Abstract
To measure primary care access on an ongoing basis, the Ontario Ministry of Health and Long-Term Care implemented the Primary Care Access Survey (PCAS) in 2006. The PCAS, a cross-sectional telephone survey, samples approximately 8,400 Ontario adults each year. It collects information on access to a family doctor, use of services, health status and socio-demographics. Analysis of the 2007—2008 PCAS (n=16,560) shows that 7.1% of Ontario's adults were without a family doctor (i.e., unattached). The attached and unattached populations differed on socio-demographic and health characteristics. Emergency department use was similar between the two groups, but walk-in clinic use was higher among the unattached. The unattached were less likely to have used care for immediate issues but accessed care in a more timely fashion than the attached. This initial exploration of the PCAS provides a better understanding of some of the differences between the attached and unattached populations in Ontario.
Abstract
En 2006, le ministère ontarien de la Santé et des Soins de longue durée mettait en place le sondage sur lçaccès aux soins primaires (Primary Care Access Survey, ou PCAS) pour mesurer de façon continue lçaccès à ce type de soins. Le PCAS est une enquête téléphonique transversale dont lçéchantillon annuel est d'environ 8 400 Ontariens adultes. Elle permet de recueillir des renseignements sur lçaccès au médecin de famille, lçutilisation des services, lçétat de santé et la situation sociodémographique. L'analyse des données du PCAS de 2007—2008 (n=16 560) montre que 7,1 % des Ontariens adultes n'ont pas de médecin de famille. Les populations avec et sans médecin de famille présentent différentes caractéristiques sociodémographiques et sanitaires. L'utilisation du service des urgences est semblable entre les deux groupes, mais lçutilisation des cliniques sans rendez-vous est plus élevée chez ceux qui n'ont pas de médecin de famille. Ces derniers sont moins enclins à utiliser les services pour des besoins immédiats, cependant ils jouissent d'un accès en temps plus opportun que ceux qui ont un médecin de famille. Cette première exploration des données du PCAS permet une meilleure compréhension de certaines différences entre la population ontarienne qui a un médecin de famille et celle qui n'en a pas.
Access to family doctors is a concern to a large number of Ontario residents and has become part of the public discourse on primary care. Having a family doctor has many important benefits, including earlier treatment for potentially difficult conditions, more preventative care (such as blood pressure checks, mammograms and Pap smears) and better management of chronic disease (Lambrew et al. 1996; DeVoe et al. 2003; McIsaac et al. 2001; Xu 2002). Having an established physician—patient relationship also contributes to better continuity and improved patient satisfaction (Hjortdahl and Laerum 1992; Schoen et al. 2004).
Patients without family physicians may use other services such as walk-in clinics or emergency departments as a substitute for primary care (Baker et al. 1994; Rask et al. 1994; Schoen et al. 2004). However, the use of such services is viewed as an inadequate substitute because it may disrupt coordination of care and leave patients at higher risk for drug interactions and delays in receiving results of lab or diagnostic tests (Lowe et al. 2005; Schoen et al. 2004). While the majority of patients using walk-in clinics have regular family doctors, there is some suggestion of lower attachment rates among visitors to clinics (Jones 2000). As with emergency departments, the substitution of walk-in clinics is related to patients' perceptions of timely primary care (Szafran and Bell 2000).
Although the vast majority of Ontario residents have regular medical doctors (Ontario Health Quality Council 2009), those without family doctors are an important concern for health jurisdictions from both population health and policy perspectives. Lower likelihood of having a family doctor has been associated with certain demographic characteristics such as younger age and being male (Merzel 2000; Viera et al. 2006; Talbot et al. 2001; DeVoe et al. 2003), as well as social factors such as single marital status, lower educational attainment and lack of English language skills (Talbot et al. 2001; Sanmartin and Ross 2006; Ponce et al. 2006; McIsaac et al. 2001). There is some evidence that those without family doctors tend to be in better health (Hayward et al. 1991; Viera et al. 2006; Nabalamba and Millar 2007; Talbot et al. 2001). Urban/rural differences in access and use of primary care have been found in some studies (DeVoe et al. 2003; Finkelstein 2001; Nabalamba and Millar 2007; Sanmartin et al. 2006; Wellstood et al. 2006), but this relationship is likely highly contextualized and partially dependent on variations in physician supply (Chaix et al. 2005).
Existing data sources such as the Canadian Community Health Survey (CCHS) can be used to determine the number of Ontarians without family doctors and their socio-demographic characteristics. However, the data are not always timely and do not capture some of the salient information needed for provincial planning. In order to inform policy, planning and management, to measure health system performance and to further research on primary care issues in Ontario, it was determined that a data source focused specifically on primary care physician access in Ontario was needed. In 2006, the Ontario Ministry of Health and Long-Term Care, in consultation with the Ontario Medical Association, the Ontario College of Family Physicians and the Institute for Clinical Evaluative Sciences, developed the Primary Care Access Survey (PCAS). Key to this initiative was the need for timely information on access, regional variation and utilization trends and the need to monitor the impact of significant primary care reforms underway in Ontario. Additionally, and perhaps more critically, there was an implicit assumption that the perceived challenges in access to care for those without a regular doctor were not being adequately examined and documented. The PCAS was designed to measure, on an ongoing basis, access to family doctors in Ontario and thus better understand the factors that may contribute to having a family doctor and accessing primary care. Measuring primary care access includes determining both the number of people who do and do not have regular family doctors, known as the attached and unattached populations, respectively, along with their experiences in attaining care, and their health and socio-demographic characteristics.
The purpose of this paper is to introduce readers to the PCAS and to use these survey data to describe the characteristics and patterns of access to primary care in Ontario by comparing the unattached and attached populations.
Methods
Data source
The PCAS began in January 2006. The survey is administered by telephone by the Institute for Social Research (ISR) at York University. Respondents are asked about their perceptions of the healthcare system in Ontario, their health status, family doctor status, reasons for not having a family doctor, their family doctor's practice setting, utilization of primary care services, socio-demographics and household composition, and coverage under the Ontario Health Insurance Plan. Each interview, conducted in either English or French, takes approximately 15 to 20 minutes to complete.
The survey covers the household population age 16 and older in Ontario. The sample is allocated equally among the 14 Local Health Integration Networks (LHINs) in Ontario, maximizing the ability to compare primary care access among the LHINs. Data are collected over the course of the year but use a quarterly sampling frame to facilitate trending over time. A minimum of 150 interviews are completed per quarter per LHIN, for a total provincial sample of approximately 2,100 every three months.
Sample design
A modified random digit dialling (RDD) sample, designed by ISR, used the following steps. First, an inventory of known telephone numbers was developed from published sources such as telephone books, street directories and subscribers' lists. These numbers were included in the sampling frame and a random list of numbers was subsequently generated to create the sample. When interviewers dial a number, they determine whether it is in service and whether it is a household number. Interviewers then randomly select an adult respondent aged 16 or older, living in the household, who is able to speak either English or French. Up to 12 call attempts are made, and if there is good reason to believe an interview will be obtained, more calls are completed. Calls are made during the day, evenings and on weekends. Computer-assisted telephone interviewing (CATI) is used in data collection. Households without telephones and some households that use only cellular phones are not included in the sample design. Of the estimated number of eligible households in the sample, 59% completed the survey.
Measures
The variables collected by the PCAS and described in this paper provide information on predisposing, enabling and need characteristics, consistent with the framework for examining access to healthcare services developed by Andersen (Andersen and Newman 1973; Andersen 1995). Seven measures of primary care access were examined: attachment to family doctors; family doctor utilization for routine care, immediate care and overall care; walk-in clinic utilization; emergency department utilization; and the time to see family doctors for immediate care. All utilization measures were based on one or more visits to a family doctor in the 12 months preceding the interview. The reference period for questions related to use and access of care was also the past 12 months. These measures and some key terms are defined in Table 1. More detailed descriptions of the social, demographic and health status variables presented in this paper are available from the authors.
TABLE 1.
Key definitions
| Terms | Definitions |
|---|---|
| Family doctors | Refers to the doctor whom respondents typically see for routine care and non-emergent problems; includes family doctors, family physicians, general practitioners or medical doctors but does not include dentists, eye doctors, gynaecologists or obstetricians. |
| Attached patients | Respondents who have family doctors. |
| Unattached patients | Respondents who do not have family doctors. |
| Routine care | Refers to regular check-ups or monitoring of ongoing health issues. |
| Immediate care | Refers to urgent health problems that require immediate attention, for example, when sick. |
| Overall care | Includes routine care, immediate care, care to obtain health information, or for advice regarding whether care is necessary. |
| Walk-in clinic visits | Refers to any visits to walk-in clinics for a health-related reason. |
| Emergency department visits | Refers to any visits to emergency departments for any health-related problems. |
| Time to see family doctor for immediate care | Based on the number of days it took respondents to obtain an appointment from a family doctor when they were sick. |
| Urban/rural geography | Urban refers to continuously built-up areas with a minimum population of 1,000 and a minimum population density of 400 per square kilometres. All other areas are defined as rural. Derived from respondent's postal code using the Postal Code Conversion File (Statistics Canada 2009). |
Analyses
Seventeen thousand, one hundred thirty-seven respondents were interviewed in 2007 and 2008. Sampling weights were used to correct for the unequal probability of selection with respect to household size (i.e., the number of adults aged 16 and older in the household) and the LHIN in which the respondent resided. Post-stratification adjustments were subsequently applied to the weighted sample so that the total age and sex categories reflected the 2007 Ontario population structure.
Respondents who did not report their age (n=577) were excluded from analysis (all respondents must be assigned to an age group to post-stratify the data), leaving a sample of 16,560 respondents. For each question, respondents reporting “don't know” or “refused” were excluded from the analysis of that item. The “don't know” and “refused” categories accounted for less than 2.2% of responses for each item, with the exception of geography. Ten per cent of respondents were not assigned to urban/rural geography because of missing or invalid postal codes.
All analyses were based on the post-stratified weighted sample, which is representative of the Ontario population aged 16 or older. Analyses were conducted using Stata Version 10.1 (StataCorp. 2008) using the program's complex survey analysis module to calculate estimates and confidence intervals at the 95% level. Weighted frequency estimates were produced to describe the characteristics of the study population. Bivariate analyses were performed to determine the association between attachment and socio-demographic characteristics, family doctor utilization, walk-in clinic and emergency department utilization, and the length of time to obtain immediate care. Differences between estimates were tested for statistical significance at the level of p<0.05, using chi-square tests.
Results
Table 2 shows selected characteristics of the Ontario population based on responses from PCAS respondents. A total sample of 16,560 was weighted to represent 10.4 million Ontarians aged 16+. According to the 2007 and 2008 PCAS data, almost 93% of Ontario residents, aged 16 or over, reported they have a family doctor (i.e., are attached).
TABLE 2.
Characteristics of study population aged 16 or older, ontario (2007 and 2008)
| Unattached (no family doctor) | Attached (has family doctor) | Total | |||||
|---|---|---|---|---|---|---|---|
| PCAS sample | (n=1,260) | (n=15,300) | (n=16,560) | ||||
| Estimated population (weighted sample) | (N=733,566) | (N=9,658,311) | (N=10,391,877) | ||||
| % of estimated population§ | 95% CI | % of estimated population§ | 95% CI | % of estimated population§ | 95% CI | p value† (unattached vs attached) | |
| Total population, aged 16+ | 7.1 | 6.6, 7.5 | 92.9 | 92.5, 93.4 | 100.0 | ||
| Gender1 | |||||||
| Male | 58.7 | 55.4, 62.0 | 48.2 | 47.9, 48.4 | 48.9 | - | p < 0.01 |
| Female | 41.3 | 38.0, 44.6 | 51.8 | 51.6, 52.1 | 51.1 | - | |
| Age1 | |||||||
| 16–24 | 17.2 | 14.2, 20.1 | 14.9 | 14.7, 15.2 | 15.1 | - | p < 0.01 |
| 25–34 | 25.1 | 21.9, 28.2 | 16.1 | 15.9, 16.4 | 16.8 | - | |
| 35–64 | 49.4 | 46.0, 52.8 | 52.1 | 51.9, 52.4 | 51.9 | - | |
| 65+ | 8.4 | 6.8, 9.9 | 16.8 | 16.7, 16.9 | 16.2 | - | |
| Education | |||||||
| Less than high school | 10.9 | 8.8, 12.9 | 13.2 | 12.6, 13.8 | 13.1 | 12.5, 13.6 | |
| High school or some post-secondary | 35.2 | 31.8, 38.6 | 35.6 | 34.7, 36.5 | 35.6 | 34.7, 36.4 | |
| Post-secondary or higher completed | 54.0 | 50.5, 57.5 | 51.2 | 50.3, 52 | 51.4 | 50.5, 52.2 | |
| Employment | |||||||
| Employed | 67.0 | 63.7, 70.3 | 62.1 | 61.3, 62.8 | 62.4 | 61.7, 63.1 | p < 0.01 |
| Unemployed | 6.8 | 5.0, 8.7 | 3.2 | 2.9, 3.6 | 3.5 | 3.1, 3.8 | |
| Student | 11.8 | 9.2, 14.4 | 9.0 | 8.4, 9.5 | 9.2 | 8.6, 9.7 | |
| Retired | 9.7 | 8.1, 11.3 | 20.0 | 19.6, 20.4 | 19.3 | 18.9, 19.6 | |
| Other | 4.7 | 3.4, 6.0 | 5.7 | 5.3, 6.1 | 5.7 | 5.3, 6.1 | |
| Family size | |||||||
| 2 or more children | 10.5 | 8.5, 12.5 | 13.8 | 13.2, 14.4 | 13.6 | 13.0, 14.1 | p<0.05 |
| 1 child | 14.1 | 11.5, 16.7 | 13.4 | 12.7, 14.0 | 13.4 | 12.8, 14.1 | |
| 0 children | 75.4 | 72.3, 78.5 | 72.9 | 72.1, 73.6 | 73.0 | 72.3, 73.8 | |
| Immigrant status | |||||||
| Non-immigrant | 76.8 | 73.7, 79.8 | 73.1 | 72.2, 73.9 | 73.3 | 72.5, 74.2 | p<0.01 |
| Established immigrants (10+ yrs in canada) | 14.7 | 12.2, 17.1 | 21.4 | 20.6, 22.2 | 20.9 | 20.1, 21.7 | |
| Recent immigrants (<10 yrs in canada) | 8.6 | 6.4, 10.8 | 5.6 | 5.1, 6.1 | 5.8 | 5.3, 6.3 | |
| Geography | |||||||
| Urban | 81.3 | 78.7, 84.0 | 79.6 | 78.9, 80.4 | 79.7 | 79.0, 80.5 | |
| Rural | 18.7 | 16.0, 21.3 | 20.4 | 19.6, 21.1 | 20.3 | 19.5, 21.0 | |
| Healthcare system system confidence | |||||||
| Very/somewhat confident | 59.5 | 56.1, 63.0 | 67.3 | 66.4, 68.2 | 66.8 | 65.9, 67.7 | p<0.01 |
| Not very/not confident | 40.5 | 37.0, 43.9 | 32.7 | 31.8, 33.6 | 33.2 | 32.3, 34.1 | |
| Has medical training | |||||||
| Yes | 10.2 | 8.1, 12.2 | 11.3 | 10.7, 11.9 | 11.2 | 10.6, 11.8 | |
| No | 89.8 | 87.8, 91.9 | 88.7 | 88.1, 89.3 | 88.8 | 88.2, 89.4 | |
| Number of chronic diseases2 | |||||||
| None | 66.0 | 62.7, 69.3 | 56.1 | 55.2, 57.0 | 56.8 | 56.0, 57.6 | p<0.01 |
| 1 | 22.7 | 19.7, 25.8 | 24.9 | 24.1, 25.7 | 24.7 | 23.9, 25.5 | |
| 2 or more | 11.3 | 9.4, 13.1 | 19.0 | 18.4, 19.6 | 18.5 | 17.9, 19.0 | |
| Health status | |||||||
| Excellent/Very good | 59.6 | 56.2, 63.1 | 58.7 | 57.7, 59.6 | 58.7 | 57.8, 59.7 | |
| Good | 27.3 | 24.1, 30.5 | 26.7 | 25.8, 27.6 | 26.8 | 25.9, 27.6 | |
| Fair/Poor | 13.0 | 10.8, 15.3 | 14.6 | 13.9, 15.3 | 14.5 | 13.9, 15.2 | |
Percentages are based on the weighted number of survey respondents to ensure estimates are representative of the population.
Test for significance between unattached and attached groups based on χ2 test.
1PCAS data are post-stratified by age and gender and thus no confidence intervals are available.
2Refers to selected chronic diseases including arthritis, asthma, cancer, chronic respiratory problems, diabetes, heart disease/stroke or high blood pressure.
The attached and unattached populations were significantly different with respect to socio-demographic and health characteristics including gender, age, employment, family size, immigrant status, healthcare system confidence and chronic diseases. Those without a family doctor were more likely to be male, younger or recent immigrants. Their employment status was more likely to be employed or unemployed, and they were less likely to report chronic conditions. Ontarians with a family doctor were more likely to be retired, have two or more children or be established immigrants. They were more likely to report they have confidence in the healthcare system and also more likely to have multiple chronic conditions.
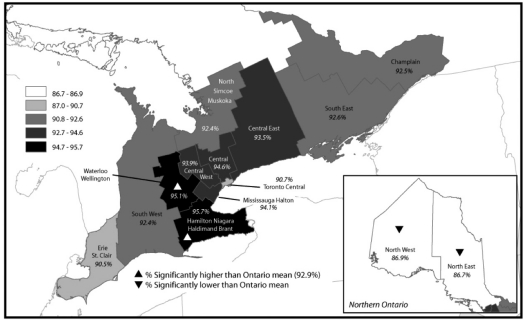
Figure 1 illustrates the geographic variation in the proportion of the population with a family doctor across Ontario's 14 LHINs. In six LHINs (those surrounding the Toronto Central LHIN), between 93% to 95% of the population were attached to a family doctor. The proportion was only slightly lower in the South West, South East, Champlain and North Simcoe Muskoka LHINs (between 92% to 93%). Compared to the provincial average, Hamilton Niagara Haldimand Brant and Waterloo Wellington LHINs had significantly higher proportions of residents attached to a family doctor, whereas North East and North West LHINs had a significantly lower proportion.
FIGURE 1.
Percentage of attached patients, population aged 16 or older, by Ontario LHINs (2007 and 2008)
The relationship between attachment and access to primary care services is presented in Table 3. Unattached residents were less likely to report they received care in the past year. In comparison to the unattached population, those with a family doctor were almost three times more likely to report they received routine care such as monitoring of health issues or check-ups (73% versus 26%). They were also more likely than unattached residents to report having received immediate care, but the difference was less pronounced (36% versus 26%). Although the use of walk-in clinics was almost twice as high among the unattached population compared to the attached, the use of emergency departments was similar between the two groups.
TABLE 3.
Use of primary care services by unattached and attached persons, Ontario (2007 and 2008)
| Unattached (no family doctor) | Attached (has family doctor) | Total population | p value† (unattached vs attached) | ||||
|---|---|---|---|---|---|---|---|
| Per cent | 95% CI | Per cent | 95% CI | Per cent | 95% CI | ||
| Overall care | 50.1 | 46.5, 53.6 | 84.1 | 83.3, 84.8 | 81.7 | 80.9, 82.4 | p<0.01 |
| Routine care | 25.9 | 22.8, 29.0 | 73.1 | 72.2, 73.9 | 69.7 | 68.9, 70.6 | p<0.01 |
| Immediate care | 25.7 | 22.5, 28.9 | 36.0 | 35.0, 37.0 | 35.3 | 34.4, 36.2 | p<0.01 |
| Use of walk-in clinic | 47.9 | 44.4, 51.5 | 24.6 | 23.7, 25.4 | 26.2 | 25.4, 27.1 | p<0.01 |
| Emergency department use | 20.8 | 18.0, 23.6 | 20.5 | 19.7, 21.3 | 20.6 | 19.8, 21.3 | |
Percentages are based on the weighted number of survey respondents to ensure estimates are representative of the population.
Test for significance between Unattached and Attached groups based on χ2 test
Those who had sought care for an urgent health issue were asked how long it took them to receive immediate care. The relationship between attachment and the length of time (in days) it took to see family doctors for immediate care is presented in Table 4. Compared to attached residents, a much larger percentage of unattached residents reported they were able to see a family doctor on either the same day or within one day from when they first tried to obtain care.
TABLE 4.
Amount of time (in days) to access immediate care by unattached and attached persons, Ontario (2007 and 2008)
| Unattached (no family doctor) | Attached (has family doctor) | Total population | p value† (unattached vs attached) | ||||
|---|---|---|---|---|---|---|---|
| Per cent | 95% CI | Per cent | 95% CI | Per cent | 95% CI | ||
| Same day | 59.5 | 52.9, 66.1 | 26.4 | 25.4, 29.5 | 28.1 | 26.6, 29.6 | p<0.01 |
| Within 1 day | 66.3 | 59.9, 72.8 | 46.1 | 44.9, 49.6 | 47.1 | 45.5, 48.7 | p<0.01 |
| Within 2 days | 71.5 | 65.3, 77.7 | 62.8 | 60.9, 65.5 | 63.2 | 61.6, 64.8 | p<0.05 |
Percentages are based on the weighted number of survey respondents to ensure estimates are representative of the population.
Test for significance between unattached and attached groups based on χ2 test.
Discussion and Conclusion
In 2007 and 2008, approximately 734,000 Ontario residents (aged 16+), representing 7.1% of the provincial population, did not have a family doctor. This figure is lower than estimates from national surveys, which had reported that 9.0% of Ontarians are without a regular medical doctor (CCHS 2007). The PCAS results show substantial geographic variation in attachment rates within Ontario, with lower attachment rates in northern regions of the province relative to the south.
The PCAS results suggest that the unattached and attached populations are not homogenous with respect to their socio-demographic characteristics nor in their use of primary care services. The unattached population was more likely to be male, younger, recent immigrants and healthier in terms of the number of chronic conditions. These differences are consistent with previous findings showing that those with and without family doctors differed with respect to health status and demographic characteristics (Talbot et al. 2001; McIsaac et al. 2001; Viera et al. 2006; Nabalamba and Millar 2007).
A previous study of Canadians had shown that those without a regular medical doctor were more likely to report difficulties accessing routine care but not immediate care (Sanmartin and Ross 2006). Although we did not look at difficulties in accessing care, we did find that unattached persons were much less likely to have used routine care in the past year. Because the unattached population is younger and healthier than those who are attached, the lower use of routine care may reflect either a self-perceived lack of need for these services, a potential lack of access to the services or a combination of the two.
The findings on the use and timing for immediate care services suggest that although those without a family doctor were less likely to have used care for an urgent problem, when they did access care they were able to do so in a more timely fashion than those with a family doctor. This may be because of the higher use of walk-in clinics among residents without a family doctor. Interestingly, approximately 20% of the attached still made use of walk-in clinics, a finding that is perhaps due to less timely access from their regular family doctors. This finding is consistent with other studies that have shown that those with a regular doctor may still experience challenges in timely access (Szafran and Bell 2000; Sanmartin et al. 2004; Wellstood et al. 2006), and that those with a family doctor may also substitute these services when timely access is not available (Rust et al. 2008; Matthews and Barnsley 2003). It is noteworthy that use of emergency departments is similar for attached and unattached Ontarians, suggesting that the unattached population does not place an overt burden on emergency services.
The limitations that typically apply to cross-sectional survey data (e.g., validity and reliability of self-reported data, generalizability of the sample) and its analysis (causal relationships between variables cannot be inferred) apply here. More specifically, PCAS household telephone survey methodology does not capture households without a telephone and may not include those that use cellular telephones exclusively. Because 92.5% of Ontario households have a land line phone and only 5% use a cellphone exclusively, this limitation is unlikely to bias our results (Statistics Canada 2007). Nonetheless, the PCAS has been instrumental in providing up-to-date estimates of unattachment rates at the provincial and LHIN levels because the continuous data collection permits ongoing monitoring. Physician attachment has been improving in Ontario (MOHLTC 2009), and the results from the PCAS suggest that fears of a burgeoning physician access problem may have been overstated. Regardless, a substantial number of Ontarians are without regular doctors and are therefore not able to receive comprehensive primary care. PCAS results show that despite this situation, primary care is being accessed by the unattached population, and their needs for immediate care are met within the same or better time frame as those with regular doctors. The unattached use walk-in clinics rather than emergency departments, but because the distribution of such clinics is greatest in urban areas, attention must be paid to those areas where alternative primary care is not readily available — notably, in rural and northern communities.
In Ontario, PCAS findings have been instrumental in shifting the policy emphasis from physician supply to strategies to promote attachment. For example, the PCAS identified the need for the Health Care Connects program, which helps Ontarians who are unattached find healthcare providers. Eligible registrants are prioritized for attachment, and physicians receive incentives to roster new patients. The ministry has also created a medical services directory for Ontarians seeking care to reduce reliance on emergency rooms. This directory includes information on walk-in clinics, acknowledging the role these clinics play in meeting the needs of unattached residents.
There is considerable scope for future research using the PCAS data, and some of this analysis is under way. While this initial exploration of the PCAS data provides a better description of some of the major differences between the attached and unattached populations in Ontario, more nuanced multivariate analyses will provide a better understanding of the relationship between demographic, social and health status characteristics and unattachment. From a research perspective, a more thorough understanding of the dynamics of unattachment in Ontario is required. PCAS results (not shown here) show that almost a third report that they are unattached because they have moved, suggesting that 100% attachment rates are an unrealistic goal. Identifying what would be a reasonable target requires understanding of such dynamics. Furthermore, the incorporation of the PCAS with data on the supply side, and a greater exploration of factors influencing geographic differences, will better inform policy and, in the long run, help improve access for Ontario residents.
Contributor Information
Carley Hay, Senior Health Analyst, Health Analytics Branch, Health System Information Management and Investment, Ontario Ministry of Health and Long-Term Care, Toronto, ON.
Michael Pacey, Senior Health Analyst, Health Analytics Branch, Health System Information Management and Investment, Ontario Ministry of Health and Long-Term Care, Kingston, ON.
Namrata Bains, Manager, LHIN Support Unit, Health Analytics Branch, Health System Information Management and Investment, Ontario Ministry of Health and Long-Term Care, Adjunct Lecturer, Department of Community Health and Epidemiology, Queen's University, Kingston, ON.
Sten Ardal, Director, Health Analytics Branch, Health System Information Management and Investment, Ontario Ministry of Health and Long-Term Care, Adjunct Faculty, School of Health Policy and Management, York University, Adjunct Faculty, Department of Health Policy Management and Evaluation, University of Toronto, Toronto, ON.
References
- Andersen R.M. Revisiting the Behavioral Model and Access to Medical Care: Does It Matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Andersen R., Newman J.F. Societal and Individual Determinants of Medical Care Utilization in the United States. Milbank Memorial Fund Quarterly. Health and Society. 1973;51(1):95–124. [PubMed] [Google Scholar]
- Baker D.W., Stevens C.D., Brook R.H. Regular Source of Ambulatory Care and Medical Care Utilization by Patients Presenting to a Public Hospital Emergency Department. Journal of the American Medical Association. 1994;271(24):1909–12. [PubMed] [Google Scholar]
- Canadian Community Health Survey (CCHS) 2005 (Cycle 3.1). 2007. Oct 10, Retrieved October 8, 2010. < http://www.statcan.gc.ca/cgi-bin/imdb/p2SV.pl?Function=getSurvey&SurvId=3226&SurvVer=0&InstaId=15282&InstaVer=3&SDDS=3226&lang=en&db=imdb&adm=8&dis=2>.
- Chaix B., Veugelers P.J., Boelle P.-Y., Chauvin P. Access to General Practitioner Services: The Disabled Elderly Lag Behind in Underserviced Areas. European Journal of Public Health. 2005;15(3):282–87. doi: 10.1093/eurpub/cki082. [DOI] [PubMed] [Google Scholar]
- DeVoe J.E., Fryer G.E., Phillips R., Green L. Receipt of Preventative Care among Adults: Insurance Status and Usual Source of Care. American Journal of Public Health. 2003;93:786–91. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein M.M. Do Factors Other Than Need Determine Utilization of Physicians' Services in Ontario? Canadian Medical Association Journal. 2001;165(5):565–70. [PMC free article] [PubMed] [Google Scholar]
- Hayward R.A., Bernard A.M., Freeman H.E., Corey C.R. Regular Source of Ambulatory Care and Access to Health Services. American Journal of Public Health. 1991;81(4):434–438. doi: 10.2105/ajph.81.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjortdahl P., Laerum E. Continuity of Care in General Practice: Effect on Patient Satisfaction. British Medical Journal. 1992;304:1287–90. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones M. Walk-in Primary Medical Care Centres: Lessons from Canada. British Medical Journal. 2000;321:928–31. doi: 10.1136/bmj.321.7266.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambrew J.M., DeFriese G.H., Carey T.S., Ricketts T.C., Biddle A.K. The Effects of Having a Regular Doctor on Access to Primary Care. Medical Care. 1996;34(2):138–51. doi: 10.1097/00005650-199602000-00006. [DOI] [PubMed] [Google Scholar]
- Lowe R.A., Localio A.R., Schwarz D.F., Williams S., Tuton L.W., Maroney S., Nicklin D., Goldfarb N., Vojta D.D., Feldman H.I. Association between Primary Care Practice Characteristics and Emergency Department Use in a Medicaid Managed Care Organization. Medical Care. 2005;43(8):792–800. doi: 10.1097/01.mlr.0000170413.60054.54. [DOI] [PubMed] [Google Scholar]
- Matthews M., Barnsley J. Patients Seeking Care during Acute Illness: Why Do They Not See Regular Physicians? Canadian Family Physician. 2003;49:1498–503. [PMC free article] [PubMed] [Google Scholar]
- McIsaac W.J., Fuller-Thomson E., Talbot Y. Does Having Regular Care by a Family Physician Improve Preventative Care? Canadian Family Physician. 2001;47:70–76. [PMC free article] [PubMed] [Google Scholar]
- Menec V.H., Roos N.P., Black C., Bogdanovich B. Characteristics of Patients with a Regular Source of Care. Canadian Journal of Public Health. 2001;92(4):299–303. doi: 10.1007/BF03404965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merzel C. Gender Differences in Health Care Access Indicators in an Urban, Low-Income Community. American Journal of Public Health. 2000;90(6):909–16. doi: 10.2105/ajph.90.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Long-Term Care (MOHLTC). 800,000 More Ontarians Find a Family Doctor. News release. 2009. Jul 21, Retrieved October 8, 2010. < http://www.health.gov.on.ca/en/news/release/2009/jul/nr_20090721.aspx>.
- Nabalamba A., Millar W.J. Going to the Doctor. Health Reports. 2007;18(1):23–35. [PubMed] [Google Scholar]
- Ontario Health Quality Council. Q Monitor: 2009 Report on Ontario's Health System (Chapter 2). 2009. Retrieved October 8, 2010. < http://www.ohqc.ca/pdfs/ohqc_2009_report_-_english.pdf>.
- Ponce N.A., Hays R.D., Cunningham W.E. Linguistic Disparities in Health Care Access and Health Status among Older Adults. Journal of General Internal Medicine. 2006;21(7):786–91. doi: 10.1111/j.1525-1497.2006.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rask K.J., Williams M.V., Parker R.M., McNagny S.E. Obstacles Predicting Lack of a Regular Provider and Delays in Seeking Care for Patients at an Urban Public Hospital. Journal of the American Medical Association. 1994;271(24):1931–33. [PubMed] [Google Scholar]
- Rust G., Ye J., Baltrus P., Daniels E., Adesunloye B., Fryer G.E. Practical Barriers to Timely Primary Care Access. Archives of Internal Medicine. 2008;168(15):1705–10. doi: 10.1001/archinte.168.15.1705. [DOI] [PubMed] [Google Scholar]
- Sanmartin C., Gendron F., Berthelot J.M., Murphy K. Access to Health Care Services in Canada, 2003. Ottawa: Statistics Canada, Minister of Industry; 2004. Statistics Canada, Catalogue 82-575-XIE 2004. [Google Scholar]
- Sanmartin C., Berthelot J.M., Ng E., Murphy K., Blackwell D.L., Gentlemen J.F., Martinez M.E., Simile C.M. Comparing Health and Health Care in Canada and the United States. Health Affairs. 2006;25(4):1133–42. doi: 10.1377/hlthaff.25.4.1133. [DOI] [PubMed] [Google Scholar]
- Sanmartin C., Ross N. Experiencing Difficulties Accessing First-Contact Health Services in Canada. Healthcare Policy. 2006;1(2):103–19. [PMC free article] [PubMed] [Google Scholar]
- Schoen C., Osborn R., Huynh P.T., Doty M., Davis K., Zapert K., Peugh J. Primary Care and Health System Performance: Adults' Experience in Five Countries. Health Affairs. 2004;(Suppl. Web Exclusives):W4-487–503. doi: 10.1377/hlthaff.w4.487. [DOI] [PubMed] [Google Scholar]
- StataCorp. Statistical Software. Release 10.1. College Station, TX: Stata Corporation; 2008. [Google Scholar]
- Statistics Canada. Residential Telephone Service Survey 2006. Ottawa: Minister of Industry; 2007. Catalogue no. 56M0001x. [Google Scholar]
- Statistics Canada. Postal Code Conversion File (PCCF), Reference Guide. September 2008 Postal Codes. Ottawa: Minister of Industry; 2009. Catalogue no. 920153-G. [Google Scholar]
- Szafran O., Bell N.R. Use of Walk-in Clinics by Rural and Urban Patients. Canadian Family Physician. 2000;46(1):114–19. [PMC free article] [PubMed] [Google Scholar]
- Talbot Y., Fuller-Thomson E., Tudiver F., Habib Y., McIsaac W.J. Canadians without a Medical Doctor: Who Are They? Canadian Family Physician. 2001;47:58–64. [PMC free article] [PubMed] [Google Scholar]
- Viera A.J., Pathman D.E., Garrett J.M. Adults' Lack of a Usual Source of Care: A Matter of Preference? Annals of Family Medicine. 2006;4(4):359–65. doi: 10.1370/afm.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellstood K., Wilson K., Eyles J. ‘Reasonable Access’ to Primary Care: Assessing the Role of Individual and System Characteristics. Health & Place. 2006;12(2):121–30. doi: 10.1016/j.healthplace.2004.10.010. [DOI] [PubMed] [Google Scholar]
- Xu K.T. Usual Source of Care in Preventive Service Use: A Regular Doctor versus a Regular Site. Health Services Research. 2002;37(6):1509–29. doi: 10.1111/1475-6773.10524. [DOI] [PMC free article] [PubMed] [Google Scholar]