Abstract
Background:
The purpose of this study was to analyse the surgical techniques, perioperative complications, and recurrence rate of laparocopic ventral hernia repair (LVHR), in comparison with the open ventral hernia repair (OVHR), based on the international literature.
Methods:
A Medline search of the English literature was performed using the term “laparoscopic ventral hernia repair.” Further articles were found by cross-referencing the references of each main article.
Results:
Current literature on the topic suggests that LVHR is a safe alternative to the open method with the main advantages being minimal postoperative pain, a shorter convalescence period, and better cosmetic results. Main complications after the laparoscopic approach, such as incidental enterotomy, protracted pain, postoperative seroma, or mesh infection occur at an acceptable rate. Furthermore, most articles favor LVHR versus OVHR in terms of recurrence rate.
Conclusions:
Although further randomized studies are needed to draw safe conclusions in terms of complications and recurrence, LVHR is fast becoming the standard approach in the repair of abdominal wall hernias.
Keywords: Hernia, Laparoscopy, Open, Ventral, Incisional
INTRODUCTION
Incisional hernia is a common long-term complication of abdominal surgery and is estimated to occur in 3% to 13% of laparotomy incisions.1 However, its incidence is greater than 23% in patients who have developed an infection in the laparotomy wound.2,3 Approximately 50% of incisional hernias develop within the first 2 years after the primary operation, and 74% develop after 3 years.4,5 Approximately more than 100,000 men, women, and children in the USA undergo surgery for ventral hernia repair each year.6,7 The recurrence rate of incisional hernia, after primary closure is high, ranging between 10% and 50%, and has been reduced to 3% to 18% after the introduction of prosthetic materials (meshes) in hernia repair.1,8,9 Nevertheless, open hernia repair can be a major operation with considerable morbidity due to mesh-related infections. An increasing interest in laparoscopic surgery and the availability of new materials have encouraged the adoption of laparoscopic techniques in ventral hernia repair. Laparoscopic ventral hernia repair (LVHR) was introduced into surgical practice by LeBlanc and Booth in 1991.10 It is based on the same physical and surgical principles as the open underlay procedure described by Stoppa,11 Rives,12 and Wantz.13 Surgeons and patients have rapidly accepted laparoscopic repair for incisional and primary ventral hernia over the past decade. LVHR is now being used with increasing frequency even for the management of patients with complex incisional hernias. With the use of the laparoscopic approach, large incisions and drain placement can be avoided, which leads to a reduction in postoperative wound-related problems.14,15 Recent reports on this topic have supported minimal postoperative morbidity, a shorter convalescence period, and an acceptable recurrence rate.16–18 Limiting factors in most studies include technical variations, limited sample size, and restricted follow-up.19,20
To date, more than 100 studies on LVHR have been published, although most of them are case series lacking control groups.21,22 Recently, several studies based on large numbers of patients have been accumulated due to increasing experience.23,24 Herein, we analyze the existing literature on LVHR, in an effort to examine the optimal surgical technique, complications, and long-term results in comparison with the open ventral hernia repair (OVHR).
PATHOGENESIS OF INCISIONAL HERNIA
Early postoperative development of incisional hernia implies an important role of perioperative factors, such as type of incision, suture technique, wound infection, or wound dehiscence.25,26 It is hypothesized that incisional hernias are caused by acute subclinical fascial separations in the early postoperative period.25 Several studies27 have compared different suture material, and it has been recommended that an absorbable suture be used for fascial closure, as it decreases the likelihood of infection and eventually dissolves, preventing a “saw-like” effect on the fascia, which may predispose to fascial disruption. However, more recently, 2 meta-analyses28,29 identified more incisional hernias after closure with absorbable sutures than with nonabsorbable sutures. Another meta-analysis performed by Van't Riet et al30 found no difference in incisional hernia development between slowly absorbable materials, such as PDS, and nonabsorbable sutures, such as nylon. In addition, nonabsorbable sutures were found to be associated with an increased incidence of prolonged wound pain and suture sinus formation; therefore, the use of slowly absorbable sutures should be considered in abdominal wound closure.
Late development of an incisional hernia implicates other mechanisms, such as advanced age, diabetes, malignancy, and connective tissue disorders.31 However, there is evidence that the abdominal wound can weaken over the course of years and give rise to an incisional hernia.32
Wound healing depends on a variety of cellular and molecular factors capable of inducing hemostasis, angiogenesis, inflammation, fibroplasias, and wound remodeling. One of the major extracellular proteins involved in wound healing is collagen, with 2 main types: type I and type III collagen. Type I collagen is found in fascia, bone, and skin, and has a high tensile strength. Type III collagen has a lower tensile strength but increased flexibility and is found in blood vessels, smooth muscle, and organ parenchyma. Early aponeurotic wound healing is based mainly on type III collagen, which provides the wound with little tensile strength. Therefore in the early phase, closure and healing of the aponeurosis depends largely on technical closure. However, fascial strength increases later as type I collagen increases and forms tight intermolecular links. It is believed that abnormalities in collagen synthesis may predispose to weak healing of the aponeurosis and progression to development of an incisional hernia.33,34 In an experimental study by Dubay et al,,35 a fibrablast growth factor (bFGF)-releasing rod was placed into the fascial wound and as a result a significant increase in type I collagen staining around the bFGF treated fascia was noted. This contributed to a considerable increase in the fascia-breaking strength, and as a consequence a significant reduction in primary and recurrent incisional hernia formation rate was observed.
Advances in analyzing the cellular and molecular mechanisms of the pathogenesis of incisional hernia will help in applying therapeutic agents to strengthen wound healing and prevent incisional hernia formation.
OPEN REPAIR TECHNIQUES
Traditional primary open repair is based on suture approximation of aponeurosis on each side of the hernia defect. However, recurrence rates after this procedure range from 41% to 52% in the long term.8,36 The introduction of prosthetic meshes in hernia repair has substantially helped in the reduction of recurrence rates. Indeed, Luijendijk et al8 demonstrated a significant reduction in recurrence rates between primary suture repair compared with mesh repair, 43% to 24%, respectively, for first-time incisional hernia repairs. However, the mesh repairs still require wide dissection of soft tissue, which contributes to an increased incidence of wound-related complications (more than 12%).17,37
Among the open repairs, the onlay technique, is the most widely used one. According to this technique, a polypropylene mesh is sutured onto the anterior rectus sheath.38 This technique is easy, convenient, but it has a considerable morbidity rate and recurrence rate (8% to 27%38–40).
Another repair option is the inlay technique, such that the mesh is sutured to the aponeurotic edges. This technique has been used to cover large aponeurotic gaps, and it carries extremely high recurrence rates.41,42 In the extra-peritoneal underlay technique, widely known as the Rives-Stoppa repair,11,12,43,44 the mesh is placed retromuscularly and anterior to the posterior rectus sheath, followed by primary closure of the anterior fascia. This technique requires limited soft tissue dissection; therefore, it carries acceptable morbidity and recurrence rates.8,41,42,45 Because there is no direct contact of mesh with the abdominal viscera, there is reduced risk of bowel obstruction, fistula formation, or both. Moreover, problems resulting from placement of the prosthesis in the subcutaneous space, such as seroma formation and wound infection, are also avoided.43,44
The intraperitoneal underlay technique was first described by McCarthy et al46 in 1981. At the beginning, they used polypropylene mesh, which was sutured to the peritoneal edge of the hernia sac. Polypropylene was gradually abandoned for intraperitoneal mesh fixation due to its trend to cause adhesions to bowel loops and was replaced by the polytetraflouoroethylene (ePTFE) mesh or bilayer polytetrafluoroethylene and polypropylene mesh in the more recent series.47 A recent study by Millikan et al47 with this technique using full-thickness transfascial sutures in 102 patients showed a 0% recurrence rate in a median follow-up of 28 months. Nevertheless, in the majority of studies analyzing the intraperitoneal underlay technique, the recurrence rate did not surpass 10%.43
Although the onlay technique seems to be the most popular due to its simplicity, it carries a higher morbidity rate than the other 3 techniques.41,42 In addition, Rudmik et al34 performed an extensive review of the articles referring to the main techniques used in open ventral hernia repair and calculated an overall 4.5%, 8%, 14%, and 48% recurrence rate for the intraperitoneal underlay repair, the extraperitoneal underlay repair, onlay repair, and inlay repair, respectively.
The relatively high morbidity and recurrence rates of the open repair techniques prompted the development of the laparoscopic approach in an effort to improve the clinical outcome.
LAPAROSCOPIC REPAIR
Since the introduction of the laparoscopic approach in ventral hernia repair by LeBlanc and Booth,10 the laparoscopic technique has gradually become increasingly popular worldwide, as it offers early recovery, decreased hospital stay, minimal morbidity, and low recurrence rates. Several comparative studies are now available to support these advantages of the laparoscopic approach.48,49
Technique
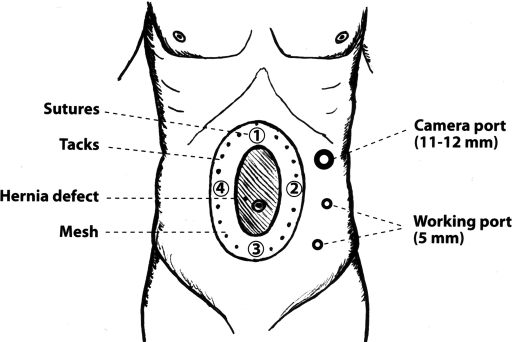
The laparoscopic technique has numerous variations of the methodology used by surgeons, although several common steps are followed by all. The procedure starts with entering the peritoneal cavity by using a Veress needle, an open Hasson method, or an optical trocar allowing view of the abdominal wall layers during penetration. Three trocars are used, one 10-mm trocar and two 5-mm, which are placed as laterally as possible on the abdominal wall, so they are at an adequate distance from the hernia orifice (Figure 1). Most of the operations are completed with 3 trocars.50 The next step of the operation is the most tedious part: adhesiolysis. The adhesions in the abdomen are lysed using electrocautery or an ultrasonic scalpel. No cauterization should be done that may injure the bowel wall. Perforation of the intestine is the most serious injury associated with laparoscopic ventral hernia repair.51
Figure 1.
Schematic presentation of a midline hernia defect, trocar sites, suture fixation of the mesh, and tack application points.
After adhesiolysis, the sac contents are gently reduced into the peritoneal cavity, while the peritoneal sac is left in situ. Closure of large hernia defects is recommended by Franklin et al52 with nonabsorbable sutures, even if only a limited closure is possible. This may be accomplished percutaneously with a suture passer by placing individual sutures. This practice may improve cosmesis and prevent undesireable complications, such as seroma formation.
The periphery of the hernia defect is evaluated by direct vision and palpation and is marked on the abdominal wall skin with a marker. The carbon dioxide should be released prior to measurement, revealing the true size of the hernia defect. The craniocaudal and lateral measurements are taken to define the size of the prosthetic mesh. The surgeon should add 6cm to these measurements in both directions, which provides a 3-cm overlap of the aponeurotic edges of the hernia by the mesh. Some surgeons suggest a 4-cm to 5-cm overlap, especially if the patient is morbidly obese, or if the hernia is recurrent or of large size.53 The size of mesh that most closely approaches this measurement is selected for the repair. Four main types of mesh have been used: polypropylene (Prolene, Ethicon, Sommerville, NJ, USA), expanded polytetrafluoroethylene (Dual mesh, Gore-Tex, Gore Medical, Flagstaff, AZ, USA), composite polypropylene+polytetrafluoroethylene (Composix, CR Bard, Cranston, NJ, USA), or composite polypropylene+collagen (Parietene, Sofradim, Trevoux, France). Polypropylene prosthesis has been abandoned in the laparoscopic approach, because it may create adhesions with bowel loops. It has been replaced by Proceed (Ethicon), which is composed of polypropylene covered with oxidized regenerated cellulose (ORC) (Table 1).51
Table 1.
The most popular prosthetic biomaterials available for incisional hernia repair
| Type of Biomaterial* | Product Name-Brand | Category According to Pore Size |
|---|---|---|
| Monofilament PPM | Marlex (Bard) | Macroporous (larger than 75 μm) |
| Double filament PPM | Prolene (Ethicon) | Macroporous |
| Monofilament PPM | Prolite (Atrium) | Macroporous |
| ePTFE mesh | Gore-Tex (Gore) | Microporous (less than 10 μm) |
| ePTFE mesh | Dulex (Bard) | Microporous |
| ePTFE mesh | DualMesh (Gore) | Microporous |
| Braided Dacron mesh | Mersilene (Ethicon) | Mix-prosthesis |
| Perforated PTFE patch | MicroMesh (Gore) | Mix-prosthesis |
| PPM + PDS + ORC | Proceed (Ethicon) | Mix-prosthesis |
| Braided PPM | Ultrapro (Ethicon) | Mix-prosthesis |
| PPM + ePTFE | Composix (Bard) | Mix-prosthesis |
| PPM + ePTFE | Ventralex (Bard) | Mix-prosthesis |
| PPM + Collagen | Parietene (Sofradim) | Mix-prosthesis |
| POL + Collagen | Parietex (Sofradim) | Mix-prosthesis |
| PPM + HA + CMC | Sepramesh (Genzyme) | Mix-prosthesis |
ePTFE = expanded polytetrafluoroethylene, PPM = polypropylene, POL = polyester, HA = hyalouronic acid, PDS = polydioxanone, ORC = oxidized regenerated cellulose, CMC = carboxymethyl cellulose.
The clinical experience with all these types of mesh varies from country to country. Gore-Tex (ePTFE) mesh has been widely used worldwide, but Composix has become more popular in the last few years. The collagen-based meshes have recently been added. All collagen meshes have been treated to eliminate all cells and proteins other than collagen, which may evoke adverse reactions to the host. The most popular of these meshes is Surgisis (Surgisis Gold, Cook Surgical, Bloomington, IL, USA), made of porcine small intestinal mucosa. These meshes are mainly used to reconstruct the abdominal wall in an infected field, but they are of limited use in laparoscopic ventral hernia repair.54
After selection of the appropriate-sized mesh, 4 to 6 sutures are placed on the edges of the prosthetic mesh. The suture sites are numbered with a marker to allow easier orientation of the prosthetic mesh in the abdominal cavity. The tailored prosthetic mesh is rolled tightly and inserted in the peritoneal cavity through the 10-mm to 11-mm trocar. It is unrolled inside the abdomen and spread under the defect. Two-mm skin incisions are made in the marked points on the abdominal wall. With the help of a Berci fascial closure instrument (KARL STORZ GmbH & Co. KG, Tuttlingen, Germany) or the Endoclose (Autosuture) inserted through each skin incision into the peritoneal cavity, the 2 ends of each suture are grasped and drawn outside through the skin incisions by separate passages and at different angles. The suture ends are tied down extracorporeally and buried subcutaneously. The mesh is further secured with 5-mm titanium tacks using Protack (AutoSuture, Norwalk, CT, USA), the EMS stapler (Ethicon), or the reusable Salute (CR Bard).50,51 The tacks are placed at the margins of the mesh at 1-cm intervals.
Advantages
LVHR achieves adequate closure of the hernia defect by using intraperitoneal mesh fixation with minimal soft-tissue dissection. The technique has all the advantages of the laparoscopic approach, such as less postoperative pain, earlier recovery, and a shorter convalescence period than the OVHR.55 Moreover, the patients feel more comfortable and tolerate oral intake earlier than after the open procedure. For patients undergoing laparoscopic repair of a primary ventral hernia, there is also a significant cosmetic advantage. However, for patients undergoing laparoscopic repair of an incisional hernia, the benefit in terms of body image is limited. LVHR also has significant technical advantages. With this approach, minimal fascial defects, known as “Swiss cheese” defects, which may be missed during the open repair, can be identified and closed with one mesh. In addition, by placing the mesh intraperitoneally, the intraabdominal pressure pushes upwards and holds the mesh into position.34 The major debate for this type of repair is which mesh fixation technique should be used, tacks plus transfascial sutures or tacks alone.
Mesh Fixation with Tacks and Sutures
A variety of reports are available on this type of mesh fixation, which represents the traditional technique in LVHR. Heniford et al,23 in a large series of 850 consecutive hernias, used an ePTFE mesh that was fixed on the abdominal wall with tacks and tranfascial ePTFE stitches in 97% of cases. Tacks alone were used to secure the mesh in several cases at the beginning of the study, but later this practice was discontinued. During a mean follow-up of 20.2 months, the hernia recurrence rate was 4.7%. LeBlanc et al56 have also suggested the importance of suture anchorage at 4-cm to 5-cm anchorage intervals around the perimeter of the mesh to minimize the risk for mesh migration. In another study, LeBlanc's group57 retrospectively compared 2 patient groups, one early and one late LVHR group, of 100 patients each. In a median follow-up of 36 months, the recurrence rate droped from 9% to 4%, which was attributed to the use of transfascial sutures and the increased mesh overlap in the more recent group.
Franklin et al54 published their 11-year experience in 384 patients who underwent LVHR using transfascial sutures. In a median follow-up of 47.1 months, the recurrence rate was 2.9%. Perrone et al58 recently reported their results in a group of 116 patients who had LVHR. In a median follow-up of 22 months, the recurrence rate was 9.3%. The majority of cases were performed with transfascial sutures; however, 35% of cases were performed with tacks alone. The 2 groups, ie, the transfascial suture group and the tack alone group, had similar recurrence rates, 9.2% and 8.5%, respectively. In a recent large review in LVHR by Cobb et al,59 a 3.8% overall recurrence rate was found, when transfascial sutures and tacks were used, compared with a 5.6% recurrence rate, when tacks only were used.
Mesh Fixation With Tacks Alone
Several studies have claimed the efficiency of tack-alone mesh fixation in LVHR. Frantzides et al60 followed up 208 patients for a median period of 24 months and reported a very low 1.4% recurrence rate. Bageacu et al61 studied a similar group of 159 patients for a median follow-up of 49 months. The recurrence rate was very high, 15.7%, and this was attributed by the authors to the learning curve effect: their recurrence rate decreased from 20% to 10% between the early (1993 to 1995) and the late period (1996 to 1998) of the study.
The largest study was performed by Carbajo et al62 who followed up 270 patients for a median period of 44 months. In this study, the recurrence rate was only 4.4%. In a Rudmik et al34 review of the related literature, the calculated recurrence rates after the suture and tack fixation technique and the tack fixation technique were approximately equal, 4.5% and 4.4%. Therefore, it seems that the fixation technique does not really affect the final outcome in LVHR, and that the laparoscopic repair yields very low recurrence rates. However, there is a general idea that tacks do not have the same holding strength as full-thickness abdominal sutures, and this is further supported by experimental evidence.63 Up to the present, no randomized prospective trial has compared the 2 fixation techniques, and therefore we cannot draw any safe conclusion in this matter.
Disadvantages-Complications
The laparoscopic approach in ventral hernia repair carries the risk of intestinal or bladder injury intraoperatively.23 Adhesions to the abdominal scar represent a significant problem during LVHR, with the risk of bowel injury around the neck of the hernia during dissection. Rudmik et al,34 in their review, calculated an overall risk of enterotomy of 2.1%. Injury of a hollow organ is a very serious event and should be recognized and treated immediately. An incidental enterotomy may occur during initial trocar placement or may result from adhesiolysis. This should be managed with endoscopic suturing if it is limited, whereas the procedure should be converted to open in case a more extensive laceration occurs of the small bowel or the colon, or if spillage of bowel contents occurs in the abdominal cavity.58 In the latter case, mesh repair of the ventral hernia should be postponed for a second stage. If the enterotomy remains unnoticed, it may result in an acute abdominal condition and sepsis within a few hours after surgery.
The main disadvantage of the laparoscopic approach is that the hernia sac is usually retained in place, which predisposes to postoperative seroma formation. The latter is a fluid collection inside the hernia sac, which develops in most cases. Actually, in a series, systematic ultrasound examinations detected seromas in 93% of patients postoperatively.64 Many of these cases are not noticed by the patient, and the majority resolve without intervention.23 However, some seromas persist for more than 8 weeks or cause symptoms requiring intervention, which is usually a sterile aspiration. The incidence of symptomatic seromas according to various reports ranges from 1% to 24%.23,34,61,62,65 According to the Carolina Medical Center's experience,23 only 2.6% of a large group of 860 patients with LVHR had seromas that persisted for more than 8 weeks or caused symptoms requiring intervention. Long-term complications, such as infection, do not usually develop from these fluid collections, regardless of whether they are aspirated early or allowed to persist for 8 weeks or longer. Seroma formation is a common problem after LVHR; however, its incidence is similar to that after OVHR.66 Despite the fact that no specific measures are available to prevent this complication, LeBlanc et al56 showed that applying a postoperative compressive bandage or wearing an abdominal binder for a couple of months after surgery may decrease clinically significant seroma formation.
In LVHR, the mesh comes into minimal contact with the patient's dermal flora while it is introduced intraperitone-ally. An adhesive tape on the skin may prevent potential contamination of the mesh. Minimal tissue dissection in the laparoscopic approach further reduces the risk of infection. Despite the potential benefit of a reduction in infectious complications from LVHR, still a percentage of patients, ranging from 0.7% to 5% in different series,23,58,67 may acquire infection related to the hernia repair. The overall calculated incidence of mesh infection is 0.6%, whereas the incidence of fistula formation is 0.1%.59 Trocar-site infection or cellulitis can be treated with antibiotics. Mesh infection may appear several weeks after surgery. Abscesses may form above or below the mesh. Infection is a devastating complication necessitating mesh removal in most cases.67 Mesh removal leaves a hernia defect and always leads to recurrence. Any associated abscesses should be drained percutaneously under computed tomography guidance, and the patient should receive systemic antimicrobial therapy.23 Prophylactic measures to reduce the risk of infection include efforts to minimize skin contamination at surgery, elimination of any potential sources of infection before surgery, limit the contact of mesh with the skin, and the use of antibiotic prophylaxis perioperatively.57
Protracted pain (more than 12 weeks) at the sites of the transfixing sutures on the abdominal wall is not uncommon (1.3% to 3.3%50,58,59). Patients with prolonged pain are initially treated with anti-iflammatory medications, or injections of local anesthetics. In case of persisitent pain, removal of the anchoring suture usually relieves the pain.58 In certain cases, however, there may be neuroma formation, which does not resolve after suture removal.
Prolonged ileus may develop in a minority of patients (3%) and should be treated expectantly, in-hospital, until patients can tolerate oral intake.23 In some patients, adhesions may form between the omentum or the intestines and the mesh at the tack sites, and this may predispose to intestinal obstruction. Exacerbation of chronic obstructive pulmonary disease may occur after the laparoscopic procedure, as a result of pneumoperitoneum. Cardiac complications may also occur in patients with preexisting cardiac disease, such as congestive cardiac failure, coronary artery disease, and other such things.
Patients with complications carry a higher risk of developing a hernia recurrence. Most recurrences occur after mesh removal for postoperative infection. Heniford et al23 found significant associations between recurrence and larger hernias, longer operative times, previous hernia repairs, morbid obesity, and higher complication rates. Sains et al66 performed an excellent meta-analysis of recent high-quality studies comparing LVHR with OVHR and they noted a trend towards lower hernia recurrence rates following the laparoscopic approach, though not achieving statistical significance. Pierce et al67 have presented a pooled data analysis of 45 published series in LVHR, representing 5340 patients (4582 LVHR, 758 OVHR). They demonstrated a significantly lower recurrence rate with LVHR for both the pooled (4.3%) and the paired (3.1%) study cohorts (studies comparing patients who had undergone LVHR or OVHR within a given institution), compared with OVHR series (12.1%, P<0.0001). Although recurrence still remains an important problem after LVHR, it does not surpass 5% to 10% in most series.34,68,69
CONCLUSIONS
Our review indicates that LVHR is a safe and effective approach to abdominal wall hernias. The technique offers the advantages of the laparoscopic approach, ie, a short hospital stay, less postoperative pain, and early convalescence. The procedure carries an acceptable risk of complications, a low risk of recurrence, and an excellent cosmetic result. However, larger, long-term multicenter studies comparing the laparoscopic with the open technique are needed to establish its efficacy. For the time being, it is considered a good alternative to its open counterpart, at least in experienced hands.
Footnotes
Presented at the EuroAmericn Multispecialty Summit III: Laparoscopy and Minimally Invasive Surgery, Orlando, Florida, USA, February 21–24, 2007.
References:
- 1.Mudge M, Hughes LE. Incisional hernia: a 10-year prospective study of incidence and attitudes. Br J Surg. 1985;72:70–71 [DOI] [PubMed] [Google Scholar]
- 2.Bucknall TE, Cox PJ, Ellis H. Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. BMJ. 1982;284:931–933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlson MA, Ludwig KA, Conlon RE. Ventral hernia and other complications of 1.000 midline incisions. South Med J. 1995;88:450–453 [DOI] [PubMed] [Google Scholar]
- 4.Pollock AV, Evans M. Early prediction of late incisional hernias. Br J Surg. 1989;76:953–954 [DOI] [PubMed] [Google Scholar]
- 5.Anthony T, Bergen PC, Kim LT, et al. Factors affecting recurrence following incisional herniorrhaphy; discussion 101. World J Surg. 2000;24:95–100 [DOI] [PubMed] [Google Scholar]
- 6.Santora TA, Roslyn JJ. Incisional hernia. Surg Clin North Am. 1993;73:557–570 [DOI] [PubMed] [Google Scholar]
- 7.Merrill CT, Elixhauser A. Hospitalization in the United States, 2002. HCUP Fact Book No. 6. AHRQ Publication No. 05– 0056, June 2005. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/data/hcup/factbk6/
- 8.Luijendijk R, Hop W, Van den Tol M, et al. A comparison of suture repair with mesh repair for incisional hernia. N Eng J Med. 2000;343:392–398 [DOI] [PubMed] [Google Scholar]
- 9.Anthony T, Bergen P, Kim L, et al. Factors affecting recurrence following incisional herniorrhaphy. World J Surg. 2000;24:95–101 [DOI] [PubMed] [Google Scholar]
- 10.LeBlanc KA, Booth WV. Laparoscopic repair of incisional abdominal hernias using polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc. 1993;3:39–41 [PubMed] [Google Scholar]
- 11.Stoppa RE. The treatment of complicated groin and incisional hernias. World J Surg. 1989;13:545–554 [DOI] [PubMed] [Google Scholar]
- 12.Rives J, Pire JC, Flament JB, et al. Treatment of large even-trations. New therapeutic indications apropos of 322 cases. Chirurgie. 1985;111:215–225 [PubMed] [Google Scholar]
- 13.Wantz GE. Incisional hernioplasty with Mersilene. Surg Gynecol Obstet. 1991;172:129–137 [PubMed] [Google Scholar]
- 14.White TJ, Santos MC, Thompson JS. Factors affecting wound complications in repair of ventral hernias. Am Surg. 1998;64:276–280 [PubMed] [Google Scholar]
- 15.Carbajo MA, del Olmo JC, Blanco JI, et al. Laparoscopic treatment of ventral abdominal wall hernias: preliminary results in 100 patients. J Soc Laparoendosc Surg. 2000;4:141–145 [PMC free article] [PubMed] [Google Scholar]
- 16.Franklin ME, Dorman JP, Glass JL, Balli JE, Gonzalez JJ. Laparoscopic ventral and incisional hernia repair. Surg Laparosc Endosc. 1998;8:294–299 [PubMed] [Google Scholar]
- 17.Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg. 2000;190:645–650 [DOI] [PubMed] [Google Scholar]
- 18.LeBlanc KA, Booth WV, Whitaker JM, Bellanger DE. Laparoscopic incisional and ventral herniorrhaphy: our initial 100 patients. Hernia. 2001;5:41–45 [DOI] [PubMed] [Google Scholar]
- 19.Constanza MJ, Heniford BT, Arca MJ, et al. Laparoscopic repair of recurrent ventral hernias. Am Surg. 1998;64:1121–1127 [PubMed] [Google Scholar]
- 20.Park A, Gagner M, Pomp A. Laparoscopic repair of large incisional hernias. Surg Laparosc Endosc. 1996;6:123–128 [PubMed] [Google Scholar]
- 21.Toy FK, Carey S, Chappuis CW, et al. Prospective, multi-center study of laparoscopic ventral hernioplasty. Surg Endosc. 1997;12:955–959 [DOI] [PubMed] [Google Scholar]
- 22.Heniford BT, RB Laparoscopic ventral hernia repair. Surg Endosc. 2002;14:419–423 [DOI] [PubMed] [Google Scholar]
- 23.Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias. Nine years' experience with 850 consecutive hernias. Ann Surg. 2003;238:391–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olmi S, Erba L, Magnone S, Bertolini A, Croce E. Prospective clinical study of laparoscopic treatment of incisional and ventral hernia using a composite mesh: indications, complications and results. Hernia. 2006;10:243–247 [DOI] [PubMed] [Google Scholar]
- 25.Pollock AV, Evans M. Early prediction of late incisional hernias. Br J Surg. 1989;76:953–954 [DOI] [PubMed] [Google Scholar]
- 26.Ausobsky JR, Evans M, Pollock AV. Does mass closure of midline laparotomies stand the rest of time? A random control clinical trial. Ann R Coll Surg Engl. 1985;67:159–161 [PMC free article] [PubMed] [Google Scholar]
- 27.Wissing J, van Vroonhoven TJ, Schattenkerk ME, Veen HF, Ponsen RJ, Jeekel J. Fascia closure after midline laparotomy: results of a randomized trial. Br J Surg. 1987;74:738–741 [DOI] [PubMed] [Google Scholar]
- 28.Weiland DE, Bay RC, Del Sordi S. Choosing the best abdominal closure by meta- analysis. Am J Surg. 1998;176:666–670 [DOI] [PubMed] [Google Scholar]
- 29.Hodgson NCF, Malthaner RA, Ostbye T. The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg. 2000;231:436–442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van't Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J. Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg. 2002;89:1350–1356 [DOI] [PubMed] [Google Scholar]
- 31.Ellis H, Gajraj H, George CD. Incisional hernias: when do they occur? Br J Surg. 1983;70:290–291 [DOI] [PubMed] [Google Scholar]
- 32.Burger JWA, Lange JF, Halm JA, Kleinrensink GJ, Jeekel H. Incisional hernia: early complication of abdominal surgery. World J Surg. 2005;29:1608–1613 [DOI] [PubMed] [Google Scholar]
- 33.Si Z, Bhardwaj R, Rosch R, Mertens PR, Klosterhalfen B, Klinge U. Impaired balance of type I and type III procollagen mRNA in cultured fibroblasts of patients with incisional hernia. Surgery. 2002;131:324–331 [DOI] [PubMed] [Google Scholar]
- 34.Rudmik LR, Schieman C, Dixon E. Laparoscopic incisional hernia repair: a review of the literature. Hernia. 2006;10:110–119 [DOI] [PubMed] [Google Scholar]
- 35.Dubay DA, Wang X, Kuhn MA, Robson MC, Franz MG. The prevention of incisional hernia formation using a delayed-release polymer of fibroblast growth factor. Ann Surg. 2004;240:179–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hesselink VJ, Luijendijk RW, de Wilt JH, et al. An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet. 1993;176:228–234 [PubMed] [Google Scholar]
- 37.White TJ, Santos MC, Thompson JS. Factors affecting wound complications in repair of ventral hernias. Am Surg. 1998;64:276–280 [PubMed] [Google Scholar]
- 38.Machairas A, Misiakos EP, Liakakos T, Karatzas G. Incisional hernioplasty with extraperitoneal onlay polyester mesh. Am Surg. 2004;70:726–729 [PubMed] [Google Scholar]
- 39.Leber GE, Garb JL, Alexander AI, Reed WP. Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg. 1998;133:378–382 [DOI] [PubMed] [Google Scholar]
- 40.Liakakos T, Karanikas I, Panagiotidis H, et al. Use of Marlex mesh in the repair of recurrent incisional hernia. Br J Surg. 1994;81:248–249 [DOI] [PubMed] [Google Scholar]
- 41.Langer C, Schaper A, Liersch T, et al. Prognosis factors in incisional hernia surgery: 25 years of experience. Hernia. 2005;9:16–21 [DOI] [PubMed] [Google Scholar]
- 42.de Vries Reilingh TS, van Geldere D, Langerhorst BLAM, et al. Repair of large midline incisional hernias with polypropylene mesh: comparison of three operative techniques. Hernia. 2004;8:56–59 [DOI] [PubMed] [Google Scholar]
- 43.Heartsill L, Richards ML, Arfai N, et al. Open Rives-Stoppa ventral hernia repair made simple and successful but not for everyone. Hernia. 2005;9:162–166 [DOI] [PubMed] [Google Scholar]
- 44.Yaghoobi Notash A, Yaghoobi Notash A, Jr., Seied Farshi J, et al. Outcomes of the Rives-Stoppa technique in incisional hernia repair: ten years of experience. Hernia. 2007;11:25–29 [DOI] [PubMed] [Google Scholar]
- 45.Martin-Duce A, Noguerales F, Villeta R, et al. Modifications to Rives technique for midline incisional hernia repair. Hernia. 2001;5:70–72 [DOI] [PubMed] [Google Scholar]
- 46.McCarthy JD, Twiest MW. Intraperitoneal polypropylene mesh support of incisional herniorrhaphy. Am J Surg. 1981;142:707–711 [DOI] [PubMed] [Google Scholar]
- 47.Millikan KW, Baptista M, Amin B, Deziel DJ, Doolas A. Intraperitoneal underlay ventral hernia repair utilizing bilayer expanded polytetrafluoroethylene and polypropylen mesh. Am Surg 2003;69:287–291, discussion 291–292 [PubMed] [Google Scholar]
- 48.Holzman MD, Purut CM, Reintgen K, Eubanks S, Pappas TN. Laparoscopic ventral and incisional hernioplasty. Surg Endosc. 1997;11:32–35 [DOI] [PubMed] [Google Scholar]
- 49.DeMaria EJ, Moss JM, Sugerman HJ. Laparoscopic intraperitoneal polytetrafluoroethylene (PTFE) prosthetic patch repair of ventral hernia. Prospective comparison to open prefascial polypropylene mesh repair. Surg Endosc. 2000;14:326–329 [DOI] [PubMed] [Google Scholar]
- 50.Yavuz N, Ipek T, As A, Kapan M, Eyuboglu E, Erguney S. Laparoscopic repair of ventral and incisional hernias: our experience in 150 patients. J Laparoendosc Adv Surg Techn. 2005;15:601–605 [DOI] [PubMed] [Google Scholar]
- 51.LeBlanc KA. Incisional hernia repair: laparoscopic techniques. World J Surg. 2005;29:1073–1079 [DOI] [PubMed] [Google Scholar]
- 52.Franklin ME, Jr, Gonzalez JJ, Jr, Glass JL, Manjarrez A. Laparoscopic ventral and incisional hernia repair: an 11-year experience. Hernia. 2004;8:23–27 [DOI] [PubMed] [Google Scholar]
- 53.Cassar K, Munro A. Surgical treatment of incisional hernia. Br J Surg. 2002;89:534–545 [DOI] [PubMed] [Google Scholar]
- 54.Franklin ME, Gonzalez JJ, Glass JL. Use of porcine small intestinal submucosa as a prosthetic device for laparoscopic repair of hernias in contaminated fields: 2-year follow-up. Hernia. 2004;8:186–189 [DOI] [PubMed] [Google Scholar]
- 55.Misra MC, Bansal VK, Kulkarni MP, Pawar DK. Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. Surg Endosc. 2006;20:1839–1845 [DOI] [PubMed] [Google Scholar]
- 56.LeBlanc KA, Booth WV, Whitaker JM, Bellanger DE. Laparoscopic incisional and ventral herniorrhaphy in 100 patients. Am J Surg. 2000;180:193–197 [DOI] [PubMed] [Google Scholar]
- 57.LeBlanc KA, Whitaker JM, Bellanger DE, Rhynes VK. Laparoscopic incisional and ventral hernioplasty: lessons learned from 200 patients. Hernia. 2003;7:118–124 [DOI] [PubMed] [Google Scholar]
- 58.Perrone JM, Soper NJ, Eagon JC, et al. Perioperative outcomes and complications of laparoscopic ventral hernia repair. Surgery 2005;138:708–715, discussion 715–716 [DOI] [PubMed] [Google Scholar]
- 59.Cobb WS, Kercher KW, Heniford BT. Laparoscopic repair of incisional hernias. Surg Clin North Am 2005;85:91–103, ix. Review [DOI] [PubMed] [Google Scholar]
- 60.Frantzides CT, Carlson MA, Zografakis JG, Madan AK, More RE. Minimally invasive incisional herniorrhaphy: a review of 208 cases. Surg Endosc. 2004;18:1488–1491 [DOI] [PubMed] [Google Scholar]
- 61.Bageacu S, Blanc P, Breton C, et al. Laparoscopic repair of incisional hernia: a retrospective study of 159 patients. Surg Endosc. 2002;16:345–348 [DOI] [PubMed] [Google Scholar]
- 62.Carbajo MA, Martp del Olmo JC, Blanco JI, et al. Laparoscopic approach to incisional hernia. Surg Endosc. 2003;17:118–122 [DOI] [PubMed] [Google Scholar]
- 63.Smietanski M, Bigda J, Iwan K, et al. Assessment of usefulness exhibited by different tacks in laparoscopic ventral hernia repair. Surg Endosc. 2007;21(6):925–928 [DOI] [PubMed] [Google Scholar]
- 64.Berger D, Bientzle M, Muller A. Postoperative complications after laparoscopic incisional hernia repair. Incidence and treatment. Surg Endosc. 2002;16:1720–1723 [DOI] [PubMed] [Google Scholar]
- 65.Raftopoulos I, Vanuno D, Khorsand J, Ninos J, Kouraklis G, Lasky P. Outcome of laparoscopic ventral hernia repair in correlation with obesity, type of hernia, and hernia size. J Laparoendosc Adv Surg Tech A. 2002;12:425–429 [DOI] [PubMed] [Google Scholar]
- 66.Sains PS, Tilney HS, Purkayastha S, et al. Outcomes following laparoscopic versus open repair of incisional hernia. World J Surg. 2006;30:2056–2064 [DOI] [PubMed] [Google Scholar]
- 67.Pierce RA, Spitler JA, Frisella MM, et al. Pooled data analysis of laparoscopic vs. open ventral hernia repair; 14 years of patient data accrual. Surg Endosc. 2007;21:378–386 [DOI] [PubMed] [Google Scholar]
- 68.Cobb WS, Kercher KW, Matthews BD, et al. Laparoscopic ventral hernia repair: a single center experience. Hernia. 2006;10:236–242 [DOI] [PubMed] [Google Scholar]
- 69.Rosen M, Brody F, Ponsky J, et al. Recurrence after laparoscopic ventral hernia repair. Surg Endosc. 2003;17:123–128 [DOI] [PubMed] [Google Scholar]