Abstract
Background and Objectives:
Mesh fixation in laparoscopic ventral hernia repair typically involves the use of tacks, transabdominal permanent sutures, or both of these. We compared postoperative pain after repair with either of these 2 methods.
Methods:
Patients undergoing laparoscopic ventral hernia repair at the Mount Sinai Medical Center were prospectively enrolled in the study. They were sorted into 2 groups (1) those undergoing hernia repairs consisting primarily of transabdominal suture fixation and (2) those undergoing hernia repairs consisting primarily of tack fixation. The patients were not randomized. The technique of surgical repair was based on surgeon preference. A telephone survey was used to follow-up at 1 week, 1 month, and 2 months postoperatively.
Results:
From 2004 through 2005, 50 patients were enrolled in the study. Twenty-nine had hernia repair primarily with transabdominal sutures, and 21 had repair primarily with tacks. Both groups had similar average age, BMI, hernia defect size, operative time, and postoperative length of stay. Pain scores at 1 week, 1 month, and 2 months were similar. Both groups also had similar times to return to work and need for narcotic pain medication.
Conclusions:
Patients undergoing laparoscopic ventral hernia repair with primarily transabdominal sutures or tacks experience similar postoperative pain. The choice of either of these fixation methods during surgery should not be based on risk of postoperative pain.
Keywords: Laparoscopic ventral hernia repair, Incisional hernia, Mesh, Fixation
INTRODUCTION
Laparoscopic ventral hernia repair has grown in popularity since it was first reported in the early 1990s. Numerous studies have found it to have many advantages over traditional open repair.1–3 Lower recurrence rates, fewer complications, and shorter hospital stays have led some to believe that it sets the new standard of care for ventral hernia repair.1,2 Controversy exists regarding the optimal method to fix the prosthetic mesh to the anterior abdominal wall. Currently, the 2 most popular methods of mesh fixation are via transabdominal sutures and laparoscopic tacks. Sutures pass through all layers of the fascia and muscle of the anterior abdominal wall, while tacks secure the mesh to the innermost millimeters of the peritoneal cavity.
Most controversy in laparoscopic repair centers on the tensile strength of the mesh fixation method. Recurrence is thought to be the result of inadequate or failed fixation. Postoperative pain produced by the securing methods is another consideration in deciding between sutures and tacks. Sutures are felt to cause worse and more persistent pain.3,4 However, no comparative studies investigate which method truly causes more discomfort. This study compares these 2 methods and examines the consequential pain that occurs after each type of fixation.
METHODS
From 2004 through 2006, patients undergoing laparoscopic ventral hernia repair by 8 different surgeons at the Mount Sinai Medical Center were prospectively enrolled in the study. Patients undergoing other simultaneous procedures were excluded. The patients were sorted into 2 groups1: those undergoing hernia repairs primarily with transabdominal sutures (Sutures Group) and2 those undergoing hernia repairs primarily with tacks (Tacks Group). Patients in the Sutures Group had repairs with transabdominal sutures placed circumferentially approximately 2 cm to 3 cm apart. These patients typically had 10 to 20 sutures placed, depending on the size of hernia. Patients in the Tacks Group included those with hernias completely repaired with only tacks and repairs that may have involved 4 stay sutures with the rest of the mesh secured to the anterior abdominal wall with tacks. The patients were not randomized into these groups. Choice of repair was made by surgeon preference, including type of mesh and type of tacks.
Patients' demographics and clinical data were prospectively recorded. Telephone follow-up was used to determine verbal pain scores at 1 week, 1 month, and 2 to 3 months postoperatively (0=pain free, 10=excruciating pain/worse pain ever). In addition, patients were asked regarding time to return to work and need for narcotic pain medications. Informed consent was obtained, and this study was approved by the institutional review board. We needed to enroll 50 patients into the study to detect a 50% difference in pain scores (Power 80%, Level of significance P=0.05).
RESULTS
Fifty patients were enrolled in this study. Twenty-nine were in the Sutures Group and 21 in the Tacks Group. Demographics and clinical characteristics of the 2 groups are outlined in Table 1. Both groups were of similar age and body mass index (BMI). More females were in the Sutures Group. No significant difference was found between the groups in terms of proportion of patients with recurrent hernias, multiple hernia defects, and total defect size. The type of mesh used was surgeon dependant and was variable across both groups.
Table 1.
Demographics and Hernia Characteristics
| Sutures (n = 29) | Tacks (n = 21) | |
|---|---|---|
| Age | 52 | 57 |
| M/F | 11/18 | 4/17 |
| BMI (kg/m2) | 31.3 | 27.4 |
| Recurrent | 5 (17%) | 5 (24%) |
| Multiple Defects | 8 (28%) | 6 (29%) |
| Mean Defect Size (cm2) | 106 | 81 |
| Mesh Type | 12 Composix EX | 15 Composix EX |
| 15 Dualmesh | 5 Parietex | |
| 1 Dulex | 1 Dualmesh | |
| 1 Parietex |
Table 2 shows the operative and postoperative characteristics of the 2 groups. Both groups were similar in operative time. The Tacks Group had a longer length of postoperative hospital stay (2.4 vs 1.7 days); however, this difference was not statistically significant. There was no early recurrence during the follow-up period. The Tacks Group had a higher morbidity rate (19% vs 4%). The most common complications between the 2 groups were pneumonia and urinary retention.
Table 2.
Operative and Postoperative Characteristics
| Sutures (n = 29) | Tacks (n = 21) | P | |
|---|---|---|---|
| Operative Time (min) | 132 | 122 | p > 0.05* |
| Length of Stay (days) | 1.7 | 2.4 | p > 0.05* |
| Early Recurrence | 0 | 0 | |
| Morbidity | 1 (3%) Pneumonia | 4 (19%) | |
| Urinary Retention: 2 | |||
| Pulmonary Embolism: 1 | |||
| Pneumonia: 1 |
Differences between groups were determined by two tailed Student's t-tests.
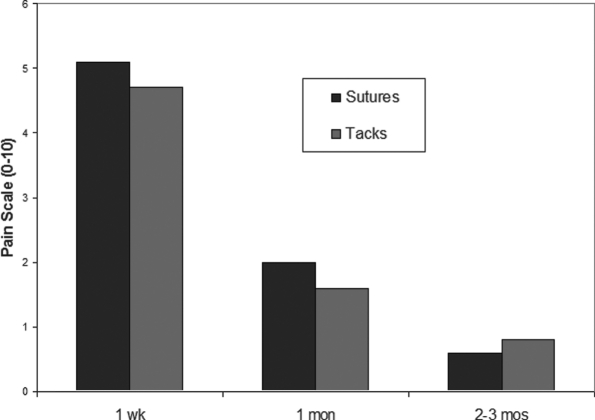
Verbal pain scores as reported via telephone interview are shown in Figure 1. No difference was reported in mean pain scores between the 2 groups at 1 week, 1 month, and 3 months (P>0.05). On a scale of 0 to 10, patients from both groups had moderate pain 1 week after the operation. Pain scores in both groups decreased at 1 month and were minimal by 2 to 3 months. In addition, use of narcotic pain medications during the postoperative period was similar in both groups (Table 3). A similar proportion of both groups required such pain medications at 1 week. Time to return to work was also similar between the groups. No patients required local anesthetic injection for chronic, persistent pain in either group.
Figure 1.
Mean postoperative pain scores at 1 week, 1 month, and 2 to 3 months after laparoscopic ventral hernia repair. No difference in pain score existed between groups (P>0.05, 2-tailed Student t test).
Table 3.
Postoperative Pain Assessment
| Sutures (n = 29) | Tacks (n = 21) | |
|---|---|---|
| Narcotic Pain Meds > 1 wk | 12 (41%) | 8 (38%) |
| Return to Work by 1 wk | 10/20 (50%) | 5/12 (42%) |
DISCUSSION
The preferred method of mesh fixation during laparoscopic ventral hernia is controversial. Many proponents of the use of transabdominal sutures cite lower recurrence rates due to higher tensile holding strengths of sutures in comparison to tacks.5,6 Other authors6–8 argue that the use of tacks reduces surgical time considerably while maintaining similar recurrence rates. These authors also argue that the use of tacks significantly reduces postoperative pain. To date, most studies of mesh fixation during laparoscopic ventral hernia repair focus on the risk of recurrence. However, this is the only study that compares postoperative pain after hernia repair with sutures versus tacks.
Anecdotally, pain is generally worse after repair with sutures than with tacks. Sutures penetrate through the full thickness of abdominal wall musculature and fascia. This has been theorized to cause local muscle ischemia resulting in severe pain postoperatively.7 In addition, numerous sutures are typically needed around the perimeter of the hernia defect. Because mesh overlap on normal muscular fascia is usually aimed for around 3 cm to 5 cm, the circumference around which sutures must be secured becomes quite large. We found no difference in postoperative pain in patients undergoing hernia repair with sutures or tacks. Both groups had moderate pain at one week and minimal pain on further follow-up. It is possible that early pain caused by multiple tacks penetrating the parietal peritoneum is equivalent to the pain caused by transfascial sutures. In the long-term, both repairs seem to level off in terms of discomfort.
Cobb et al12 has also proposed that intercostal nerves may become entrapped within the transabdominal sutures causing chronic, persistent neuropathic pain. Series of repairs using transfascial sutures report persistent pain and discomfort in 1% to 6% of patients.1–3,8,9 Most authors feel oral anti-inflammatory medications or injections of a local anesthetic can alleviate the symptoms in the majority of cases.1,3,10,11 Others have reported re-explorations for persistent pain, finding immediate relief after the release of a suture from the site of symptoms.12 None of the patients in our study had persistent pain severe enough to undergo local anesthetic injection or reoperation. The reports of persistent cases of pain seem to be isolated at one particular suture site, supporting the nerve entrapment theory. Pain from muscle ischemia would seem to be more generalized at all of the suture sites. Our data suggest that both methods of mesh fixation are generally not different in terms of their resultant postoperative pain. However, because our study only included 50 patients, occasional episodes of chronic persistent pain due to nerve entrapment are certainly possible if more patients were followed. Our findings are somewhat consistent with those of LeBlanc et al,17 whose study noted that patients in the earlier half of their series had more pain. These patients had fewer sutures used, suggesting the use of these sutures was unrelated to postoperative pain.
Though the use of laparoscopic tackers may seem to be simpler and faster, we did not find a significant difference in operative time between the 2 fixation methods. This is contrary to the general opinion that the use of tacks reduces surgical time.1,4 Operative time during laparoscopic ventral hernia repair significantly involves extensive adhesiolysis and dissection of peritoneal contents from the anterior abdominal wall. Conceivably, surgeons may misinterpret the amount of time spent on the different phases of the operation and focus on time spent on mesh fixation. In our study, we did not specifically look at operative time during different components of the operation. Moreover, no other prospective studies compare operative time in laparoscopic ventral hernia repair. Therefore, the assumption that repair with transabdominal sutures takes longer than tack repair remains largely unproven.
The limitations of this study center on the sample size. Fifty patients were followed, and comparisons were made between the 2 groups. Small differences in pain scale between the groups may be difficult to assess. However, large differences should be found. Considering that most anecdotal evidence suggests a large difference in pain experience, we feel our conclusions are still valid. In addition, although data were prospectively recorded, the patients in this study were not randomized to treatment arms. The type of repair was based on surgeon preference, as each had his or her own strong feeling regarding the best method of fixation. Larger controlled trials may be necessary to optimally determine which method contributes to the most pain.
CONCLUSION
Patients undergoing laparoscopic ventral hernia repair with primarily transabdominal sutures or tacks experience similar overall postoperative pain. Symptoms are moderate by the end of the first postoperative week and mild by 1 month. Occasional episodes of chronic, persistent suture site pain are possible and have been reported. Postoperative pain should be a minor factor when deciding between repair with sutures or tacks in laparoscopic ventral hernia repair.
Acknowledgments
The authors wish to thank Anthony J. Vine, MD, Brian P. Jacob, MD, Subhash Kini, MD, and David Pertsemlidis, MD, at the Mount Sinai School of Medicine for assisting in recruiting their patients for this study.
References:
- 1.McGreevy JM, Goodney PP, Birkmeyer CM, Finlayson SRG, Laycock WS, Birkmeyer JD. A prospective study comparing the complication rates between laparoscopic and open ventral hernia repairs. Surg Endosc. 2003;17:1778–1780 [DOI] [PubMed] [Google Scholar]
- 2.DeMaria EJ, Moss JM, Sugerman HJ. Laparoscopic intraperitoneal polytetrafluoroethylene (PTFE) prosthetic patch repair of ventral hernia. Surg Endosc. 2000;14:326–329 [DOI] [PubMed] [Google Scholar]
- 3.Carbajo MA, Martin del Olmo JC, Blanco JI, et al. Laparoscopic treatment vs open surgery in the solution of major incisional and abdominal wall hernias with mesh. Surg Endosc. 1999;13:250–252 [DOI] [PubMed] [Google Scholar]
- 4.Heniford B, Park A, Ramshaw BJ, Voller G. Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg. 2000;190:645–650 [DOI] [PubMed] [Google Scholar]
- 5.Eid GM, Prince JM, Mattar SG, Hamad G, Ikrammudin SI, Schauer PR. Medium-term follow-up confirms the safety and durability of laparoscopic ventral hernia repair with PTFE. Surgery. 2003;143:599–604 [DOI] [PubMed] [Google Scholar]
- 6.Carbajo MA, Martin del Olmo JC, Blanco JI, et al. Laparoscopic approach to incisional hernia. Lessons learned from 270 patients over 8 years. Surg Endosc. 2003;17:118–122 [DOI] [PubMed] [Google Scholar]
- 7.Gillian GK, Geis WP, Grover G. Laparoscopic incisional and ventral hernia repair (LIVH): an evolving outpatient technique. JSLS. 2002;6:315–322 [PMC free article] [PubMed] [Google Scholar]
- 8.Berger D, Bientzle M, Muller A. Postoperative complications after laparoscopic incisional hernia repair. Surg Endosc. 2002;16:1720–1723 [DOI] [PubMed] [Google Scholar]
- 9.Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias. Nine years' experience with 850 consecutive hernias. Ann Surg. 2003;238:391–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van't Riet M, van Steenwijk PJ, Kleinrensink GJ, Steyerberg EW, Bonjer HJ. Tensile strength of mesh fixation methods in laparoscopic incisional hernia repair. Surg Endosc. 2002;16:1713–1716 [DOI] [PubMed] [Google Scholar]
- 11.Franklin ME, Gonzalez JJ, Jr, Glass JL, Manjarrez A. Laparoscopic ventral and incisional hernia repair: An 11-year experience. Hernia. 2004;8:23–27 [DOI] [PubMed] [Google Scholar]
- 12.Cobb WS, Kercher KW, Heniford BT. Laparoscopic repair of incisional hernias. Surg Clin N Am. 2005;85:91–103 [DOI] [PubMed] [Google Scholar]
- 13.Parker HH, 3rd, Nottingham JM, Byone RP, Yost MJ. Laparoscopic repair of large incisional hernias. Am Surg. 2002;68:530–533 [PubMed] [Google Scholar]
- 14.Reitter DR, Paulsen JK, Debord JR, Estes NC. Five-year experience with the “four-before” laparoscopic ventral hernia repair. Am Surg. 2002;66:465–468 [PubMed] [Google Scholar]
- 15.LeBlanc KA, Whitaker JM. Management of chronic postoperative pain following incisional hernia repair with Composix mesh: a report of two cases. Hernia. 2002;6:194–197 [DOI] [PubMed] [Google Scholar]
- 16.Carbonell AM, Harold KL, Mahmutovic AJ, et al. Local injection for the treatment of suture site pain after laparoscopic ventral hernia repair. Am Surg. 2003;69:688–691 [PubMed] [Google Scholar]
- 17.LeBlanc KA, Whitaker JM, Bellanger DE, Rhynes VK. Laparoscopic incisional and ventral hernioplasty: lessons learned from 200 patients. Hernia. 2003;7:118–124 [DOI] [PubMed] [Google Scholar]