and feasibility of the transaxillary technique in dissecting and assessment of both thyroid lobes in performing near total thyroidectomy.
Methods:
Prior to this study we successfully performed endoscopic transaxillary thyroid lobectomy in 32 patients between August 2003 and August 2005. Technical feasibility in performing total thyroidectomy using this approach was accomplished first utilizing a porcine model followed by three human cadaver models prior to proceeding to human surgery. After IRB approval three female patients with histories of enlarging multinodular goiter were selected to undergo endoscopic near total thyroidectomy.
Results:
The average operative time for all models was 142 minutes (range 57–327 min). The three patients in this study had clinically enlarging multinodular goiters with an average size of 4 cm. The contralateral recurrent laryngeal nerve and parathyroid glands were identified in all cases. There was no post-operative bleeding, hoarseness or subcutaneous emphysema.
Conclusion:
Endoscopic transaxillary near total thyroidectomy is feasible and can be performed safely in human patients with bilateral thyroid disease.
Keywords: endoscopic, thyroidectomy, total, transaxillary
INTRODUCTION
Endoscopic thyroidectomy has joined the ranks of surgical procedures being performed via a minimally invasive approach. Since its first reported performance in 1996, cervical minimally invasive procedures have been deemed safe and effective for treating benign thyroid and parathyroid disease.1 Endoscopic approach to the thyroid and parathyroid gland may be performed through a direct or indirect (remote) technique. The direct approach places the access ports within the cervical region and is considered the least invasive.2–5 The indirect approach provides access to the neck through a remote site from the target area.6–11 Though this approach provides superior cosmesis, it is the most invasive, requiring a relatively large working space to access the thyroid region.
Of the indirect procedures, the transaxillary technique approaches the gland from a remote lateral site to completely hide the surgical scars. Because this is a lateral approach, its primary application has historically been treatment of unilateral thyroid and parathyroid disease.9 In this study, we examined the safety and feasibility of the transaxillary technique to dissect and remove both sides of the thyroid gland in performing a total or near total thyroidectomy for benign thyroid disease.
METHODS
From August 2003 to August 2005, we successfully performed endoscopic transaxillary thyroid and parathyroidectomy surgery for unilateral and parathyroid disease in 41 patients. In this study, we set out to explore the feasibility of an endoscopic transaxillary approach in performing near total to total thyroidectomy for benign thyroid disease. Before performing this technique in humans, technical and safety data confirming its feasibility were obtained in animal and human cadaver models. The challenge of this approach was the ability to visualize and safely dissect the contralateral lobe while adequately identifying and avoiding injury to the recurrent laryngeal nerve (RLN) and parathyroid glands.
In this study, 3 human cadaver models were initially used to validate the technical feasibility. Following affirmation of the technical feasibility of the procedure, we used the animal (pig) model for live tissue study before attempting it on a human patient. Technical feasibility was arbitrarily defined as the ability to adequately visualize the target gland and its adjacent vital structures (i.e., RLN, parathyroid glands, carotid artery, jugular vein, and others), the ability to safely dissect and mobilize, and the ability to complete the procedure within a time period commensurate with a learning curve model.
Cadaver Model Operative Technique
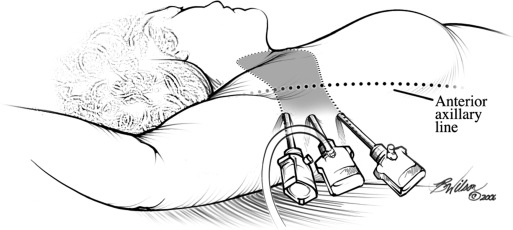
Three 5-mm incisions were made in the anterior axillary line beneath the pectoralis major muscle. Using two 2-mm Steinman pins, blunt dissection beneath the platysma and superior to the pectoralis major muscle was performed to develop the initial working space. The working space was insufflated with CO2 insufflation of 10 mm Hg, and dissection of the connective tissue continued with the Harmonic scalpel and scissor cautery. The sternocleidomastoid muscle was identified, and the plane between the sternocleidomastoid and the sternohyoid muscle was dissected. After elevating the sternohyoid muscle, the sternothyroid muscle was visualized and retracted anteriorly exposing the ipsilateral thyroid gland. The inferior pedicle was bluntly dissected while the RLN was identified. The vessels were then clipped and divided. Smaller vessels were divided by using the Harmonic scalpel (Ethicon Endo-Surgery, Cincinnati, OH) exposing the ligament of Berry. This ligament was divided to mobilize the gland and to allow exposure of the superior thyroid pedicle. The superior thyroid vessels were dissected, clipped, and divided from within the capsule of the gland. Dissection of the gland completely from the anterior trachea facilitated retraction of the gland medially exposing the contralateral side. Under direct visualization, the vessels of the contralateral inferior pole were dissected near the thyroid capsule, ligated, and divided. This maneuver allowed further medial and cephalad retraction of the thyroid gland. Using the 45-degree 5-mm endoscope, the contralateral RLN was identified. On the second cadaver, the nerve could not be adequately identified until the trocar housing the 5-mm 45-degree scope was placed medial to the anterior axillary line (Figure 1) on to the anterior chest wall location to thoroughly inspect the contralateral tracheoesophageal groove. Subsequently, the nerve and parathyroid glands were visualized by using this additional maneuver. After nerve and parathyroid identification, the Harmonic scalpel was used to dissect and transect the remainder of the thyroid gland up to the contralateral superior pole. Due to some difficulty exposing this portion of the gland, division of the sternothyroid muscle was necessary. After division of the superior pole, the total gland was extracted through an extended axillary incision.
Figure 1.
Lateral view of transaxillary approach.
Pig Model Operative Technique
The operative procedure was performed with the pig under general anesthesia. After positioning the animal to extend the neck, three 5-mm trocars were placed along the lateral chest wall near the axilla. Dissection along the anterior chest wall directed toward the animal's cervical region was accomplished using the Harmonic scalpel. The sternocleidomastoid muscle and the thyroid gland were identified in the fashion previously described.13 After dissection of the ipsilateral gland, the opposite lobe was explored. The isthmus of the gland was grasped and dissected, freeing the posterior gland from the anterior surface of the trachea. Using gentle traction on the gland, the contralateral inferior lobe was retracted superiorly exposing the inferior vascular pedicle as it penetrated into the thyroid gland. Gentle dissection of the surrounding areolar tissue isolated the vessels that were clipped and divided. This increased the mobility of the gland and allowed further retraction of the gland superiorly and medially. The recurrent laryngeal nerve was now easily appreciated with the 5-mm 45-degree endoscope. Staying within the capsule of the gland, dissection of the middle thyroid vein was accomplished. The 5-mm Harmonic scalpel was used to dissect, clip, and divide smaller vessels to the thyroid. This maneuver allowed complete mobility of the gland exposing the superior thyroid pedicle. The superior vessels were then clipped and divided freeing the entire gland, all the while protecting the recurrent laryngeal nerve. The gland was removed through an extended lateral incision.
Human Patient Operative Technique
After IRB approval and informed patient consent, 3 female patients were selected for endoscopic near total thyroidectomy each with a history of enlarging multinodular goiter.2 All 3 patients had been followed on an average of 7 years (range, 4 to 19) with a history of a gradual increase in size of the gland before consideration for surgical extirpation. Average age in this group was 31 years (range, 18 to 61). Fine needle aspiration was performed in all patients. Preoperatively, no clinical or pathological evidence of malignancy was present.
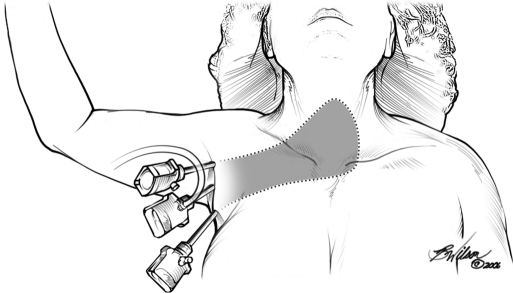
The patient was placed on the operating table and general anesthesia was administered. The patient's arm was abducted at 90 degrees to the vertical axis of the body to expose the axilla (Figure 2). Three 5-mm incisions were made, and initial dissection of the working space was accomplished with blunt 3-mm Steinman pins beneath the platysma and anterior to the pectoralis major muscle. Three 5-mm trocars were placed through the incisions and directed towards the thyroid gland (Figure 3). Insufflation of CO2 at an initial pressure of 7 mm Hg pressure was used to maintain the working space. Dissection was then carried out to reach the sternocleidomastoid muscle and thyroid gland.
Figure 2.
Positioning of the patient for Near Total thyroidectomy
Figure 3.
Dissection area using transaxillary approach.
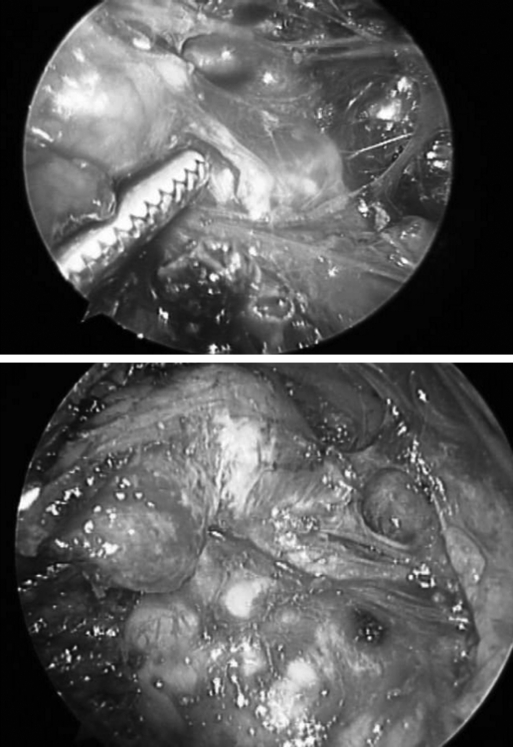
The ipsilateral thyroid lobe was identified and mobilized. After mobilization of the isthmus from the anterior surface of the trachea, the gland was grasped and gently retracted anteromedially. This maneuver was facilitated by division of the sternothyroid muscle leaving the more superficial sternohyoid muscle intact. This allowed greater anterior retraction, exposing the contralateral inferior thyroid pole. Complete dissection of the junction between the thyroid capsule and the contralateral inferior thyroid vessels was accomplished. These vessels were then clipped and divided. Complete mobility of the gland was accomplished, and the contralateral superior thyroid pedicle was exposed (Figure 4). The superior vessels were then clipped and divided, freeing the entire gland while protecting the recurrent laryngeal nerve. The gland, completely detached, was placed in an Endocatch (Ethicon Endo-Surgery, Cincinnati, OH) retrieval bag and removed through an extended lateral incision within the axilla. The paratracheal spaces were inspected for hemostasis. A 7-mm Blake drain was placed within the thyroid bed and anterior chest wall, and brought out through one of the 5-mm axillary port sites (Figure 5).
Figure 4.
Identification of recurrent laryngeal nerve and parathyroid gland.
Figure 5.
Postoperative day 2 with drain.
RESULTS
Before initiating the present study, we successfully completed 32 unilateral thyroidectomy procedures for benign thyroid disease by using an endoscopic transaxillary approach. The operative time for these procedures averaged 142 minutes (range, 57 to 327) and has remained relatively stable over the last 15 cases.
In the cadaver and pig models, optimal magnified visualization was achieved using the endoscopic approach.4 Although identification of the thyroid gland and adjacent vital structures was easier in the porcine model, the cadaver model more accurately represented the anatomy as seen in live patients. Dissection of the ipsilateral and contralateral thyroid lobes was accomplished with good visualization of the RLN and parathyroid glands. Combined operating times in both models averaged 112 minutes (range, 109 to 327).
Following successful completion of total thyroidectomy using cadaver and live animal models, we proceeded to evaluate safety and efficacy in humans. In this clinical study, 3 live human subjects presented with a diffusely enlarged multinodular goiter that had clinically increased in size over the past year. All 3 patients had unilateral lobe sizes of 4 cm or less as determined by preoperative thyroid ultrasonography. Fine needle aspiration revealed benign colloid cells in all 3 individuals.
Upon operative dissection, as described above, we were successful at visualization of the ipsilateral thyroid gland in all models. Further dissection allowed clear visualization of the contralateral lobe and its adjacent major structures. The recurrent laryngeal nerve and parathyroid glands were clearly identified. The operative time for these patients averaged 128 minutes (range, 99 to 195) (Table 1). The axillary incision had to be extended to an average 35 mm (range, 18 to 49) to adequately extract the thyroid specimen. All incisions were covered with the subject's arm in the normal anatomic position (Figure 6). There were no injuries to the recurrent laryngeal nerve or parathyroid glands.3 Dissection in a parallel plane to the anterior axillary line and above the pectoralis major muscle avoided injury to other structures within the axilla, including the long thoracic, thoracodorsal, and brachial plexus nerves. There were no postoperative complications, such as bleeding or hoarseness, and no adverse sequelae of CO2 insufflation. There were no postoperative complaints of dysphagia or stridor. All patients were discharged on postoperative day 2, and all drains were removed within 72 hours of surgery.
Table 1.
Operative Time (Minutes)
| Model | One (min) | Two (min) | Three (min) | Mean Operative Time |
|---|---|---|---|---|
| Porcine | 91 | 102 | 83 | 92 |
| Cadaver | 135 | 115 | 146 | 132 |
| Human | 195 | 90 | 99 | 128 |
Figure 6.
Postoperative day 14 with drain removed.
DISCUSSION
Endoscopic thyroidectomy provides a minimally invasive approach to the thyroid gland, resulting in improved visualization of anatomic structures for the surgeon and superior cosmetic results for the patient. The most commonly performed endoscopic approach places the trocars anteriorly within the neck region to directly access the thyroid.12 Though this direct approach has been shown to be the least invasive, the cosmetic results may prove less than optimal in patients with large thyroid lesions that require extension of the neck incision for extraction. Furthermore, if it becomes unsafe to proceed endoscopically using the direct approach (bleeding, poor visualization, and other complications), conversion to the open approach would result in several visible neck incisions in addition to the open cervical incision, giving an unsatisfactory cosmetic outcome.
The endoscopic transaxillary approach conceals the incisions within the axilla, allowing removal of larger lesions without compromising cosmesis. The remote transaxillary technique provides access to the thyroid gland by subcutaneously traversing the chest wall via a lateral videoscopic approach avoiding any incision in the cervical area. Because of the amount of tissue dissected to reach the target area, this procedure is the most invasive of the minimal access techniques to the thyroid gland. Such an approach minimizes any perceived cosmetic deformity and possible anxiety concerning the cosmetic outcome of the surgery.6 Because there is no difference in hospital stay between this procedure and the direct cervical approach, and because postoperative pain may be increased with this maximally invasive technique, better cosmesis and possibly safer dissection through improved visualization may be the only perceived benefits of this particular approach. Although the endoscope provides excellent visualization and magnification, the unconventional approach from the lateral fields requires thorough knowledge of the anatomy in this area. This technique has been previously described for benign unilateral thyroid disease with safety and excellent cosmetic results.9,11 Although the transaxillary approach has been deemed safe and effective in patients with unilateral disease, its application in bilateral disease has not been explored. Possibly inadequate visualization of the contralateral anatomy, resulting in inadequate and precarious dissection, may be the reason.
CONCLUSION
Although endoscopic thyroid surgery has been shown to be safe and effective, its use remains limited. Advantages of this technique include superior visualization of local anatomy and improved cosmesis. Most endoscopic techniques that approach the gland from the anterior neck or chest surface limit the size of gland that can be removed to avoid unsatisfactory cosmetic results. A significant percentage of patients presenting with thyroid disorders will harbor multifocal disease that may require total or near total thyroidectomy.7 To date, this approach has not been studied for malignant disease of the thyroid gland and is therefore not recommended.
In our study, visualization of the recurrent laryngeal nerve and parathyroid glands was clear, detailed, and without doubt. For an endoscopic approach to be a viable alternative to open surgery, it should be a feasible approach for a majority of surgical diseases involving the thyroid gland. This study shows that endoscopic transaxillary thyroidectomy is safe and feasible in select patients with multifocal and bilateral thyroid disease. For select patients with multinodular goiters transaxillary thyroidectomy a useful and cosmetically superior alternative to open thyroidectomy.
References:
- 1. Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg. 1996; 83 ( 6): 875. [DOI] [PubMed] [Google Scholar]
- 2. Inabnet WB, Chu CA. Transcervical endoscopic-assisted mediastinal parathyroidectomy with intraoperative parathyroid hormone monitoring. Surg Endosc. 2003; 17 ( 10): 1678. [DOI] [PubMed] [Google Scholar]
- 3. Miccoli P, Bendinelli C, Conte M, et al. Endoscopic parathyroidectomy by a gasless approach. J Laparoendosc Adv Surg Tech A. 1998; 8 ( 4): 189– 194 [DOI] [PubMed] [Google Scholar]
- 4. Miccoli P, Bendinelli C, Vignali E, et al. Endoscopic parathyroidectomy: report of an initial experience. Surgery. 1998; 124 ( 6): 1077– 1079 [DOI] [PubMed] [Google Scholar]
- 5. Naitoh T, Gagner M, Garcia-Ruiz A, Heniford BT. Endoscopic endocrine surgery in the neck. An initial report of endoscopic subtotal parathyroidectomy. Surg Endosc. 1998; 12 ( 3): 202– 205 [DOI] [PubMed] [Google Scholar]
- 6. Ng WT. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech. 2000; 10 ( 5): 339– 340 [PubMed] [Google Scholar]
- 7. Ohgami M, Ishii S, Arisawa Y, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech. 2000; 10 ( 1): 1– 4 [PubMed] [Google Scholar]
- 8. Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy by the axillary approach. Surg Endosc. 2001; 15 ( 11): 1362– 1364 [DOI] [PubMed] [Google Scholar]
- 9. Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy and parathyroidectomy by the axillary approach. A preliminary report. Surg Endosc. 2002; 16 ( 1): 92– 95 [DOI] [PubMed] [Google Scholar]
- 10. Ikeda Y, Takami H, Niimi M, et al. Endoscopic total parathyroidectomy by the anterior chest approach for renal hyper-parathyroidism. Surg Endosc. 2002; 16 ( 2): 320– 322 [DOI] [PubMed] [Google Scholar]
- 11. Chantawibul S, Lokechareonlarp S, Pokawatana C. Total video endoscopic thyroidectomy by an axillary approach. J Laparoendosc Adv Surg Tech A. 2003; 13 ( 5): 295– 299 [DOI] [PubMed] [Google Scholar]
- 12. Inabnet WB, 3rd, Jacob BP, Gagner M. Minimally invasive endoscopic thyroidectomy by a cervical approach. Surg Endosc. 2003; 17 ( 11): 1808– 1811 [DOI] [PubMed] [Google Scholar]
- 13. Duncan T, Ejeh A, et al. Thyroidectomy using an endoscopic transaxillary approach: our early experience. In press [DOI] [PubMed] [Google Scholar]