Abstract
The vast majority of traumatic brain injuries (TBI) in children are of mild severity. Even if only a small proportion of children with mild TBI suffer negative outcomes, then mild TBI is a serious public health problem. This review summarizes the literature regarding the neurobehavioral outcomes associated with mild TBI in children and adolescents, focusing on the longstanding debate regarding postconcussive symptoms and attendant conceptual and methodological issues. The review also discusses future research directions, the long-term goal of which is to develop a comprehensive and integrated biopsychosocial model of outcomes that helps guide clinical management.
Keywords: mild head injury, concussion, pediatric, outcomes
Mild traumatic brain injuries (TBI) are common in children and adolescents. Annually, as many as 500,000 youth under the age of 15 sustain TBI that require hospital-based medical care in the United States, and the large majority of these injuries are mild in severity (Bazarian et al., 2005; Kraus, 1995). Even if only a small proportion of children with mild TBI suffer persistent negative outcomes, then mild TBI is a serious public health problem.
More than a decade ago, additional research on mild TBI was identified as a pressing need in national consensus conferences in the United States (NIH Consensus Panel on Rehabilitation of Persons with Traumatic Brain Injury, 1999; Seidel et al., 1999). The need for additional research is particularly acute given the decreasing rate of hospitalization for children with mild TBI (Bowman et al., 2008). This trend places a burden on health care providers in emergency medicine and outpatient care settings to make informed decisions regarding the management of mild TBI in children and adolescents.
This review summarizes the existing literature regarding the neurobehavioral outcomes of mild TBI in children and adolescents, focusing on the longstanding debate regarding postconcussive symptoms. Conceptual and methodological issues that arise in research on the outcomes of mild TBI are discussed, and the review concludes with suggestions for future research directions.
What’s In a Name?
Many different terms have been used to refer to mild TBI, including minor closed-head injury (American Academy of Pediatrics, 1999), mild traumatic brain injury (American Congress of Rehabilitation Medicine, 1993), and concussion (McCrory et al., 2009). The differences in terminology are a frequent cause of confusion, and hamper comparisons of findings across different research studies (Bodin, Yeates, & Klamar, in press). Recently, the World Health Organization (WHO) Collaborating Centre Task Force on Mild Traumatic Brain Injury (Carroll et al., 2004a) offered the following operational definition of mild TBI:
“MTBI is an acute brain injury resulting from mechanical energy to the head from external physical forces. Operational criteria for clinical identification include: (i) 1 or more of the following: confusion or disorientation, loss of consciousness for 30 minutes or less, post-traumatic amnesia for less than 24 hours, and/or other transient neurological abnormalities such as focal signs, seizure, and intracranial lesion not requiring surgery; (ii) Glasgow Coma Scale score of 13–15 after 30 minutes post-injury or later upon presentation for healthcare.”
The variability in terminology and associated criteria likely hampers the accurate identification and diagnosis of children with mild TBI (Powell et al., 2008). Epidemiological studies of mild TBI are also hindered by the use of International Classification of Diseases (ICD; World Health Organization, 1992) diagnostic codes employed in most clinical settings (National Center for Injury Prevention and Control, 2003). The ICD includes multiple codes that are potentially applicable to mild TBI, but most are not limited to injuries that are exclusively mild in severity. Obviously, inaccuracies and inconsistencies in diagnostic criteria will impede research on the outcomes of mild TBI.
Neurobehavioral Outcomes of Mild TBI
The outcomes of mild TBI in children and adolescents are controversial (McKinlay, 2009). Most previous studies have assessed outcomes in one of two ways, using performance-based tests of cognitive abilities or broad-based ratings of behavioral adjustment. Cognitive tests tend to be sensitive to mild TBI only acutely (Satz, 2001; Satz et al., 1997). Both epidemiological and clinical studies provide little evidence of persistent cognitive deficits resulting from mild TBI, especially in studies that are methodologically rigorous (e.g., Asarnow et al., 1995; Bijur & Haslum, 1995; Fay et al., 1993). Similar results have been obtained using broad-based measures of adjustment. However, the latter concern emotional and behavioral problems that often are not sensitive to medical disorders (Drotar, Stein, & Perrin, 1995) and do not focus on the somatic and cognitive symptoms that often occur following TBI (Yeates et al., 2001).
Few studies have focused specifically on what are commonly referred to as “postconcussive symptoms.” Postconcussive symptoms are complaints that tend to occur more often following TBI and include a range of somatic (e.g., headache, fatigue), cognitive (e.g., inattention, forgetfulness, slowed processing), and affective symptoms (e.g., irritability, disinhibition; Yeates et al., 1999). Although not specific to mild TBI, postconcussive symptoms are more common and severe in children with mild TBI than in children with injuries not involving the head or in healthy children matched for demographics (Barlow et al., in press; Hawley, 2003; Mittenberg, Wittner, & Miller, 1997; Ponsford et al., 1999; Taylor et al., 2010; Yeates et al., 1999, 2009). Postconcussive symptoms tend to be most pronounced shortly after injury and to resolve over time (Barlow et al. in press; Nacajauskaite et al., 2006; Ponsford et al., 1999; Taylor et al., 2010), but some children with mild TBI experience persistent symptoms, with potentially negative consequences for long-term psychosocial functioning (McKinlay et al., 2002; Overweg-Plandsoen et al., 1999; Yeates et al., 2009).
The persistent postconcussive symptoms that sometimes occur following mild TBI may constitute a coherent syndrome or disorder (Brown, Fann, & Grant, 1994). The diagnosis of post-concussion syndrome is included in the ICD-10 (World Health Organization, 1992) and research criteria for post-concussional disorder are contained in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 1994). However, the DSM-IV and ICD-10 have different diagnostic criteria, which make different underlying assumptions about the etiology of PCS, result in different incidence estimates, yield limited diagnostic agreement, and may not be specific to TBI (Boake et al., 2004, 2005; Yeates & Taylor, 2005). Recent research has shown that postconcussive symptoms form reliable and stable dimensions in children with mild TBI (Ayr et al., 2009), suggesting a potential basis for refining the symptom criteria for postconcussive syndrome in both the ICD and DSM-IV.
Postconcussive symptoms often occur in the absence of objective evidence of brain injury. This has engendered disputes about whether the etiology of PCS reflects “psychogenesis” or “physiogenesis” (Alexander, 1997; Bigler, 2008; Lishman, 1988). Proponents of “psychogenesis” argue that postconcussive symptoms reflect premorbid differences, post-injury psychological factors, or malingering in the context of litigation, rather than any alteration in brain function (Binder, 1986). In contrast, proponents of “physiogenesis” point to experimental studies of non-human animals and clinical research with humans suggesting that mild TBI can result in acute neuropathology and other abnormalities in brain function (Giza & Hovda, 2001). They also cite studies showing that postconcussive symptoms can be associated with deficits on standardized cognitive testing and abnormalities on neuroimaging (Levin et al., 2008; Wilde et al., 2008). Of course, these explanations are not mutually exclusive. Research is needed to identify both injury and non-injury related factors that predict persistent postconcussive symptoms (Satz, 2001; Yeates & Taylor, 2005). Indeed, research with adults shows that both injury characteristics and non-injury related variables help account for the outcomes of mild TBI (Kashluba, Paniak, & Casey, 2008; Luis, Vanderploeg, & Curtiss, 2003; Ponsford et al., 2000).
Conceptual and Methodological Issues in Research
Definition of mild TBI
The existing research on mild TBI suffers from a variety of methodological shortcomings (Dikman & Levin, 1993). One major limitation involves the definition of mild TBI (Williams, Levin, & Eisenberg, 1990), which has varied substantially across studies, along with associated inclusion/exclusion criteria. Most studies have defined mild TBI based on Glasgow Coma Scale (Teasdale & Jennett, 1974) scores ranging from 13 to 15, but they have been inconsistent in applying other criteria, such as presence or duration of unconsciousness or post-traumatic amnesia.
Studies can often be criticized for not defining both the lower and upper limits of severity of mild TBI. Many previous studies included children who sustained a head trauma without requiring any alternation in mental status or concussive symptoms associated with their injuries, and have excluded children with more severe injuries, including those with positive neuroimaging findings. These practices have engendered potentially erroneous conclusions about the outcomes of mild TBI. The WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury reviewed the prognosis of mild TBI (Carroll et al., 2004b) and cited two studies to justify their conclusion that PCS in children “… are usually transient in nature” (p. 88) and “… appear to be largely resolved within 2–3 months of the injury” (p. 85). However, both studies excluded children with so-called “complicated” mild TBI. Studies including children with more severe injuries have found more pronounced and persistent postconcussive symptoms as compared to children with orthopedic injuries or healthy children (Fay et al., 2003; Mittenberg, Williams, & Miller, 1997; Taylor et al., 2010; Yeates et al., 2009).
Comparison groups
Previous studies can be criticized for the absence of appropriate comparison groups (Dikman & Levin, 1993). Many early studies did not include comparison groups, relying on normative data to determine the effects of mild TBI. More recently, non-injured children matched on demographic variables have been used as a comparison group (e.g., Fay et al., 1993). However, non-injured children are not equated to children with mild TBI in terms of the experience of a traumatic injury or ensuing medical treatment. Research also suggests that children who sustain traumatic injuries are more likely to display premorbid behavioral disorders and differ in other ways from non-injured children (Gerring et al., 1998; McKinlay et al., 2010).
In one of the larger studies of mild TBI (Asarnow, et al., 1995; Light et al., 1998), the cognitive test performance of children with mild TBI was worse than that of children who were matched demographically but not injured. In contrast, the cognitive and behavioral functioning of children with mild TBI did not differ from that of children with injuries not involving the head. Comparison groups comprised of children who have sustained mild injuries not involving the head and undergone acute medical treatment are desirable in research on mild TBI.
Outcome measurement
The measurement of postconcussive symptoms has typically been limited to questionnaires and rating scales, almost always completed only by parents. Parent-child agreement regarding postconcussive symptoms is significant but modest (Gioia et al., 2009; Hajek et al., in press), suggesting that both child and parents reports should be explored in studies of mild TBI. The reporting of postconcussive symptoms may also depend on the format for symptom reporting (i.e., questionnaire/rating scale vs. structured interview); however, the author is not aware of any structured interview that is intended specifically to assess postconcussive symptoms.
Previous research has also treated postconcussive symptoms as if they occur along a single dimension. However, research indicates that postconcussive symptoms are multidimensional, with a clear distinction being able to be drawn between somatic and cognitive symptoms (Ayr et al., 2009). The dimensions not only can be distinguished psychometrically, but also follow distinct trajectories following mild TBI (Taylor et al., 2010).
Assessment of risk factors
The assessment of risk factors that predict outcomes following mild TBI has been problematic. Most studies have not adequately characterized the severity of children’s injuries. Children with mild TBI are often treated as a homogenous group, without regard to whether factors such as loss of consciousness or abnormalities on neuroimaging increase the risk of negative outcomes. Few studies have explored existing schemes for grading mild TBI, such as those set forth by the American Academy of Neurology (1997) for the management of sports concussions.
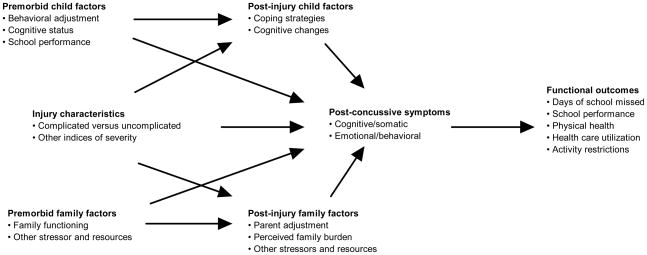
Research also needs to incorporate measures of non-injury related risk factors as possible predictors of postconcussive symptoms. In many cases, children with premorbid learning or behavior problems are omitted from studies, despite the possibility that they are most at risk for persistent postconcussive symptoms. We recently showed that children’s premorbid cognitive ability moderates the outcomes of mild TBI (Fay et al., 2009). Parent and family functioning also can be affected by mild TBI (Ganesaglinam et al., 2008), and may moderate outcomes, as it does in children with more severe TBI (Yeates et al., 1997). In the long run, models are needed that capture the interplay of injury-related and non-injury related child and family factors in predicting post-concussive symptoms (see Figure 1).
Figure 1.
Model for study of postconcussive symptoms in children with mild traumatic brain injury (reprinted from Yeates & Taylor, 2005).
Timing of assessment
Research on mild TBI has often been cross-sectional and focused on relatively short-term outcomes. Longitudinal studies are needed to examine the sequelae of mild TBI over time, as well as how the relationship of risk factors to post-concussive symptoms varies post-injury. (Ponsford et al., 1999). In longitudinal studies, decisions regarding the timing of assessments are critical (Taylor & Alden, 1997). Acute post-injury assessments are often desirable, not only to document the acute effects of mild TBI, but also to obtain retrospective measures of children’s premorbid functioning. The timing of subsequent assessments is likely to reflect assumptions about variations in outcomes following mild TBI. The DSM-IV criteria for postconcussive syndrome, for instance, require that symptoms persist for at least 3 months, so an assessment at that time is often desirable (American Psychiatric Association, 1994). However, even longer-term assessments may be needed to determine whether mild TBI results in significant impairment in children’s social or academic functioning.
Prediction of individual outcomes
Studies of the outcomes of mild TBI have focused on group outcomes, in part because most common statistical techniques yield results that are based on group data. Thus, most analyses are variable-centered. In clinical practice, however, we are interested in knowing whether the occurrence of mild TBI accounts for postconcussive symptoms in a particular patient, because we recognize that the importance of risk factors is likely to vary across individuals. Research on mild TBI should examine individual variations in the outcomes of mild TBI in relation to specific risk factors, by incorporating alternative statistical methods that reflect a person-centered approach (Laursen & Hoff, 2006).
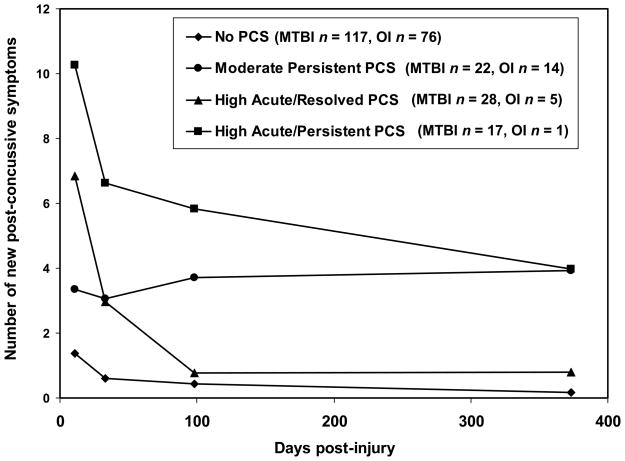
Growth curve modeling permits the investigation of change at an individual level (Francis et al., 1991). Mixture modeling also can be used to examine intraindividual change, by empirically identifying latent classes of individuals based on different developmental trajectories (Nagin, 2005). Figure 2 provides an example of this approach; it shows distinct developmental trajectories of post-concussive symptoms in children with mild TBI (Yeates et al., 2009). In this study, children with mild TBI were more likely than those with orthopedic injuries to demonstrate the two trajectories involving high acute levels of symptoms, and the differences were particularly pronounced for children whose acute clinical presentation reflected more severe injury. Finally, analyses of reliable change also can be used to identify individual children who display unusually large increases in postconcussive symptoms and to study the risk factors associated with such increases (McCrea et al., 2005).
Figure 2.
Illustration of developmental trajectory analysis of postconcussive symptoms in children with mild TBI and orthopedic injuries (reprinted from Yeates et al., 2009).
Future Research Directions
Future research on mild TBI in children should reflect advances in our understanding of biological, psychological, and social factors that affect outcomes. At the biological level, genetic factors may help to account for variability in outcomes. The apolipoprotetin E gene has not been found to be associated with the outcomes of mild TBI in children (Moran et al., 2009), but many other candidate genes should be examined (Jordan, 2007). Research at a biological level also is likely to yield more sensitive measures of brain injury. For instance, various biomarkers are under study as possible indicators of underlying brain injury in mild TBI (Berger et al., 2010). Advanced neuroimaging techniques, such as susceptibility-weighted and diffusion tensor imaging, may also provide a more sensitive assessment of mild TBI (Ashwal et al., 2010).
At the psychological level, future research may offer more refined and sensitive measures of cognitive functioning in mild TBI. Computerized testing has the advantage of being able to assess reaction time, which has been shown to be sensitive to concussion (Iverson et al., 2006). Existing measures of postconcussive symptoms are also in need of additional refinement, so that they accurately reflect underlying dimensions of symptom type (Ayr et al., 2009). Ideally, screening instruments could be developed that physicians in emergency department and outpatient settings can use to assess children with mild TBI to determine whether to refer for more extensive neuropsychological evaluation (Gioia, Collins, & Isquith, 2008).
Finally, at a social level, research is needed to clarify which aspects of the family and broader social environment influence outcomes and to delineate the mechanisms by which they do so (Rutter, 1999). Recent studies have shown that the family and social environment are related to children’s functioning following TBI (Yeates et al., 1997). Future research will benefit from the consideration of more sophisticated models of the relationship between contextual factors and developmental outcomes (Steinberg & Avenevoli, 2000).
A key long-term goal for research on the outcomes of mild TBI should be to develop a biopsychosocial model that incorporates developmental considerations and allows for individual variability in the importance of different risk factors. A comprehensive, integrated model should provide a clearer picture of risk and resiliency in children with mild TBI, and thereby foster more effective clinical management (Kirkwood et al., 2008). For instance, research has shown that the provision of anticipatory guidance can prevent the onset of postconcussive symptoms (Ponsford et al., 2001) and that active rehabilitation can ameliorate postconcussive symptoms when they do occur (Gagnon et al., 2009). Future research will enable health care providers to provide parents and children with accurate and useful information regarding the effects of mild TBI and to identify those children who are most at risk for demonstrating negative outcomes. Health care providers can then target at-risk children and their families for appropriate management.
Acknowledgments
This work was supported by grants HD44099 and HD39834 from the National Institutes of Health to the author.
References
- Alexander MP. Minor traumatic brain injury: A review of physiogenesis and psychogenesis. Seminars in Clinical Neuropsychiatry. 1997;2:177–187. doi: 10.1053/SCNP00200177. [DOI] [PubMed] [Google Scholar]
- American Academy of Neurology. Practice parameter: The management of concussion in sports (summary statement). Report of the Quality Standards Subcommittee. Neurology. 1997;48:581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. The management of minor closed head injury in children. Pediatrics. 1999;104:1407–1415. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Asarnow RF, Satz P, Light R, Zaucha K, Lewis R, McCleary C. The UCLA study of mild head injury in children and adolescents. In: Michel ME, Broman S, editors. Traumatic head injury in children. New York: Oxford University Press; 1995. pp. 117–146. [Google Scholar]
- Ashwal S, Tong KA, Obenaus A, Holshouser BA. Advanced neuroimaging techniques in children with traumatic brain injury. In: Anderson VA, Yeates KO, editors. New directions in pediatric traumatic brain injury: Multidisciplinary and translational perspectives. New York: Oxford University Press; 2010. pp. 68–93. [Google Scholar]
- Ayr LK, Yeates KO, Taylor HG, Browne M. Dimensions of post-concussive symptoms in children with mild traumatic brain injuries. Journal of the International Neuropsychological Society. 2009;15:19–30. doi: 10.1017/S1355617708090188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow KM, Crawford S, Stevenson A, Sandhu SS, Belanger F, Dewey D. A prospective epidemiological study of post-concussion syndrome in pediatric mild traumatic brain injury. Pediatrics. doi: 10.1542/peds.2009-0925. in press. [DOI] [PubMed] [Google Scholar]
- Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998–2000. Brain Injury. 2005;19:85–91. doi: 10.1080/02699050410001720158. [DOI] [PubMed] [Google Scholar]
- Berger RP, Hayes RL, Wang KKW, Kochanek P. Using serum biomarkers to diagnose, assess, treat and predict outcome after pediatric TBI. In: Anderson VA, Yeates KO, editors. New directions in pediatric traumatic brain injury: Multidisciplinary and translational perspectives. New York: Oxford University Press; 2010. pp. 36–53. [Google Scholar]
- Bigler ED. Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. Journal of the International Neuropsychological Society. 2008;14:1–22. doi: 10.1017/S135561770808017X. [DOI] [PubMed] [Google Scholar]
- Bijur PE, Haslum M. Cognitive, behavioral, and motoric sequelae of mild head injury in a national birth cohort. In: Broman S, Michel ME, editors. Traumatic head injury in children. Oxford University Press; 1995. pp. 147–164. [Google Scholar]
- Binder LM. Persisting symptoms after mild head injury: A review of the postconcussive syndrome. Journal of Clinical and Experimental Neuropsychology. 1986;8:323–346. doi: 10.1080/01688638608401325. [DOI] [PubMed] [Google Scholar]
- Boake C, McCauley SR, Levin HS, Contant CF, Song JX, Brown SA, Merritt SG. Limited agreement between criteria-based diagnoses of Postconcussional syndrome. Journal of Neuropsychiatry and Clinical Neurosciences. 2004;16:493–499. doi: 10.1176/jnp.16.4.493. [DOI] [PubMed] [Google Scholar]
- Boake C, McCauley SR, Levin HS, Pedroza C, Contant CF, Song JX, Diaz-Marchan PJ. Diagnostic criteria for Postconcussional syndrome after mild to moderate traumatic brain injury. Journal of Neuropsychiatry and Clinical Neurosciences. 2005;17:350–356. doi: 10.1176/jnp.17.3.350. [DOI] [PubMed] [Google Scholar]
- Bodin D, Yeates KO, Klamar K. Definition and classification of concussion. In: Apps JN, Walter K, editors. Handbook of pediatric concussion. New York: Guilford Press; in press. [Google Scholar]
- Bowman SM, Bird TM, Aitken ME, Tilford JM. Trends in hospitalizations associated with pediatric traumatic brain injuries. Pediatrics. 2008;122:988–993. doi: 10.1542/peds.2007-3511. [DOI] [PubMed] [Google Scholar]
- Brown SJ, Fann JR, Grant I. Postconcussional disorder: Time to acknowledge a common source of neurobehavioral morbidity. The Journal of Neuropsychiatry and Clinical Neurosciences. 1994;6:15–22. doi: 10.1176/jnp.6.1.15. [DOI] [PubMed] [Google Scholar]
- Carroll LJ, Cassidy JD, Holm L, Kraus J, Coronado VG. Methodological issues and research recommendations for mild traumatic brain injury: The WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine. 2004a;Suppl 43:113–125. doi: 10.1080/16501960410023877. [DOI] [PubMed] [Google Scholar]
- Carroll LJ, Cassidy JD, Peloso PM, Borg J, von Holst H, Holm L, Paniak C, Pépin M. Prognosis for mild traumatic brain injury: Results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine. 2004b;Suppl 43:84–105. doi: 10.1080/16501960410023859. [DOI] [PubMed] [Google Scholar]
- Dikman SS, Levin HS. Methodological issues in the study of mild head injury. Journal of Head Trauma Rehabilitation. 1993;8:30–37. [Google Scholar]
- Drotar D, Stein REK, Perrin EC. Methodological issues in using the Child Behavior Checklist and its related instruments in clinical child psychology research. Journal of Clinical Child Psychology. 1995;24:184–192. [Google Scholar]
- Fay GC, Jaffe KM, Polissar NL, Liao S, Martin KM, Shurtleff HA, Rivara JB, Winn JR. Mild pediatric traumatic brain injury: A cohort study. Archives of Physical Medicine and Rehabilitation. 1993;74:895–901. [PubMed] [Google Scholar]
- Fay TB, Yeates KO, Taylor HG, Bangert B, Dietrich A, Nuss KE, Rusin J, Wright M. Cognitive reserve as a moderator of postconcussive symptoms in children with complicated and uncomplicated mild traumatic brain injury. Journal of the International Neuropsychological Society. 2009;16:94–105. doi: 10.1017/S1355617709991007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis DJ, Fletcher JM, Stuebing KK, Davidson KC, Thompson NM. Analysis of change: Modeling individual growth. Journal of Consulting and Clinical Psychology. 1991;59:27–37. doi: 10.1037//0022-006x.59.1.27. [DOI] [PubMed] [Google Scholar]
- Gagnon I, Galli C, Friedman D, Grilli L, Iverson GL. Active rehabilitation for children who are slow to recover following sport-related concussion. Brain Injury. 2009;23:956–964. doi: 10.3109/02699050903373477. [DOI] [PubMed] [Google Scholar]
- Ganesalingam K, Yeates KO, Ginn MS, Taylor HG, Dietrich A, Nuss K, Wright M. Family burden and parental distress following mild traumatic brain injury in children and its relationship to post-concussive symptoms. Journal of Pediatric Psychology. 2008;33:621–629. doi: 10.1093/jpepsy/jsm133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerring JP, Brady KD, Chen A, Vasa R, Grados M, Bandeen-Roche KJ, Bryan N, Denckla MB. Premorbid prevalence of ADHD and development of secondary ADHD after closed head injury. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:647–654. doi: 10.1097/00004583-199806000-00015. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Collins M, Isquith PK. Improving identification and diagnosis of mild traumatic brain injury with evidence: Psychometric support for the Acute Concussion Evaluation. Journal of Head Trauma Rehabilitation. 2008;23:230–242. doi: 10.1097/01.HTR.0000327255.38881.ca. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Schneider JC, Vaughan CG, Isquith PK. Which symptom assessments and approaches are uniquely appropriate for paediatric concussion? British Journal of Sports Medicine. 2009;43(Suppl I):i13–i22. doi: 10.1136/bjsm.2009.058255. [DOI] [PubMed] [Google Scholar]
- Giza CC, Hovda DA. The neurometabolic cascade of concussion. Journal of Athletic Training. 2001;36:228–235. [PMC free article] [PubMed] [Google Scholar]
- Hajek CA, Yeates KO, Taylor HG, Bangert B, Dietrich A, Nuss KE, Rusin J, Wright M. Agreement between parents and children on ratings of postconcussive symptoms following mild traumatic brain injury. Child Neuropsychology. doi: 10.1080/09297049.2010.495058. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawley CA. Reported problems and their resolution following mild, moderate, and severe traumatic brain injury amongst children and adolescents in the UK. Brain Injury. 2003;17:105–129. doi: 10.1080/0269905021000010131. [DOI] [PubMed] [Google Scholar]
- Iverson GL, Brooks BL, Collins MW, Lovell MR. Tracking neuropsychological recovery following concussion in sport. Brain Injury. 2006;20:245–252. doi: 10.1080/02699050500487910. [DOI] [PubMed] [Google Scholar]
- Jordan BD. Genetic influences on outcome following traumatic brain injury. Neurochemical Research. 2007;32:905–915. doi: 10.1007/s11064-006-9251-3. [DOI] [PubMed] [Google Scholar]
- Kashluba S, Paniak C, Casey JE. Persistent symptoms associated with factors identified by the WHO Task Force on Mild Traumatic Brain Injury. The Clinical Neuropsychologist. 2008;22:195–208. doi: 10.1080/13854040701263655. [DOI] [PubMed] [Google Scholar]
- Kirkwood MW, Yeates KO, Taylor HG, Randolph C, McCrea M, Anderson VA. Management of pediatric mild traumatic brain injury: A neuropsychological review from injury through recovery. The Clinical Neuropsychologist. 2008;22:769–800. doi: 10.1080/13854040701543700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus JF. Epidemiological features of brain injury in children: Occurrence, children at risk, causes and manner of injury, severity, and outcomes. In: Broman SH, Michel ME, editors. Traumatic head injury in children. New York: Oxford University Press; 1995. pp. 22–39. [Google Scholar]
- Laursen B, Hoff E. Person-centered and variable-centered approaches to longitudinal data. Merrill-Palmer Quarterly. 2006;52:377–389. [Google Scholar]
- Levin HS, Hanten G, Roberson G, Li X, Ewing-Cobbs L, Dennis M, Chapman S, Max JE, Hunter J, Schachar R, Luerssen TG, Swank P. Prediction of cognitive sequelae based on abnormal computed tomography findings in children following mild traumatic brain injury. Journal of Neursurgery: Pediatrics. 2008;1:461–470. doi: 10.3171/PED/2008/1/6/461. [DOI] [PubMed] [Google Scholar]
- Light R, Asarnow R, Satz P, Zucha K, McCleary C, Lewis R. Mild closed-head injury in children and adolescents: Behavior problems and academic outcomes. Journal of Consulting and Clinical Psychology. 1998;66:1023–1029. doi: 10.1037//0022-006x.66.6.1023. [DOI] [PubMed] [Google Scholar]
- Lishman WA. Physiogenesis and psychogenesis in the post-concussion syndrome. British Journal of Psychiatry. 1988;153:460–469. doi: 10.1192/bjp.153.4.460. [DOI] [PubMed] [Google Scholar]
- Luis CA, Vanderploeg RD, Curtiss G. Predictors of postconcussion symptom complex in community dwelling male veterans. Journal of the International Neuropsychological Society. 2003;9:1001–1015. doi: 10.1017/S1355617703970044. [DOI] [PubMed] [Google Scholar]
- McCrea M, Barr WB, Guskiewicz K, Randolph C, Marshall SW, Cantu R, Onate JA, Kelly JP. Standard regression-based methods for measuring recovery after sport-related concussion. Journal of the International Neuropsychological Society. 2005;11:58–69. doi: 10.1017/S1355617705050083. [DOI] [PubMed] [Google Scholar]
- McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, Cantu R. Consensus statement on concussion in sport 3rd International Conference on Concussion in Sport Held in Zurich, November 2008. Clinical Journal of Sports Medicine. 2009;19:185–195. doi: 10.1136/bjsm.2009.058248. [DOI] [PubMed] [Google Scholar]
- McKinlay A. Controversies and outcomes associated with mild traumatic brain injury in childhood and adolescence. Child: care, health, and development. 2009;36:3–21. doi: 10.1111/j.1365-2214.2009.01006.x. [DOI] [PubMed] [Google Scholar]
- McKinlay A, Dalrymple-Alford JC, Horwood LJ, Fergusson DM. Long term psychosocial outcomes after mild head injury in early childhood. Journal of Neurology, Neurosurgery, and Psychiatry. 2002;73:281–288. doi: 10.1136/jnnp.73.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinlay A, Kyonka EGE, Grace RC, Horwood LJ, Fergusson DM, MacFarlane MR. An investigation of the pre-injury risk factors associated with children who experience traumatic brain injury. Injury Prevention. 2010;16:31–35. doi: 10.1136/ip.2009.022483. [DOI] [PubMed] [Google Scholar]
- Mild Traumatic Brain Injury Committee of the Head Injury Interdisciplinary Special Interest Group of the American Congress of Rehabilitation Medicine. Definition of mild traumatic brain injury. Journal of Head Trauma Rehabilitation. 1993;8:86–87. [Google Scholar]
- Mittenberg W, Wittner MS, Miller LJ. Postconcussion syndrome occurs in children. Neuropsychology. 1997;11:447–452. doi: 10.1037//0894-4105.11.3.447. [DOI] [PubMed] [Google Scholar]
- Moran LM, Taylor HG, Ganesalingam K, Gastier-Foster JM, Frick J, Bangert B, Dietrich A, Nuss KE, Rusin J, Wright M, Yeates KO. Apolipoprotein E4 as a predictor of outcomes in pediatric mild traumatic brain injury. Journal of Neurotrauma. 2009;26:1489–1495. doi: 10.1089/neu.2008.0767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Injury Prevention and Control. Report to Congress on mild traumatic brain injury in the United States: Steps to prevent a serious public health problem. Atlanta: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- Nacajauskaite O, Endziniene M, Jureniene K, Schrader H. The validity of post-concussion syndrome in children: A controlled historical cohort study. Brain and Development. 2006;28:507–514. doi: 10.1016/j.braindev.2006.02.010. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- NIH Consensus Panel on Rehabilitation of Persons with Traumatic Brain Injury. Rehabilitation of persons with traumatic brain injury. Journal of the American Medical Association. 1999;282:974–983. [Google Scholar]
- Overweg-Plandsoen WCG, Kodde A, van Straaten M, van der Linden EAM, Neyens LGJ, Aldenkamp AP, Vermeulen M. Mild closed head injury in children compared to traumatic fractured bone; neurobehavioural sequelae in daily life 2 years after the accident. European Journal of Pediatrics. 1999;158:249–252. doi: 10.1007/s004310051061. [DOI] [PubMed] [Google Scholar]
- Ponsford J, Willmott C, Rothwell A, Cameron P, Ayton G, Nelms R, Curran C, Ng KT. Cognitive and behavioral outcomes following mild traumatic head injury in children. Journal of Head Trauma Rehabilitation. 1999;14:360–372. doi: 10.1097/00001199-199908000-00005. [DOI] [PubMed] [Google Scholar]
- Ponsford J, Willmott C, Rothwell A, Cameron P, Ayton G, Nelms R, Curran C, Ng K. Impact of early intervention on outcome after mild traumatic brain injury in children. Pediatrics. 2001;108:1297–1303. doi: 10.1542/peds.108.6.1297. [DOI] [PubMed] [Google Scholar]
- Ponsford J, Willmott C, Rothwell A, Cameron P, Kelly AM, Nelms R, Curran C, Ng K. Factors influencing outcome following mild traumatic brain injury in adults. Journal of the International Neuropsychological Society. 2000;6:568–579. doi: 10.1017/s1355617700655066. [DOI] [PubMed] [Google Scholar]
- Powell JM, Ferraro JV, Dikmen SS, Temkin NR, Bell KR. Accuracy of mild traumatic brain injury diagnosis. Archives of Physical Medicine and Rehabilitation. 2008;89:1550–1555. doi: 10.1016/j.apmr.2007.12.035. [DOI] [PubMed] [Google Scholar]
- Rutter ML. Psychosocial adversity and child psychopathology. British Journal of Psychiatry. 1999;174:480–493. doi: 10.1192/bjp.174.6.480. [DOI] [PubMed] [Google Scholar]
- Satz P. Mild head injury in children and adolescents. Current Directions in Psychological Science. 2001;10:106–109. [Google Scholar]
- Satz P, Zaucha K, McCleary C, Light R, Asarnow R. Mild head injury in children and adolescents: A review of studies (1970–1995) Psychological Bulletin. 1997;122:107–131. doi: 10.1037/0033-2909.122.2.107. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Avenevoli S. The role of context in the development of psychopathology: A conceptual framework and some speculative propositions. Child Development. 2000;71:66–74. doi: 10.1111/1467-8624.00119. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Alden J. Age-related differences in outcome following childhood brain injury: An introduction and overview. Journal of the International Neuropsychological Society. 1997;3:555–567. [PubMed] [Google Scholar]
- Taylor HG, Dietrich A, Nuss K, Wright M, Rusin J, Bangert B, Yeates KO. Post-concussive symptoms in children with mild traumatic brain injury. Neuropsychology. 2010;24:148–159. doi: 10.1037/a0018112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness: A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Williams DH, Levin HS, Eisenberg HM. Mild head injury classification. Neurosurgery. 1990;27:422–428. doi: 10.1097/00006123-199009000-00014. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- Yeates KO, Luria J, Bartkowski H, Rusin J, Martin L, Bigler ED. Post-concussive symptoms in children with mild closed-head injuries. Journal of Head Trauma Rehabilitation. 1999;14:337–350. doi: 10.1097/00001199-199908000-00003. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG. Neurobehavioural outcomes of mild head injury in children and adolescents. Pediatric Rehabilitation. 2005;8:5–16. doi: 10.1080/13638490400011199. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Barry CT, Drotar D, Wade SL, Stancin T. Neurobehavioral symptoms in childhood closed-head injuries: Changes in prevalence and correlates during the first year post injury. Journal of Pediatric Psychology. 2001;26:79–91. doi: 10.1093/jpepsy/26.2.79. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Drotar D, Wade SL, Klein S, Stancin T, Schatschneider C. Pre-injury family environment as a determinant of recovery from traumatic brain injuries in school-age children. Journal of the International Neuropsychological Society. 1997;3:617–630. [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Rusin J, Bangert B, Dietrich A, Nuss K, Wright M, Nagin DS, Jones BL. Longitudinal trajectories of post-concussive symptoms in children with mild traumatic brain injuries and their relationship to acute clinical status. Pediatrics. 2009;123:735–743. doi: 10.1542/peds.2008-1056. [DOI] [PMC free article] [PubMed] [Google Scholar]