Abstract
Background and Objectives:
Umbilical port-site infections after video-laparoscopic cholecystectomy (VLC) are frequent complications. The aim of this prospective randomized study was to verify the validity of topical rifamycin for prevention of post-VLC umbilical infections.
Methods:
From September 2006 to April 2007, 48 patients with uncomplicated cholelithiasis who underwent VLC were enrolled in the study. Enrolled patients were randomized into 2 groups. The first group of 24 patients was treated with topical rifamycin to the umbilicus. The second group of 24 patients was not treated with rifamycin.
Results:
Postoperative umbilical pain with a need for analgesics, presence of signs of inflammation of the umbilical wound, dehiscence of the umbilical skin sutures, and the presence of incisional umbilical hernia on the 60th postoperative day were statistically significantly better in the rifamycin group compared with the control group.
Conclusions:
Topical administration of rifamycin to the umbilicus in the pre-, intra- and postoperative periods was a rapid, safe, and economic way to reduce infective complications after VLC.
Keywords: Laparoscopy, Cholecystectomy, Umbilicus, Rifamycin
INTRODUCTION
The preoperative preparation of a patient for video-laparoscopic cholecystectomy (VLC) is well defined and includes short-term antibiotic therapy, prevention of deep venous thrombosis, and prophylactic cleaning and disinfection of the skin.
Open access, during a Hasson video-laparoscopic cholecystectomy (VLC) technique, is through the umbilicus. The umbilicus is an area rich in bacteria, so we thought it might be useful to use prophylactic topical antibiotic therapy in this region to reduce the incidence of postoperative infection at the umbilical port site.
Umbilical port-site infection during cholecystectomy is reported to be 9%1,2 even for a difficult cholecystectomy.3 The role of topical antibiotic prophylaxis is particularly useful in prevention of local infections in patients with other major risks, such as immunodeficient patients, patients taking immunosuppressive drugs, uncompensated diabetic patients, and others. In the literature, no data show differences in umbilical port-site infections in the video-cholecystectomized patients who undergo different techniques of peritoneal access: Hasson, Veress, and others.4,5
The aim of this study was to evaluate the use of topical prophylactic antibiotic (ie, rifamycin) for prevention of post-VLC infection at the umbilical port-site.
METHODS
From September 2006 to April 2007, 59 patients with uncomplicated gallstones underwent VLC, in the Division of General Surgery, Department of Surgical Sciences of the University of Foggia, School of Medicine, Polyclinic of Foggia, Italy. Of these, 48 patients were enrolled in the study: 30 females and 18 males with a mean age of 38 years (range, 21 to 64), affected by the same clinical scenario.
The laparoscopic access technique used was the Hasson open technique. Rifamycin was chosen as the topical medication because it is has been used by our institution for the treatment of local infections with good results.
Rifamycin is usually used topically for the treatment of infections caused by germs, such as pyodermitis, dermatitis, skin plagues, abscesses, infected wounds, exposed trauma, and fistulae, as recommended based on the technical information about the drug.
We evaluated the results of the topical antibiotic therapy on a series of patients with no added risk for infection. Therefore, we excluded from this study patients with preoperative clinical conditions that might predispose to the development of port-site infection. Patients with un-complicated gallstones were enrolled in the study.
The preoperative exclusion criteria were the following: (1) acute cholecystitis with localized peritonitis; (2) umbilical hernia; (3) immunodepressed patients; (4) uncompensated diabetes. Four patients with uncompensated diabetes and 2 patients with umbilical hernia were excluded from the study.
The intraoperative exclusion criteria were the following: (1) perforation of the gallbladder in the peritoneal cavity during VLC; (2) perforation of the gallbladder during its removal through the umbilicus with bile leakage. The patients who were excluded from the study in the intraoperative phase were the following: 3 patients with intraperitoneal perforations of the gallbladder and 2 patients with perforations during specimen removal through the umbilicus.
The enrolled patients were randomized into 2 groups. The first group (rifamycin group) was treated with rifamycin (24 patients), and the second group (control group) was not treated with rifamycin (24 patients).
This protocol aimed at the controls and at the evaluation only of local infections. So, for all patients, we applied the usual prophylactic systemic antibiotic protocol used within our institution by means of the preoperative intravenous administration of 2 g of ceftriaxone, followed by a second intraoperative dose, and a final dose after 24 hours.
The 2 protocol studies foresaw the application of some simple procedures in the treatment of the umbilicus during the pre-, intra-, and post-VLC phases; the registration of some objective clinical signs and subjective clinical symptoms completed the 2 protocol studies.
The protocol for the rifamycin group patients (rifamycin protocol) had the following phases:
- Preoperative phase. Twelve hours before VLC, the patients underwent the following:
- disinfection of the umbilical and periumbilical skin with iodopovidone;
- application of a sterile medication with 3mL of rifamycin (250 mg) on the umbilicus.
- Intraoperative phase. After gallbladder removal through the umbilicus, all patients underwent:
- suture of the umbilical access: muscular fascia and of the skin wound with Vicryl;
- disinfection of the umbilical wound and periumbilical skin with iodopovidone first, and then with 0.9% saline solution;
- application of a sterile medication with 3mL of rifamycin (250mg) on the umbilical wound.
Postoperative phase. At 12, 24, 36, 48, and 72 hours after VLC, rifamycin was applied in a sterile fashion to the umbilical wound of all the patients. Evaluation of the results of the topical antibiotic prophylaxis, in relation to the development of signs of local infection, was executed by means of subsequent controls at 12, 24, 36, and 48 hours after VLC and on the third, fourth, fifth, sixth, and seventh post-VLC day. The evaluated parameters were the following: (1) umbilical region pain (pain scale from 0 to 5); (2) analgesic drug administration for localized umbilical region pain; (3) signs of inflammation of the umbilical wound (rubor, tumor, calor); (4) purulent leakage through the umbilical wound; (5) dehiscence of the umbilical skin sutures. On the 60th post-VLC day, the possible presence of incisional hernia in the umbilical region was registered.
The protocol for the control group patients (called control protocol) had the same phases as the above-mentioned protocol but rifamycin was not one of the pre-, intra-, and postoperative medications applied. The same surgical equipment was used to perform the VLC operative technique in all 48 cases. The data were analyzed using Statistical Package for Social Sciences software (SPSS version 11.0) by means of the chi-square test.
RESULTS
The topical administration of rifamycin reduced the incidence of omphalitis, a finding that is statistically significant. For evaluation of omphalitis, we chose clinical observation for local signs of inflammation, secretion from the wound, and dehiscence of cutaneous suture. The results were reported by means of histograms.
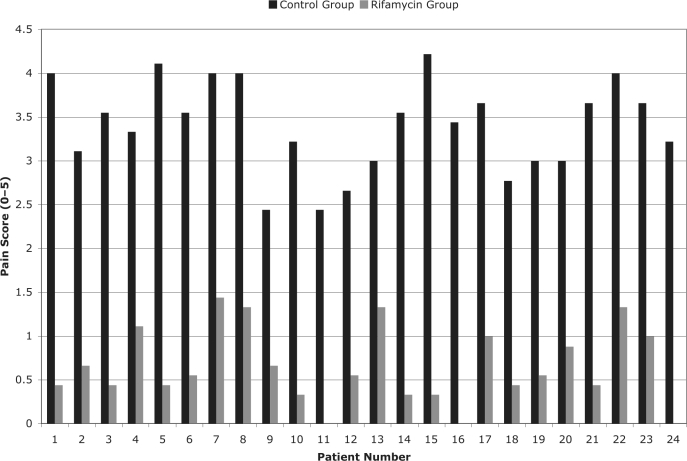
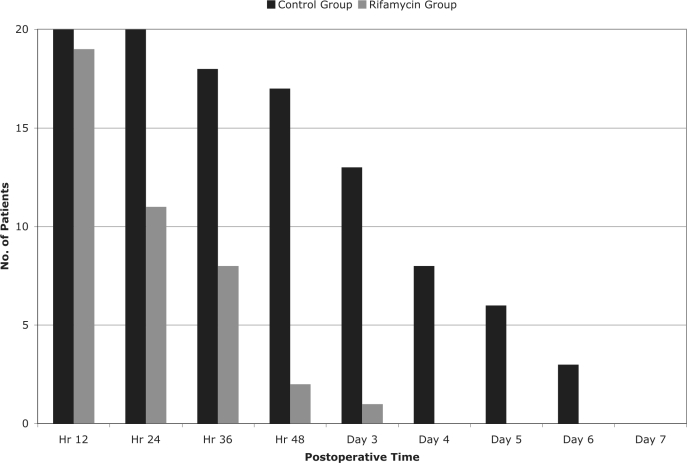
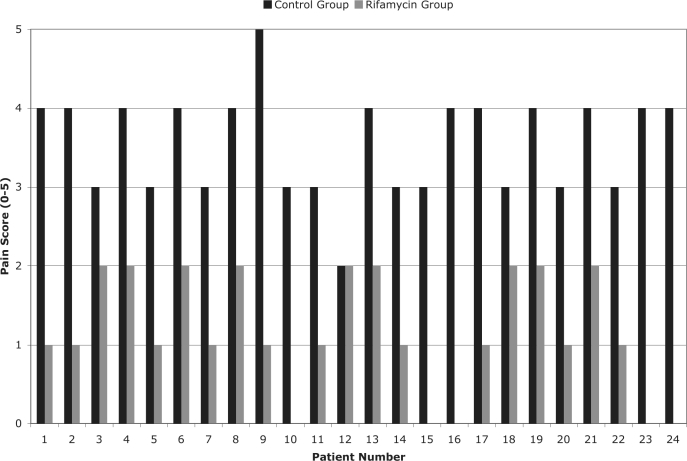
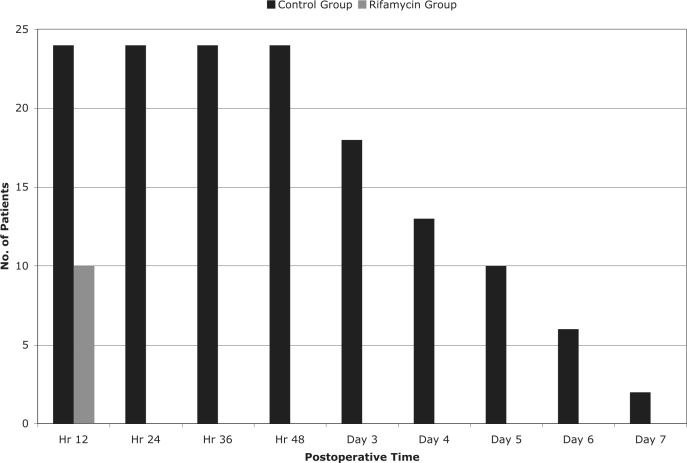
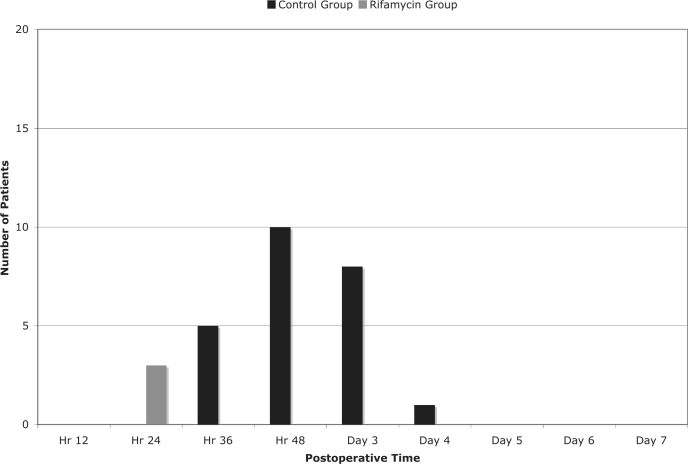
In histogram one (Figure 1), the mean values of the postoperative observations of pain localized in the umbilical region in patients in both groups are reported (P<0.001). In histogram 2 (Figure 2), the number of patients in both groups that required added analgesic drug administration (yes or not) was reported (P<0.005). Histogram 3 (Figure 3) depicts the mean values (on a scale of 0 to 5) of local signs of inflammation (wound warmness, hyperemia, umbilical wound swelling) in the umbilical region in the patients of both groups are reported (P<0.001). Histogram 4 (Figure 4) depicts the number of patients in both groups who suffered purulent leakage through the umbilical wound (yes or not) (P<0.005). Histogram 5 (Figure 5) depicts the number of patients in both groups who had dehiscence of the umbilical skin sutures (yes or no) (P<0.001).
Figure 1.
Umbilical region pain (N=24).
Figure 2.
Use of analgesics (N=24).
Figure 3.
Signs of phlogosis of the umbilical wound (N=24).
Figure 4.
Umbilical wound leakage (N=24).
Figure 5.
Umbilical skin suture dehiscence (N=24).
Clinical data were registered at 12, 24, 36, and 48 hours after the VLC and also on the third, fourth, fifth, sixth, and seventh post-VLC day; for the patients dismissed before the third postoperative day, there was an ambulatory outpatient control.
Sixty days after VLC, 2 cases of incisional umbilical hernias were reported in the control group.
The mean postoperative stay was 3 days in the rifamycin group (range, 1 to 8), and 4 days in the control group (range, 3 to 8).
DISCUSSION
Omphalitis is a minor postoperative complication after VLC. It is treated quite simply as an outpatient problem, but omphalitis represents discomfort for the patient, and it can cause a delay in the resumption of work. But, above all, omphalitis is a risk factor for the development of incisional umbilical hernia, which may occur in greater than 1% of cases.6
Postoperative umbilical port-site infection after VLC is a factor in the morbidity of this procedure, as it requires twice as much outpatient observation and treatment.
The occurrence of problems that were statistically significant (P<0.001) included referred pain of the umbilical region, local development of the classical signs of inflammation (rubor, tumor, calor, and others), and dehiscence of the cutaneous suture.
Our results show that in patients treated with rifamycin, umbilical port-site infections occurred less often than in the control group. Even analgesic usage and purulent secretion from the umbilical wound were statistically different (P<0.005) between the study group and the control group.
On the whole, a graphic representation of the results depicts a statistically significant difference between the 2 groups of patients, in favor of the rifamycin group. Topical prophylactic antibiotic therapy reduces omphalitis.
Moreover, control of the umbilical port-site infections is a relevant element in the patients with metabolic diseases and/or with alterations of the immune system, because they are frequently exposed to infections.
Systemic prophylactic antibiotic therapy in VLC maintains its usual role.7,8 Topical antibiotic prophylaxis was efficacious in reducing infections, but its use is not meant to replace systemic antibiotic prophylaxis. Rather, its use is to serve as an adjunct to systemic antibiotic prophylaxis so that the usual antibiotic protocol is not changed (ie, short-and ultra short-term antibiotic therapy).
The main result of this study is that umbilical port-site infections can be reduced by the topical use of rifamycin. In addition, patient comfort was enhanced in the rifamycin group compared with the control group.
Patients in the rifamycin group had minor postoperative morbidity caused by the presence of omphalitis, shorter postoperative stay, and almost no need of outpatient ambulatory medications.
The cost of the use of rifamycin in the pre-, intra-, and post-VLC period is surely less than is required for the ambulatory treatment of a postoperative wound infection.
The reduction of omphalitis with topical prophylactic antibiotic therapy is cost effective. Patients can resume work sooner, and ambulatory management requires less commitment in terms of human resources (physicians, nurses) and medical materials.
The literature reports the use of several methods to reduce the incidence of post-VLC umbilical port-site infections, such as specimen removal by means of an endo-bag,7 but in no study is the topical utilization of an antibiotic (like rifamycin) described during the pre-, intra-, and post-VLC periods.
The advantages derived from the use of rifamycin are significant, even if they are for a minor postoperative complication.
CONCLUSION
In this study, we examined a simple, economic way to treat the umbilicus to significantly reduce the incidence of post-VLC omphalitis. The data gathered showed positive and statistically significant results in favor of the rifamycin group. The series of patients, however, was limited and further studies are encouraged. Based on the above, use of topical rifamycin on the umbilicus is proposed as a rapid, safe, and economic way to reduce postoperative morbidity following VLC.
References:
- 1.Hamzaoglu I, Baca HB, Boler DE, Polat E, Ozer Y. Is umbilical flora responsible for wound infection after laparoscopic surgery? Surg Laparosc Endosc Percutan Tech 2004;14(5):263–267 [DOI] [PubMed] [Google Scholar]
- 2.Voitk AJ, Tsao SGS. The umbilicus in laparoscopic Surgery. Surg Endosc. 2001;15(8):878–881 [DOI] [PubMed] [Google Scholar]
- 3.Neri V, Ambrosi A, Di Lauro G, Fersini A, Valentino TP. Difficult cholecystectomies: validity of the laparoscopic approach. JSLS. 2003;7(4):329–333 [PMC free article] [PubMed] [Google Scholar]
- 4.Molloy D, Kaloo PD, Cooper M, Nguyen TV. Laparoscopic entry: a literature review and analysis of techniques and complications of primary port entry. Aust N Z J Obstet Gynaecol. 2002;42(3):246. [DOI] [PubMed] [Google Scholar]
- 5.Australian Safety and Efficacy Register of New Interventional Procedures–Surgical. Consumer Summary: Methods Used to Establish Laparoscopic Pneumoperitoneum (Adapted from the Report of the Review Group for Consumer Use by Ms. E. Ahern) Melbourne Australia: Royal Australian College of Surgeons; March 2002 [Google Scholar]
- 6.Coda A, Bossotti M, Ferri F, et al. Incisional hernia and fascial defect following laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2000;10(1):34–38 [PubMed] [Google Scholar]
- 7.Colizza S, Rossi S, Picardi B, et al. Surgical infections after laparoscopic cholecystectomy: ceftriaxone vs ceftazidime antibiotic prophylaxis. A prospective study. Chir Ital. 2004;56(3):397–402 [PubMed] [Google Scholar]
- 8.Harling R, Moorjani N, Perry C, MacGowan AP, Thompson MH. A prospective, randomised trial of prophylactic antibiotics versus bag extraction in the prophylaxis of wound infection in laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2000;82(6):408–410 [PMC free article] [PubMed] [Google Scholar]