Abstract
Background:
Dieulafoy's lesion is a vascular malformation, usually of the stomach but occasionally of the small or large bowel. It is an uncommon, but clinically significant, source of upper gastrointestinal hemorrhage. Three cases have been reported in the literature of laparoscopic gastric wedge resection of these lesions by using intraoperative endoscopic localization. We present the only reported case of preoperative endoscopic localization of a Dieulafoy's lesion with India ink and an endoscopic clip before laparoscopic resection.
Case Report:
We present an 82-year-old female patient who presented to the emergency department with 3 episodes of hematemesis. Esophagogastroduodenoscopy revealed an actively bleeding Dieulafoy's lesion in the fundus of the stomach along the greater curvature, which was controlled endoscopically. However, the patient had a recurrent episode of bleeding. Repeat endoscopy was performed and the lesion was tagged with 2 endoscopic clips and marked with India ink. A laparoscopic wedge resection was performed after the India ink was identified in the fundus. The patient did well postoperatively.
Conclusion:
Preoperative localization of a Dieulafoy's lesion with India ink and endoscopic clips before laparoscopic wedge resection is a feasible procedure. Therefore, no need exists for intraoperative endoscopy to aid in the localization, as previously reported.
Keywords: Dieulafoy's lesion, Laparoscopy, India ink
INTRODUCTION
Gallard in 1884 described Dieulafoy's lesions as a “military aneurysm”1; In 1898, Dieulafoy, a French surgeon, referred to these lesions as exulceratio simplex and felt that these were the result of injury to the gastric mucosa with subsequent hemorrhage from a normal submucosal artery.2 Since this early description of Dieulafoy's lesion, today we know that they are abnormal, submucosal, “caliber-persistent” arteries that typically protrude through a minute mucosal defect, leading to gastrointestinal hemorrhage.3
Management of Dieulafoy's lesion has evolved over the years. Before the advent of endoscopy, radical surgeries, such as subtotal or total gastrectomies, were performed with high morbidity. Today, management of bleeding from Dieulafoy's lesion is mostly endoscopic with superior results. The role of surgery has been significantly reduced. However, multiple endoscopies may be required at times to identify a Dieulafoy's lesion. Yet, 3% to 16% of the time, endoscopic treatment may fail to resolve the bleeding lesion, resulting in the need surgery.4
Minimally invasive surgery has been shown to play a greater role in the surgical management of a Dieulafoy's lesion that fails endoscopic treatment. Recently, in conjunction with intraoperative endoscopy used for localization, laparoscopic resection of Dieulafoy's lesion has been successfully performed.5–8
CASE REPORT
We present an 82-year-old female patient who presented to the emergency department with 3 episodes of hematemesis. She underwent an esophagogastroduodenoscopy (EGD) that revealed an actively bleeding Dieulafoy's lesion in the fundus of the stomach along the greater curvature. The bleeding was controlled with an epinephrine injection and electrocautery. However, the patient had a second episode of hematemesis. She underwent a repeat EGD, and the lesion was tagged with 2 endoscopic clips and marked with India ink in preparation for surgical treatment.
The patient was then taken to the operating room. She was placed in a supine position and surgery was performed via 4 ports, two 5-mm and two 5- to 11-mm instrument ports. The larger ports were used for placement of the stapler and the laparoscope. The stomach was exposed with the liver retracted by using Nathanson Hook Retractors (Automated Medical Products Corps, Edison, NJ). The India ink stain clearly demarcated the lesion on the fundus of the stomach. Laparoscopic gastric wedge resection was performed using an endo-GIA universal stapler system (US Surgical, Norwalk, CT) with a cartridge 60 mm in length and 3.5 mm in thickness (Figure 1). The staple line was reinforced with bovine pericardial strip. Once removed, the specimen was opened, and the endoscopically placed clips were identified within the specimen (Figure 2).
Figure 1.
Wedge resected specimen of Dieulafoy's lesion of the stomach, identified by the India ink stain on the serosa.
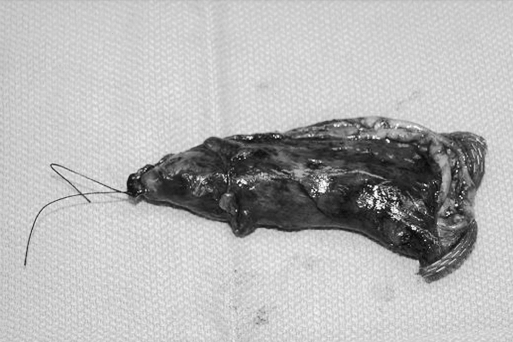
Figure 2.
Gastric wedge resected specimen of the stomach with the Dieulafoy's lesion. The specimen is opened and the Dieulafoy's lesion can be identified by the hemoclips that were placed endoscopically.
The patient tolerated the procedure well and was discharged on postoperative day 2. The final pathology confirmed the confinement of the Dieulafoy lesion within the resected specimen. The patient was doing well at 6-month follow-up.
DISCUSSION
Dieulafoy's lesion is commonly located in the proximal aspect of the stomach and accounts for 1% to 5.8% of nonvariceal bleeds.4 Over the years, endoscopy has been successful in the diagnosis and treatment of bleeding Dieulafoy's ulcers. Minimally invasive surgery has further improved results of surgical treatment with the advantages of a shorter hospital stay and faster recovery. However, intraoperative endoscopy is necessary for localization of the lesion. This would require the presence of an experienced endoscopist in the operating room to identify the lesion.
Preoperative endoscopic tattooing is extensively used to localize lesions, such as those in the colon, during open surgery. Ottenjann et al9 in 1969 described its use in the stomach. Later, Ponsky et al10 in 1975 described its use in the colon. India ink is commonly used and is composed of colloidal suspension of carbon particles in a solution of organic and nonorganic substances used as stabilizing diluents and surfactants.11 They are safe, superior, and last for 48 hours after initial injection before getting gradually reabsorbed.11 Although preoperative marking has been widely used especially for colon resections in open surgery, Beretvas and Ponsky12 recently described the feasibility of tattooing the gastrointestinal tract with India ink in patients undergoing laparoscopic surgery. They were successful in visualizing the India ink on the serosa while performing laparoscopic surgery in 15 patients.
Laparoscopic transgastric resection of Dieulafoy's lesion involving an anterior gastrotomy and resection of the lesion, without the need for endoscopy, has been performed.13 However, such procedures involve an unnecessary gastrotomy. There are 3 case reports in the literature of laparoscopic resection of Dieulafoy's lesions.5–7 All 3 cases were performed with intraoperative endoscopic localization. Once pneumoperitoneum was established, the gastroscope was passed into the stomach and air was insufflated. It was necessary to dim or turn off the laparoscopic light and to retroflex the gastroscope to see the ulcer. The area was marked by clips or suture laparoscopically and resection was then performed. Another method used by Mixter GC et al8 involved a combined endoscopic and laparoscopic approach to identification and ligation of the vessel(s) that feeds the ulcer without the need for resection. Our technique used preoperative endoscopic injection of the lesion with India ink and clip placement for exact localization. Clip length varies from 5 mm to 20 mm. The most common problem with clip placement is that it could fall out before surgery. In such a case, the India ink is still present to guide the resection. Clips have not been known or reported to interfere with the staple line or to cause disruption of the staple line. We have not encountered any problem, but we have had very limited experience using the stapler for tissue with this type of clips. However, it is very rare for the stapler to malfunction when it is used to divide across another staple line. If the malfunction occurs, it is usually quite apparent so the problem can be corrected immediately.
Results of laparoscopic wedge resection are superior when compared with oversewing the Dieulafoy's lesion.5 However, when lesions are situated within 6 cm of the gastroesophageal junction, wedge resection may not be feasible, and in such situations, oversewing the lesion or laparoscopic clip placement on the vessel feeding the lesion may be used as part of the surgeon's armamentarium for the treatment of this disease.5,8
CONCLUSION
There is no doubt that the primary management of Dieulafoy's lesion is endoscopic. However, surgery is the only option for patients who fail endoscopic management. Although a combination of laparoscopic wedge resection and intraoperative endoscopic localization has been used, we feel that this form of localization is not necessary. We showed that endoscopic marking of the bleeding Dieulafoy's lesion with India ink and clips can alleviate the use of intraoperative endoscopy.
Footnotes
Presented at the 13th International Congress and Endo Expo 2004, SLS Annual Meeting, New York, New York, USA, September 29 –October 2, 2004.
References:
- 1. Gallard T. Aneurysmes miliares de l’estomac lieu a des hematemeses mortelles. Bull Mem Soc Med hop Paris. 1884; 1: 84– 91 [Google Scholar]
- 2. Dieulafoy G. Exulceratio simplex. L’intervention chirurgicale dans hematemesis foudroyantes consecutives a l’exulceration simple de l’estomac. Bull Mem Soc Med Hop Paris. 1898; 49: 49– 84 [Google Scholar]
- 3. Yarze JC. Routine endoscopic “marking” of Dieulafoy-like lesions. Am J Gastroenterol. 2001; 96: 264– 265 [DOI] [PubMed] [Google Scholar]
- 4. Lee YT, Walmsley RS, Leong RW, Sung JJ. Dieulafoy's lesion. Gastrointest Endosc. 2003; 58: 236– 243 [DOI] [PubMed] [Google Scholar]
- 5. Draper G, Layani L, McLeish J. Management of Dieulafoy's disease with combined endoscopy and laparoscopic gastric wedge resection. Aust N Z J Surg. 1999; 69: 156– 158 [DOI] [PubMed] [Google Scholar]
- 6. Bouillot JL, Aubertin JM, Fornes P, Petite JP, Alexandre JH. Dieulafoy's ulcer: combined endoscopic and laparoscopic treatment. Endoscopy. 1996; 28: 394– 395 [DOI] [PubMed] [Google Scholar]
- 7. Karanfilian GR, Yang KH, Gendler S. Resection of Dielafoy's lesion by a combined endoscopic and laparoscopic approach. J Laparoendosc Surg. 1996; 6 ( 5): 345– 348 [DOI] [PubMed] [Google Scholar]
- 8. Mixter GC, Sullivan AC. Control of proximal gastric bleeding: Combined laparoscopic and endoscopic approach. J Laparoendosc Surg. 1992; 2 ( 2): 105– 109 [DOI] [PubMed] [Google Scholar]
- 9. Ottenjann R, Peter H, Elster K. Gastroscopic marking of the fundus antrum border. In: Maratka Z, Setka J. (eds). Endoscopy of the Digestive System. New York, NY: Karger; 1969 [Google Scholar]
- 10. Ponsky JL, King JF. Endoscopic marking of colonic lesions. Gastrointest Endosc. 1975; 22: 42– 43 [DOI] [PubMed] [Google Scholar]
- 11. Ginsberg GG, Barkun AN, Bosco JJ, et al. Endoscopic tattooing: February 2002. Gastrointest Endosc. 2002; 55: 811– 814 [DOI] [PubMed] [Google Scholar]
- 12. Beretvas RI, Ponsky J. Endoscopic marking: an adjunct to laparoscopic gastrointestinal surgery. Surg Endosc. 2001; 15: 1202– 1203 [DOI] [PubMed] [Google Scholar]
- 13. Proske JM, Vons C. Transgastric laparoscopic approach for resection of hemorrhagic Dieulafoy's vascular malformation. Surg Endosc. 2004; 18: 554– 556 [DOI] [PubMed] [Google Scholar]