Abstract
Background:
A Spigelian hernia is a congenital defect in the transversus aponeurosis fascia. Traditionally, an anterior hernioplasty was used to repair these defects. This study aimed to document our experience with laparoscopic transabdominal preperitoneal repair for Spigelian hernia.
Methods:
Eight patients underwent laparoscopic transabdominal Spigelian hernia repair. All patients underwent creation of a peritoneal flap, sac dissection, identification and approximation of the fascial defect, mesh reinforcement, and reperitonealization.
Results:
All patients presented with pain. An intermittent palpable mass was noticed in 4 patients. One third of the patients had undergone prior surgery and none had an incisional hernia. Only 1 patient presented with severe pain for 1 day; however, there was no bowel strangulation intraoperatively. All patients underwent laparoscopic transabdominal preperitoneal repair. No postoperative complications occurred. There have been no recurrences at a mean follow-up of 41 months (range, 8 to 96).
Conclusion:
Laparoscopic transabdominal preperitoneal repair of Spigelian hernia is safe, easy, and feasible for experienced laparoscopic surgeons.
Keywords: Spigelian hernia, Adults, Laparoscopy, Preperitoneal repair
INTRODUCTION
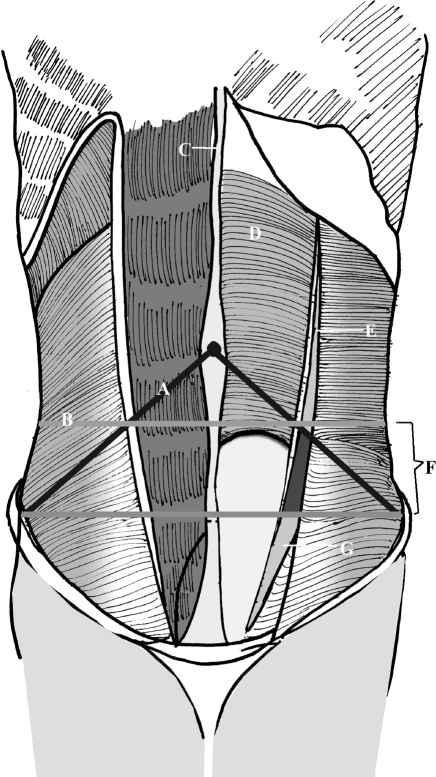
Spigelian hernia is a protrusion of preperitoneal fat, a sac of peritoneum, an organ, through a congenital defect, or weakness in the Spigelian fascia.1,2 The hernial orifice of the Spigelian hernia is usually located along the semilunar line (Spigelian line) through the transversus abdominis aponeurosis (Spigelian fascia) close to the level of arcuate line.3 Most herniae occur in the region of the Spigelian belt (Figure 1). Also, most are high Spigelian herniae (Figure 2).
Figure 1.
Spigelian aponeurosis. (A) Munros line, (B) imaginary line 6 cm from interspinal line, (C) linea alba, (D) posterior rectus sheath, (E) spigelian line (semilunar line), (F) spigelian belt, (G) spigelian aponeurosis, (H) interspinal line.
Figure 2.
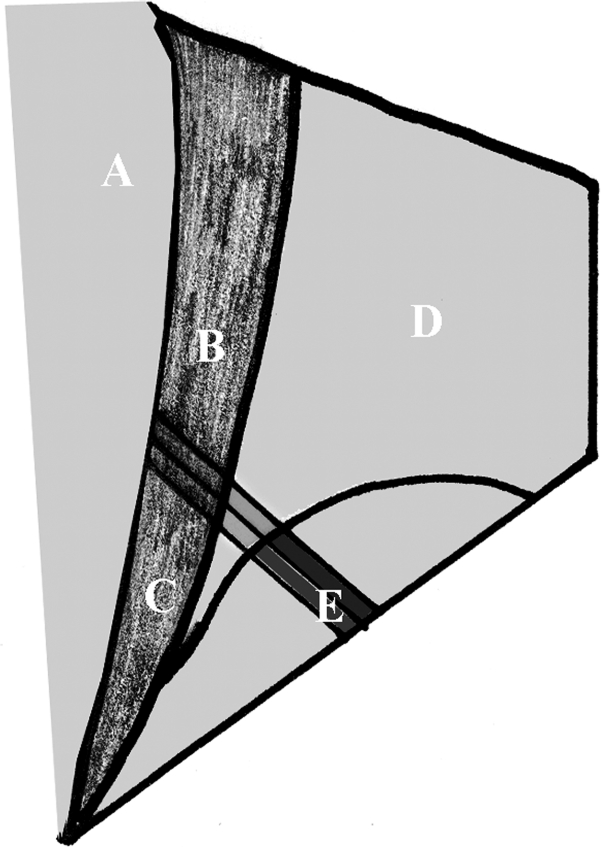
Spigelian aponeurosis. (A) Rectus muscle, (B) area of high spigelian hernia, (C) area of low spigelian hernia, (D) transversus abdominis, (E) inferior epigastric vessels.
This study aimed to document our experience with laparoscopic transabdominal preperitoneal repair of Spigelian hernia.
METHODS
All patients were admitted in the evening 1 day before surgery and discharged within 24 hours to 48 hours after surgery. Eight herniae underwent laparoscopic Spigelian hernia repair. Patients were placed in a supine position. Pneumoperitoneum was created by the closed Veress needle technique. A triangular orientation was maintained with a 10-mm telescope in the epigastric region and two 5-mm working ports on either side, pararectally. Findings were noted and contents, if any, reduced at this stage (Figures 3 through 7).
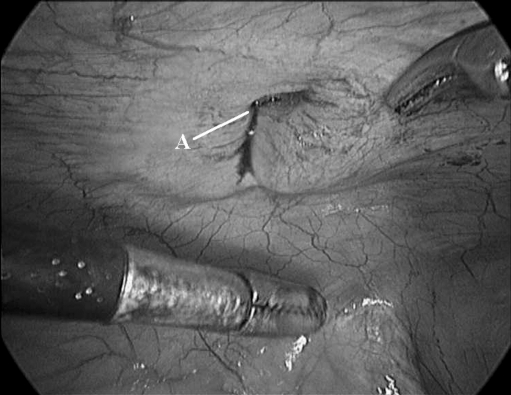
Figure 3.
(A) Spigelian hernial defect without any contents.
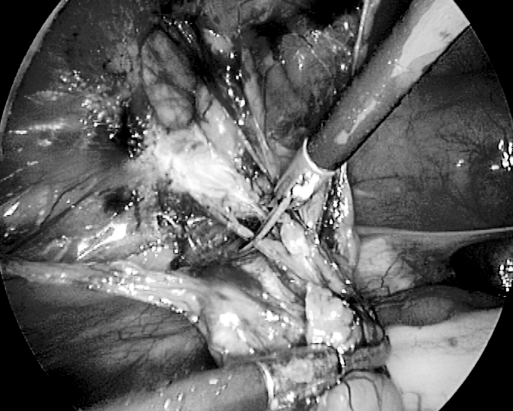
Figure 7.
Dissection of sac after creation of peritoneal flap.
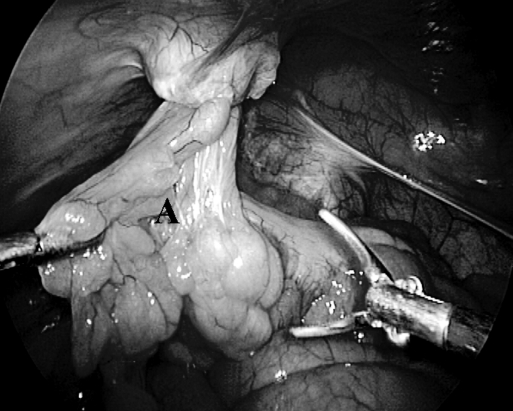
Figure 4.
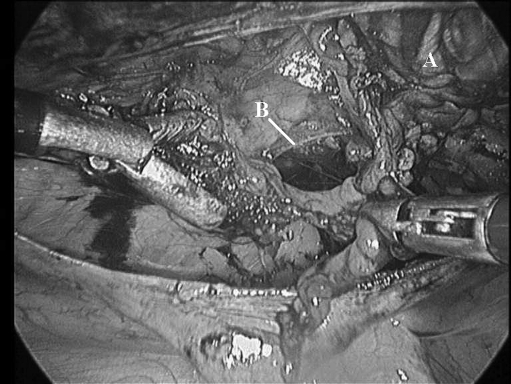
Spigelian hernial defect with sigmoid mesentery as contents. (A) Rectus abdominis muscle, (B) Spigelian defect.
Figure 5.
(A) Reduction of the sigmoid mesentery.
Figure 6.
Spigelian defect after reduction of contents. (A) Inferior epigastric vessels, (B) defect visualized above the inferior epigastric vessels, (C) Sigmoid colon.
A peritoneal flap (Figure 7) was created similar to the transabdominal approach for laparoscopic inguinal hernia repair.4 The sac was dissected all around. The defect was identified and closed with polypropylene sutures (Figures 8 and 9). The entire Spigelian fascia was now reinforced with a polypropylene mesh (Figure 10), which was fixed with 2 or 3 interrupted polypropylene sutures (Figure 11). The peritoneal flap was approximated with absorbable sutures (Figure 12). No drain was placed. Abdomen was deflated and subcuticular sutures placed for skin closure. Only the epigastric port-site fascia was closed with absorbable suture.
Figure 8.
Spigelian defect. (A) Inferior epigastric vessels, (B) defect.
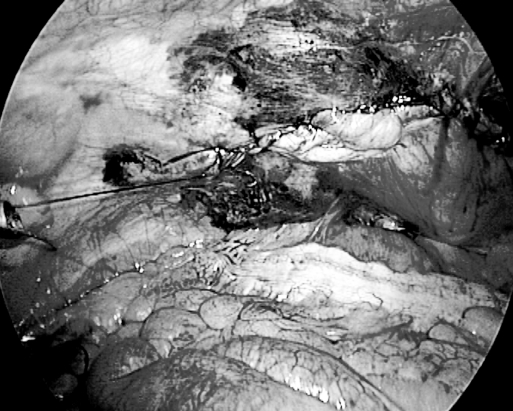
Figure 9.
Approximation of the defect by intracorporeal polypropylene suture.
Figure 10.
Defect reinforced with polypropylene mesh.
Figure 11.
Mesh fixation with intracorporeal polypropylene suture.
Figure 12.
Completion of the peritoneal flap closure with absorbable suture.
RESULTS
Eight patients, 7 female and 1 male, underwent laparoscopic repair of Spigelian hernias. Patients’ mean age was 42 years (range, 35 to 60). All patients presented with symptoms of abdominal pain and an intermittent palpable mass was noted in 4 patients. One patient had pain unrelated to the hernia. The pain was described as localized in 5 patients and diffuse in the other 3 patients. Only 1 patient had experienced severe pain for 1 day. Seven patients had no significant preoperative morbidity. One (female) patient had chronic obstructive pulmonary disease, controlled with medication. One third of the patients had undergone prior surgery and none had incisional hernia. One patient had undergone previous abdominal surgery followed by ventral hernia repair. Two patients had undergone surgery for gynecological conditions. None of them were laparoscopic surgeries.
Abdominal ultrasound showed the defect in the echo line from the aponeurosis (Figure 13). This defect was noted in all patients, and ultrasound aided the diagnosis in 4 of the patients, without the combination of pain and palpable mass. Thus, all patients were diagnosed on the basis of patient history, and clinical and ultrasound examination. None underwent herniography or computed tomography. All patients underwent laparoscopic transabdominal preperitoneal repair of Spigelian hernia. The patient who presented with severe pain for 1 day had a small bowel loop as contents. However, the bowel loop showed no signs of strangulation. Two more patients had omentum and sigmoid colon mesentery. In all cases, contents were reduced easily. There was no inadvertent trauma during reduction. All patients underwent defect closure; mesh re-enforcement; and re-peritonealization.
Figure 13.
Ultrasound image of spigelian hernia. Defect is shown (between the arrows).
No postoperative complications occurred. All patients were discharged within 24 hours to 48 hours. There have been no recurrences at a mean follow-up of 41 months (range, 8 to 96). The demographic and technical data are mentioned in Table 1.5,6
Table 1.
Demographic and Technical Details
| Spangen1 | Larson and Farley5 | MorenoEgea et al6 | Palanivelu | |
|---|---|---|---|---|
| No. of Patients | 24 | 76 | 28 | 8 |
| No. of Hernias | 25 | 81 | 28 | 8 |
| Mean Age (years) | 35 | 63 | 60 | 42 |
| Female (%) | 92 | 51 | 71 | 88 |
| Left (%) | 25 | 52 | 64 | 75 |
| Pain (%) | 100 | 26 | — | 100 |
| Palpable Mass (%) | 50 | 38 | — | 50 |
| Palpable Mass and Pain (%) | 21 | 29 | — | 50 |
| Acute Presentation (%) | 10 | 10 | 21 | 12 |
| Strangulation (%) | 8 | 17 | — | 0 |
| Recurrence (%) | — | 4 | — | 0 |
| Mean Follow-up (years) | — | 8 | 3.4 | 3.4 |
DISCUSSION
Spigelian or lateral ventral hernia is a rare pathology, representing about 2% of all abdominal wall hernias.7 Its diagnosis requires a high index of suspicion, given the lack of consistent symptoms and signs. Thus, a physician needs a combination of history, physical examination, and preoperative imaging to secure the diagnosis.
The predominant symptom was pain, which varied in its location and severity. A palpable mass was noted in 4 patients. Thus, a combination of palpable and reducible mass makes diagnosis easy. Predisposing factors were observed in most patients with hernia. In our study, 2 patients had undergone surgery for gynecological conditions; 1 patient underwent abdominal surgery followed by ventral hernia repair. Thus, one third of the patients had undergone a previous surgery but had no incisional hernia. This suggests a possibility of an increased risk of spigelian hernia development. Also, a prior laparoscopic surgery appears to be a risk factor, due to the creation of pneumoperitoneum.8 However, none of the patients had undergone laparoscopic surgery. All patients underwent an abdominal ultrasound, which aided diagnosis in those patients without the combination of pain and palpable mass. Abdominal sonography or computed tomography may aid diagnosis.9 Abdominal sonography scanning is advantageous, as it is noninvasive, easily available, inexpensive, and can detect the hernial orifice in the Spigelian fascia. All the defects were diagnosed by abdominal sonography. None of our patients underwent computed tomography.
Given the high rate of incarceration/strangulation, the diagnosis of Spigelian hernia is an indication for surgical repair. Most repairs are done electively. Laparoscopic repairs reported include the preperitoneal approach with polypropylene mesh,10 onlay mesh repairs using expanded polytetrafluoroethylene,11 and composite mesh repairs.12 We performed laparoscopic transabdominal preperitoneal repair for 8 Spigelian herniae. A similar repair technique has been reported by Kasirajan et al.13 No postoperative complications occurred.
CONCLUSION
Laparoscopic transabdominal preperitoneal repair of Spigelian herniae is safe, easy, and feasible for experienced laparoscopic surgeons.
References:
- 1. Spangen L. Spigelian hernia. Surg Clin North Am. 1984; 64: 351– 366 [DOI] [PubMed] [Google Scholar]
- 2. Kalaba Z. Spigelian hernia: a case of typical Spigelian hernia in an elderly man. Ugeskr Laeger. 1999; 161: 2095– 2096 [PubMed] [Google Scholar]
- 3. Spangen L. Spigelian hernia. World J Surg. 1989; 13: 573– 580 [DOI] [PubMed] [Google Scholar]
- 4. Palanivelu C. Laparoscopic management of rare hernia. In: Operative Manual of Laparoscopic Hernia Surgery. India: Gem Foundation; 2004; 295: 305 [Google Scholar]
- 5. Larson DW, Farley DR. Spigelian hernias: repair and outcome for 81 patients. World J Surg. 2002; 26 ( 10): 1277– 1281 [DOI] [PubMed] [Google Scholar]
- 6. Moreno-Egea A, Flores B, Girela E, et al. Spigelian hernia: bibliographical study and presentation of a series of 28 patients. Hernia. 2002; 6 ( 4): 167– 170 [DOI] [PubMed] [Google Scholar]
- 7. Ng WT. Incidence and outcome of surgical repair of spigelian hernia. Br J Surg. 2004; 91: 640– 644 [DOI] [PubMed] [Google Scholar]
- 8. Slakey DR, Teplitsky S, Cheng SS. Incarcerated Spigelian hernia following laparoscopic living-donor nephrectomy. JSLS. 2002; 6 ( 3): 217– 219 [PMC free article] [PubMed] [Google Scholar]
- 9. Mostard GJ, van Deursen CT. Diagnostic image (74). A woman with stomach cramps and vomiting. Ned Tijdschr Geneeskd. 2002; 146 ( 5): 209. [PubMed] [Google Scholar]
- 10. Tarnoff M, Rosen M, Brody F. Planned totally extraperitoneal laparoscopic Spigelian hernia repair. Surg Endosc. 2002; 16 ( 2): 259. [DOI] [PubMed] [Google Scholar]
- 11. Appeltans BM, Zeebregts CJ, Cate Hoedemaker HO. Laparoscopic repair of a Spigelian hernia using an expanded polytetrafluoroethylene (ePTFE) mesh. Surg Endosc. 2000; 14 ( 12): 1189 Epub 2000 Sep 28 [DOI] [PubMed] [Google Scholar]
- 12. Barie PS, Thompson WA, Mack CA. Planned laparoscopic repair of a spigelian hernia using a composite prosthesis. J Laparoendosc Surg. 1994; 4 ( 5): 359– 363 [DOI] [PubMed] [Google Scholar]
- 13. Kasirajan K, Lopez J, Lopez R. Laparoscopic technique in the management of Spigelian hernia. J Laparoendosc Adv Surg Tech A. 1997; 7 ( 6): 385– 388 [DOI] [PubMed] [Google Scholar]