Abstract
Background and objectives:
Trocar-site incisional hernia following laparoscopic ventral hernia repair is reported to have a relatively high incidence. The main reasons are trocar diameter and design, pre-existing fascial defects, and some operation- and patient-related factors. The aim of this article to show a new technique of ventral hernia repair that could prevent trocar site incisional hernia.
Methods:
After establishing the pneumoperitoneum, three 5-mm ports are inserted in positions according to the site and size of the hernia. The procedure begins by dissection of the adhesions of bowel loops or omentum (if any) from the hernia to clear a good margin for mesh coverage. Then a single 10-mm to 15-mm port (mesh insertion port) is inserted in the center of the ventral hernia depending on the size of the mesh. The mesh is fixed in position with a 5-mm tacker. The peritoneum and underlying superficial fascia are carefully closed before closing the skin.
Results:
A total of 35 patients were recruited for this method. The mean hospital stay was 1.5 days, the mean age was 50.35 years and the mean operative time was 40 minutes. In all patients, 10x15-cm ePTFE was used. No single incidence of trocar-site incisional hernia occurred during a mean follow-up of 2 years. Three (8.57%) patients developed complications and no mortality was reported.
Conclusion:
The mesh introduction through the port, which is situated at the center of the hernia defect is a simple, cost-effective technique and will prevent trocar-site incisional hernia.
Keywords: Trocar site incisional hernia, TSIH, Laparoscopic ventral hernia repair, LVHR
INTRODUCTION
With advancements in minimal access surgery, it is now feasible to repair ventral hernias with less pain, shorter hospital stay, earlier recovery, and fewer complications. The mesh is fixed in a sublay position overlying the hernia edges. In this article, we describe a new technique for performing laparoscopic ventral hernia repair. The main reason for adopting this technique was to prevent trocar-site incisional hernia, which is reported in the literature to have a relatively high occurrence rate. Other reasons are to simplify the method of ventral hernia repair and to shorten the time of the procedure. Furthermore, adopting this technique will reduce the number of operations required to repair trocar-site incisional hernias in the future. Finally, we have the advantage of sealing the incisional hernia without causing further weakness to the abdominal wall. Thus, we made advantageous use of the defect and eliminated the complication caused by placing a larger port outside the hernia defect.
METHODS
One consultant surgeon performed all procedures. The technique used is as follows. Preoperative skin marking of the hernia edge and the center are performed. The patient is placed in a supine position, and the operative site is prepared and drapped. Pneumoperitoneum is established with a Veress needle or an EXCBC port, or both Veress needle and EXCBC port as required. Three 5-mm ports that accommodate the working instruments and the telescope are inserted in positions according to the site and size of the hernia. The procedure begins by dissection of the adhesions of bowel loops or omentum (if any) from the hernia to clear a good margin for mesh coverage (Figure 1). Usually harmonic dissection is performed, but sharp scissors dissection is performed also in patients who have bowel adhesions. Then a single 10-mm to 15-mm port (mesh insertion port) is inserted in the center of the ventral hernia depending on the size of the mesh (Figures 2 and 3). Introduction of the port is very easy because at that location (center of the hernia), there is only skin, subcutaneous tissue, and peritoneum, while the fascial and muscle layers are usually attenuated. A single stitch is fixed to the center of the mesh before its introduction into the peritoneal cavity (Figure 4). A grasping instrument is introduced through this port to grab and pull the stitch thus easing fitness and centralization of the mesh over the hernia defect. The mesh is fixed in position with a 5-mm tacker (Figure 5). No transfascial stiches are used. We recommend closing the peritoneum and underlying superficial fascia carefully before closing the skin, as this will provide an extra barrier to infection.
Figure 1.
Ventral hernia.
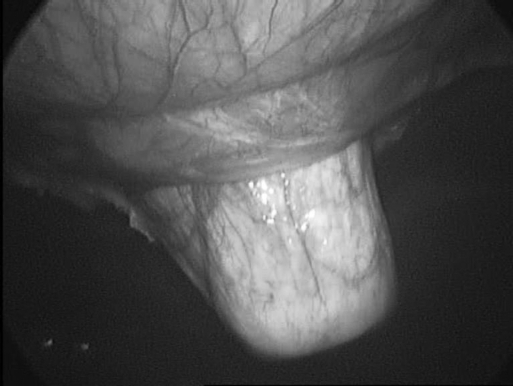
Figure 2.
Port insertion through the hernia defect.
Figure 3.
Mesh insertion.
Figure 4.
Mesh inside, the suture helps to fit the mesh to the defect.
Figure 5.
Mesh is fixed in position.
RESULTS
This method was used in a consecutive series of 35 patients. Nineteen men (54.28%) and 16 women (45.71%) were included in this study. The mean hospital stay was 1.5 days (range, 1 to 5). The mean age was 50.35 years (range, 41 to 80). The mean operative time was 40 minutes (range, 30 to 75). In all patients, 10x15-cm ePTFE was used. No single incidence of trocar-site incisional hernia occurred during a mean follow-up of 2 years (range, 5 months to 30 months). Three (8.57%) patients developed complications. Two patients (5.71%) developed abdominal pain, tenderness, and vomiting. One patient underwent diagnostic laparoscopy, which was normal. The other patient underwent computed tomography and no abnormalities were found. Both patients recovered with conservative management. We think that the cause of these symptoms could be bowel adhesions. The third patient developed early bowel obstruction due to adhesion and was managed laparoscopically. None of our patients died.
DISCUSSION
Laparoscopic ventral hernia repair (LVHR) has proved superior to open repair with all the advantages of the laparoscopic approach.1–4 It provides shorter hospital stay, earlier recovery, lower recurrence rate, and is cost effective. However, one of the problems with LVHR is trocar-site incisional hernia (TSIH), which is a known preventable complication following laparoscopic surgery. Its incidence is variable, but many studies report an incidence between 1% and 6%.5,6 The incidence following LVHR however is 1% to 2.6%.7,8 TSIH following LVHR could develop at the open introduction of the port, the mesh insertion port, or any other working instrument ports. The majority of studies report an incidence of less than 3%, which is considered an acceptable rate, especially if compared with open repair and its morbidity.9 A higher incidence rate of TSIH was also confirmed in the literature. Boldó et al10 reported an incidence of 22% (6 patients) in a series of 27 LVHR.
The risk factors for development of TSIH are trocar diameter, trocar design, pre-existing fascial defects, and some operation- and patient-related factors8 in addition to the direction of the port insertion, use of a drain, and the site of the port.
Specifically, changing from the traditional technique to our new technique can prevent TSIH after LVHR. Our method provides an easy, simple method of mesh insertion, which we recommend be done through a port, which is centralized over the hernia defect. By this method, the likelihood of TSIH will be negligible because the recurrence if any will be the recurrence of the original hernia, as this site will be supported by the mesh. In certain patients, the size of the hernia required a larger size of mesh or insertion of 2 (15x10 cm) meshes. Subsequently, careful anatomical closure of the port is performed to provide an extra barrier to infection and to maintain the pneumoperitoneum to complete the procedure.
One of the main concerns with this technique is the possibility of infection because the incision is directly over the mesh. Only one patient developed mesh infection and was treated successfully without mesh removal. The length of follow-up of patients is the inherent weakness of hernia repair studies. In all 35 operations we have performed, no single case of TSIH was reported during the follow-up period. This was including 5-mm ports, although TSIH can develop at this small port site.11
CONCLUSION
The new technique of mesh introduction through the port, which is situated at the center of the hernia defect, will prevent trocar-site incisional hernia. It is a simple and cost-effective technique because it reduces the number of operations for trocar-site incisional hernia.
References:
- 1.Heniford BT, Ramshaw BJ. Laparoscopic ventral hernia repair: a report of 100 consecutive cases. Surg Endosc. 2000;14(5):419–423 [DOI] [PubMed] [Google Scholar]
- 2.Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM. Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc. 2007;21(3):378–386 [DOI] [PubMed] [Google Scholar]
- 3.McGreevy JM, Goodney PP, Birkmeyer CM, Finlayson SR, Laycock WS, Birkmeyer JD. A prospective study comparing the complication rates between laparoscopic and open ventral hernia repairs. Surg Endosc. 2003;17(11):1778–1780 [DOI] [PubMed] [Google Scholar]
- 4.Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years' experience with 850 consecutive hernias. Ann Surg. 2003;238(3):391–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Lorenzo N, Coscarella G, Lirosi F, Gaspari A. Port-site closure: a new problem, an old device, JSLS. 2002;6(2):181–183 [PMC free article] [PubMed] [Google Scholar]
- 6.Di Lorenzo N, Coscarella G, Lirosi F, Pietrantuono M, Sus-anna F, Gaspari A. Trocars and hernias: a simple, cheap remedy. Chir Ital. 2005;57(1):87–90 [PubMed] [Google Scholar]
- 7.Berger D, Bientzle M, Muller A. Postoperative complications after laparoscopic incisional hernia repair. Incidence and treatment. Surg Endosc. 2002;16:1720–1723 [DOI] [PubMed] [Google Scholar]
- 8.Sanchez LJ, Bencini L, Moretti R. Recurrences after laparoscopic ventral hernia repair: results and critical review. Hernia. 2004;8:138–143 [DOI] [PubMed] [Google Scholar]
- 9.Immè A, Cardì F. Incisional hernia at the trocar site in laparoscopic surgery [in Italian]. Chir Ital. 2006;58(5):605–609 [PubMed] [Google Scholar]
- 10.Boldó E, Perez de Lucia G, Aracil JP, et al. Armelles trocar site hernia after laparoscopic ventral hernia repair. Surg Endosc. 2007;21:798–800 [DOI] [PubMed] [Google Scholar]
- 11.Holzinger F, Klaiber C. Trocar site hernias. A rare but potentially dangerous complication of laparoscopic surgery. Chirurg. 2002;73(9):899–904 [DOI] [PubMed] [Google Scholar]