Previous research has compared physicians' use of electronic resources [1–3], use of MEDLINE search features [4], preferred source type for clinical information [4–6], perceived barriers to accessing information for patient care in specific countries [1, 7, 8], attitudes toward evidence-based medicine (EBM) [9, 10], and understanding of EBM terms [9, 10]. These published research papers were included in a review by Davies [11] of the evidence on the information-seeking behavior of doctors, during which comparison across different countries was identified as an area needing further research. The study reported here compares these aspects, focusing on EBM resources across three countries: Canada, the United Kingdom, and the United States.
METHODOLOGY
An online questionnaire (Appendix, online only) was utilized to determine the information needs and the use of EBM resources by qualified physicians in these three countries. The questionnaire was designed by the author and piloted as a Microsoft Word document on three medical librarians, two nurses, and three doctors (two general practitioners and one consultant; all recently retired) prior to the uniform resource locator (URL) being released. SurveyMonkey hosted this online questionnaire [12]. The survey questions covered the topics of physicians' information needs; use of technologies and electronic EBM resources; attitudes toward and understanding of EBM; and barriers to accessing health information.
As part of the author's doctoral thesis, the survey was administered to physicians in the United Kingdom from December 2006 to May 2007 [13]. To compare responses with physicians in Canada and the United States, the same survey was promoted to physicians in these countries from March to May 2007. The email addresses of physicians in Canada, the United States, and the United Kingdom were identified from websites, and an email inviting them to complete the questionnaire was sent to each. Medical websites were identified through a general Internet search and then individually searched for the email contact details of physicians (Table 1, online only). Emails were sent to all the physicians listed on the websites who had active, current email addresses. The emails explained that these data were being collected for a doctoral thesis and were intended to be published in a peer-reviewed journal. There was no incentive offered to encourage completion of the questionnaire. There was no method for determining who responded to the emails, as the questionnaire responses were anonymous. This meant there was no opportunity to send out second follow-up reminder emails. The larger concurrent survey in the United Kingdom received 636 completed questionnaires, so an online research randomizer [14] was utilized to select 80 responses.
The data were analyzed using Excel. Ethical approval was obtained from Loughborough University.
RESULTS
Four hundred and ninety-eight emails were delivered to US physicians and 416 to Canadian physicians. Eighty responses were received from both US and Canadian physicians, which was a response rate of 16% and 19%, respectively. In the United Kingdom, 2,351 emails were delivered, with 636 questionnaires completed, representing an approximate response rate of 27%.
The percentages of responses from physicians working in general practice were similar for 2 of the countries: 31.30% for the United Kingdom and 32.50% Canadian responses, but 30.00% of the US responses were from physicians in general practice and 12.50% from family medicine specialists (which is a term not used in the United Kingdom). The remaining responses were evenly distributed among the medical specialties listed on the questionnaire, though both Canada and the United States had 6.25% “other” responses, possibly due to the different terminologies utilized in the United Kingdom.
Significant numbers of UK and Canadian physicians responded that they never used electronic resources for diagnosis, 20.0% and 13.8%, respectively, compared to 1.3% of US physicians.
Physicians in the United States were twice as likely to report using electronic resources to locate information on treatment options for common diseases “all the time” compared to UK physicians (31.3% compared to 15.0%) and 3 times as likely to report locating information on rare diseases and syndromes using electronic resources “all the time” (56.3% compared to 18.8%). Physicians in the United States used electronic resources for patient information more frequently (United States 26.3% all the time, Canada and United Kingdom 15.0%).
US physicians used electronic resources for research more (United States 51.3% all the time, Canada 47.5%, and United Kingdom 26.3%). Physicians utilized electronic resources for teaching in a similar pattern (United States 55.0% all the time, Canada 32.5%, and United Kingdom 22.5%).
The only information use for electronic resources that was similar for all countries was continuing professional development (CPD). Approximately 30% of physicians in all 3 countries used electronic resources “all the time,” and more than 50% “sometimes” used electronic resources to update their knowledge and/or skills.
Comparing the reported frequency of searching by country, US and UK physicians reported almost opposite patterns of use. More than a quarter (27.5%) of US physicians responded that they formulated specific questions that required searching external evidence less than once a week, whilst for British physicians, the response was 71.3%. Conversely, compared to UK physicians (28.8%), twice the number of Canadian physicians (56.3%), and even more from the United States (72.5%), searched the literature electronically at least once a week.
Physicians were asked their level of awareness and understanding of specific terms used in journal papers about EBM, such as relative risk, systematic review, confidence interval, and publication bias. The responses from the different countries were similar with more than 70% (range of 71%–77%) reporting understanding or being able to explain the EBM concepts. The physicians' responses agreeing with the EBM statements (such as “EBM is a good concept that fails in practice” and “The whole medical information ‘explosion’ is overwhelming”) were also similar when comparing the 3 countries.
All the respondents reported similar use of networked computers. However, physicians in the United States (43.8%) and Canada (40.0%) were more than twice as likely to currently use wireless laptop computers compared to those in the United Kingdom (18.8%). Canadian physicians (51.3%) and US physicians (41.3%) were also more than twice as likely to currently use personal digital assistants (PDAs) compared to UK physicians (16.3%).
Respondents were asked to identify the search features they regularly used when searching MEDLINE/PubMed. Applying limits (such as English language, human subjects only, date of publication) was used by US physicians 57.5%, Canadian physicians 55.0%, and UK physicians 42.5% of the time. Combining 2 concepts using a Boolean “AND” was used by US physicians 82.5%, Canadian physicians 77.5%, and UK physicians 67.5% of the time. Medical Subject Headings (MeSH) were used by US physicians 46.3%, Canadian physicians 43.9%, and UK physicians 32.5% of the time. The “related articles” or “similar titles” facility was used by US physicians 78.8%, Canadian physicians 72.5%, and UK physicians 62.5% of the time. Physicians in the United States used all of these features more than those in Canada, whilst Canadian physicians used them more than British physicians.
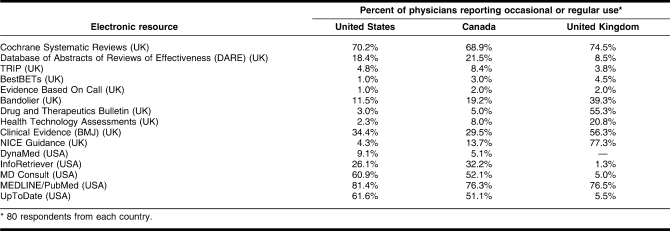
Table 2 shows the responses to use of particular EBM resources; “occasionally” and “regularly” responses are combined. Even though the Database of Abstracts of Reviews of Effectiveness (DARE) and TRIP are produced in the United Kingdom, more Canadian and US physicians reported using these resources than UK physicians. The UK resources Bandolier, Drug and Therapeutics Bulletin, Health Technology Assessments, Clinical Evidence (BMJ), and NICE Guidance were used more by physicians based in the United Kingdom. The most frequently used subscription-based electronic resources were UpToDate and MD Consult. These resources were used more often by physicians from the United States and Canada, compared to those in the United Kingdom. MEDLINE/PubMed was the most frequently used resource for all physicians.
Table 2.
Comparison of British and US produced electronic evidence-based medicine (EBM) resources used by physicians
Physicians were asked to rank in order of importance the aids they used in clinical decision making (textbooks or journals in paper format; full-text electronic journals; EBM resources; colleagues; and other health professionals, such as pharmacists). US and Canadian physicians ranked electronic full-text journals first, whilst the UK physicians ranked these third. UK physicians preferred using colleagues to assist in their clinical decision making (which was ranked fourth by US and Canadian physicians).
Physicians ranked five barriers to accessing electronic information, and the top three responses were the same for each country. In order, these were the time it takes to search, too much information that is not clinically relevant, and lack of easy access to electronic resources.
LIMITATIONS OF THE STUDY
An issue with any generic questionnaire is that the variations in terminologies between different countries are not addressed. For example, the questionnaire used in this research referred to medical specialisms (UK) rather than medical specialties (US). The small number of responses from each country prohibited analysis by year of medical school graduation or medical specialty.
There were several differences in resource availability that may also have affected the results. In the United Kingdom, the National Health Service (NHS) provides the information technology devices for health care staff, and these are usually personal computers, not laptops. In addition, NHS Evidence [15] provides standardized access to NHS Athens resources that are centrally purchased for NHS staff. UpToDate and MD Consult had low reported use in the United Kingdom, but neither is included in the centrally funded package. This lack of use is not really surprising; physicians are probably more likely to use first those resources that they are aware of and that are readily and freely available to them.
Finally, it is worth noting that the questionnaire only asked for use of electronic information resources. There is a possible bias toward respondents who are comfortable and skilled in the use of information technology due to the sampling method utilized in this study, because respondents needed to have an active email account and be willing (and able) to answer an online questionnaire.
DISCUSSION
Canadian and UK physicians might be using paper-based information sources, while US physicians might have embraced electronic resources to a greater extent. The US and Canadian physicians reported searching electronic resources more frequently than UK physicians. Physicians in the United States also reported using the search features on MEDLINE/PubMed more than Canadian physicians, who, in turn, reported using them more than UK physicians. UK physicians preferred to use colleagues to assist in their clinical decision making, while US and Canadian physicians preferred to use electronic full-text journals. The findings of a 2007 publication based on research in the United States found the questions from medical students (who are less experienced than the physicians in this research) were more frequently answered by attending physicians [6].
In research undertaken in 2001, New Zealand physicians ranked text books first and specialists and colleagues second [4], while a 2005 study of pediatricians in the United States ranked specialists first, textbooks second, and electronic resources third [5].
Previous Australasian research found the most frequently used evidence source was MEDLINE (76%), followed by Cochrane Library (17%) [1], whilst a US study found the Cochrane Library was rarely used [2]. In this research, the Cochrane resource was the second most frequently used resource, coming right after MEDLINE/PubMed among physicians in all countries.
A British study found that physicians preferred UK drug resources to those produced in the United States [16]. This is not surprising as the drugs prescribed for use in the two countries can be very different. It is then worth considering if producer's location affects other EBM resources because, in this study, UK physicians were generally less likely to know about US-produced resources.
The time it takes to search is still the main barrier to accessing electronic information. This finding reflects previous research [1, 7, 8].
CONCLUSION
Generally, physicians in the United States (and Canada) were more likely to use electronic resources to locate information compared to physicians based in the United Kingdom. However, there was a distinct cultural bias, with physicians often preferring to utilize resources created in their country. The major barrier to using electronic resources for health information is still time.
The results from this research and range of results from previous research suggest that comparing physicians' use of information and information resources in different countries is an area where further investigation is required before in-depth conclusions can be drawn.
Electronic Content
Footnotes
REFERENCES
- 1. Scott I, Heyworth R, Fairweather P. The use of evidence-based medicine in the practice of consultant physicians. results of a questionnaire survey. Aust N Z J Med. 2000 Jun;30(3):319–26. doi: 10.1111/j.1445-5994.2000.tb00832.x. [DOI] [PubMed] [Google Scholar]
- 2. Ramos K, Linscheid R, Schafer S. Real-time information-seeking behaviour of residency physicians. Fam Med. 2003 Apr;35(4):257–60. [PubMed] [Google Scholar]
- 3. Wong K, Veness M.J. Internet access, awareness and utilisation of web-based evidence: a survey of Australian, New Zealand and Singaporean radiation oncology registrars. Asia Pac J Clin Oncol. 2005 Dec;1(4):120–7. [Google Scholar]
- 4. Cullen R.J. In search of evidence: family practitioners' use of the Internet for clinical information. J Med Libr Assoc. 2002 Oct;90(4):370–9. [PMC free article] [PubMed] [Google Scholar]
- 5. Kim G.R, Bartlett E.I, Jr, Lehmann H.P. Information resource preferences by general paediatricians in office settings: a qualitative study. BMC Med Inform Decis Mak [Internet] 2005 Oct;5(34) doi: 10.1186/1472-6947-5-34. [cited 17 May 2006]. < http://www.biomedcentral.com/content/pdf/1472-6947-5-34.pdf>. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCord G, Smucker W.D, Selius B.A, Hannan S, Davidson E, Schrop S.L, Rao V, Albrecht P. Answering questions at the point of care: do residents practice EBM or manage information sources. Acad Med. 2007 Mar;82(3):298–303. doi: 10.1097/ACM.0b013e3180307fed. [DOI] [PubMed] [Google Scholar]
- 7. Green M.L, Ciampi M.A, Ellis P.J. Residents' medical information needs in clinic: are they being met. Am J Med. 2000 Aug;109(3):218–23. doi: 10.1016/s0002-9343(00)00458-7. [DOI] [PubMed] [Google Scholar]
- 8. Andrews J.E, Pearce K.A, Ireson C, Love M.M. Information-seeking behaviors of practitioners in a primary care practice-based research network (PBRN) J Med Libr Assoc. 2005 Apr;93(2):206–12. [PMC free article] [PubMed] [Google Scholar]
- 9. Veness M, Rikard-Bell G, Ward J. Views of Australian and New Zealand radiation oncologists and registrars about evidence-based medicine and their access to Internet based sources of evidence. Australas Radiol. 2003, Dec;47(4):409–15. doi: 10.1046/j.1440-1673.2003.01211.x. [DOI] [PubMed] [Google Scholar]
- 10. Callen J.L, Fennell K, McIntosh J.H. Attitudes to, and use of, evidence-based medicine in two Sydney divisions of general practice. Aust J Public Health. 2006;12(1):40–6. [Google Scholar]
- 11. Davies K. The information-seeking behaviour of doctors: a review of the evidence. Health Info Libr J. 2007 Jun;24(2):78–94. doi: 10.1111/j.1471-1842.2007.00713.x. [DOI] [PubMed] [Google Scholar]
- 12.Finley R. SurveyMonkey.com [Internet] Portland, OR: SurveyMonkey; 2010. [cited 8 Jul 2010]. < http://www.surveymonkey.com>. [Google Scholar]
- 13.Davies K. Clinical information needs of doctors in the UK [disseration] Leicestershire, UK: Loughborough University; 2008 Apr. (awarded Dec). [Google Scholar]
- 14.Urbaniak G.C, Plous S.Research randomizer [Internet] 1997. [cited 8 Jul 2010]. < http://www.randomizer.org/form.htm>.
- 15.National Health Service. Evidence in health and social care [Internet] The Service; 2009. [cited 8 Jul 2010]. < http://www.evidence.nhs.uk>. [Google Scholar]
- 16. Honeybourne C, Sutton S, Ward L. Knowledge in the palm of your hands: PDAs in the clinical setting. Health Info Libr J. 2006 Mar;23(1):51–9. doi: 10.1111/j.1471-1842.2006.00621.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.